Procedure 2 Fasciotomy of the Upper Limb
Examination/Imaging
Clinical Examination
 Compartment syndrome is caused by increased pressure within the myofascial compartments leading to a decrease in blood flow. Nerves followed by muscle are most sensitive to ischemia and undergo irreversible changes within 6 to 8 hours. It is therefore important to decompress the fascial compartment by performing a fasciotomy and to restore tissue perfusion as soon as possible.
Compartment syndrome is caused by increased pressure within the myofascial compartments leading to a decrease in blood flow. Nerves followed by muscle are most sensitive to ischemia and undergo irreversible changes within 6 to 8 hours. It is therefore important to decompress the fascial compartment by performing a fasciotomy and to restore tissue perfusion as soon as possible.
 Compartment syndrome is a clinical diagnosis based on the features of ischemia of nerve (paresthesia, pain, and paralysis), muscle (pain on passive stretch), and vessel (pallor and pulselessness). All features may not be present in every patient, and a diagnosis is made based on the overall clinical scenario.
Compartment syndrome is a clinical diagnosis based on the features of ischemia of nerve (paresthesia, pain, and paralysis), muscle (pain on passive stretch), and vessel (pallor and pulselessness). All features may not be present in every patient, and a diagnosis is made based on the overall clinical scenario.
 A prophylactic fasciotomy should be performed in all major limb replantations/revascularizations irrespective of the clinical appearance of the limb at the end of the procedure (Fig. 2-4). The limb is insensate and becomes progressively swollen as a result of diminished venous return and ischemia reperfusion injury. When a fasciotomy is not performed, the arterial inflow can be compromised, leading to failure of the replantation.
A prophylactic fasciotomy should be performed in all major limb replantations/revascularizations irrespective of the clinical appearance of the limb at the end of the procedure (Fig. 2-4). The limb is insensate and becomes progressively swollen as a result of diminished venous return and ischemia reperfusion injury. When a fasciotomy is not performed, the arterial inflow can be compromised, leading to failure of the replantation.
Investigations
 No investigations are required if a diagnosis of compartment syndrome is clinically apparent. Some laboratory studies (complete blood count, prothrombin time, partial thromboplastin time, serum and urine myoglobin, and creatinine phosphokinase) and imaging studies (radiographs, Doppler, and arteriography) can be used to complement the clinical findings.
No investigations are required if a diagnosis of compartment syndrome is clinically apparent. Some laboratory studies (complete blood count, prothrombin time, partial thromboplastin time, serum and urine myoglobin, and creatinine phosphokinase) and imaging studies (radiographs, Doppler, and arteriography) can be used to complement the clinical findings.
 If a clinical diagnosis is equivocal, compartment pressure measurements should be obtained. We use a commercially available device (Stryker Intra-Compartmental Pressure Monitor) (Fig. 2-5). The normal tissue pressure is 0 to 8 mm Hg. A fasciotomy is recommended if the tissue pressure is higher than 30 mm Hg. Close monitoring, repeated clinical examination, and serial measurement of compartment pressures may be required for pressure measurements between 20 and 30 mm Hg.
If a clinical diagnosis is equivocal, compartment pressure measurements should be obtained. We use a commercially available device (Stryker Intra-Compartmental Pressure Monitor) (Fig. 2-5). The normal tissue pressure is 0 to 8 mm Hg. A fasciotomy is recommended if the tissue pressure is higher than 30 mm Hg. Close monitoring, repeated clinical examination, and serial measurement of compartment pressures may be required for pressure measurements between 20 and 30 mm Hg.
Surgical Anatomy
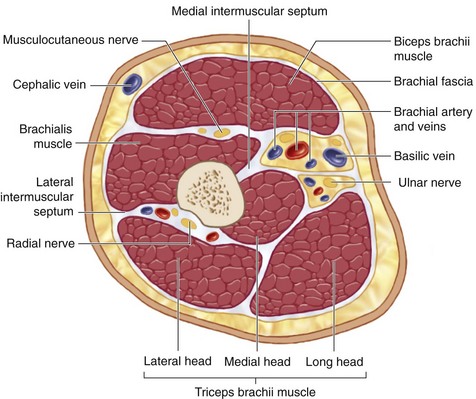
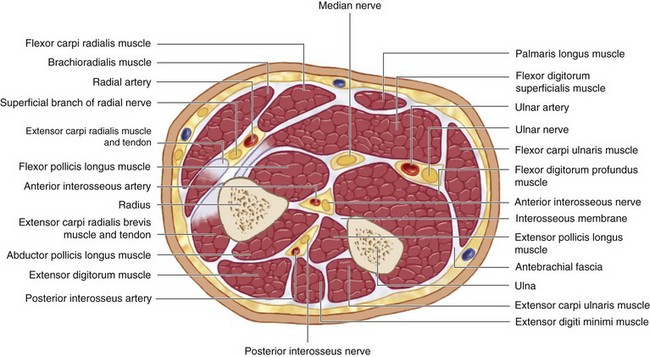
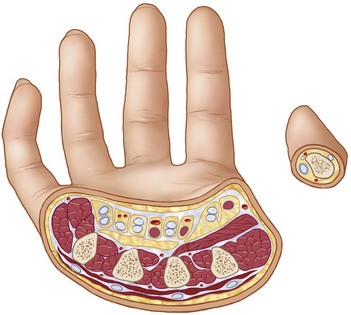
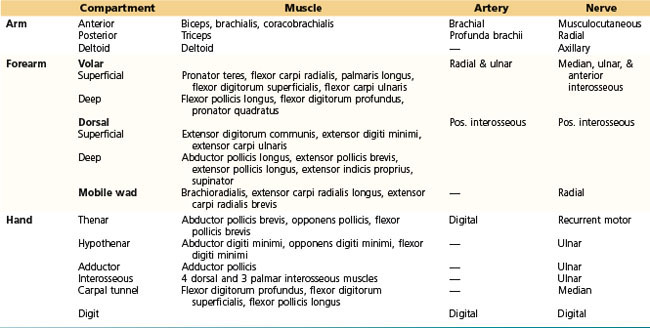
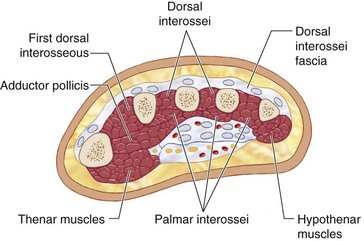
 The myofascial compartments of the upper extremity may be divided into compartments of the arm, forearm, and hand (Figs. 2-6, 2-7, and 2-8). The compartments and their contents are listed in Table 2-1.
The myofascial compartments of the upper extremity may be divided into compartments of the arm, forearm, and hand (Figs. 2-6, 2-7, and 2-8). The compartments and their contents are listed in Table 2-1.
 The brachial fascia of the arm is thin and poorly defined compared with the fascia of the forearm; therefore, development of increased pressure in the arm is less likely. Although a distinct fascial layer has not been defined in the hand, the glabrous skin overlying the thenar and hypothenar muscle compartments is relatively unyielding and serves as a constricting layer.
The brachial fascia of the arm is thin and poorly defined compared with the fascia of the forearm; therefore, development of increased pressure in the arm is less likely. Although a distinct fascial layer has not been defined in the hand, the glabrous skin overlying the thenar and hypothenar muscle compartments is relatively unyielding and serves as a constricting layer.
Positioning
 The procedure is performed under tourniquet control and regional or general anesthesia. The patient is positioned supine with the affected extremity on a hand table. A fasciotomy is usually done at the end of major limb replantation, and a tourniquet is not used in this situation. An emergency escharotomy may be done at the bedside for a circumferential third-degree burn because such a burn is not painful.
The procedure is performed under tourniquet control and regional or general anesthesia. The patient is positioned supine with the affected extremity on a hand table. A fasciotomy is usually done at the end of major limb replantation, and a tourniquet is not used in this situation. An emergency escharotomy may be done at the bedside for a circumferential third-degree burn because such a burn is not painful.
Exposures
Hand
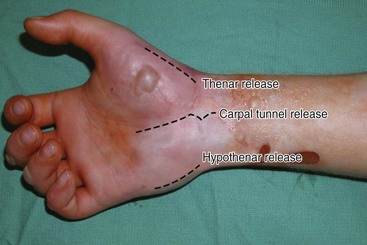
 The carpal tunnel is decompressed by a single incision between the thenar and hypothenar muscles in line with the third web space (Fig. 2-9).
The carpal tunnel is decompressed by a single incision between the thenar and hypothenar muscles in line with the third web space (Fig. 2-9).
 The thenar compartment is decompressed by an oblique longitudinal incision along the radial margin of the thenar eminence (see Fig. 2-9).
The thenar compartment is decompressed by an oblique longitudinal incision along the radial margin of the thenar eminence (see Fig. 2-9).
 The hypothenar compartment is released via a longitudinal incision along the ulnar aspect of the palm (see Fig. 2-9).
The hypothenar compartment is released via a longitudinal incision along the ulnar aspect of the palm (see Fig. 2-9).
 The dorsal compartments are released by two longitudinal incisions parallel to the radial border of the index and ring metacarpals (Fig. 2-10).
The dorsal compartments are released by two longitudinal incisions parallel to the radial border of the index and ring metacarpals (Fig. 2-10).
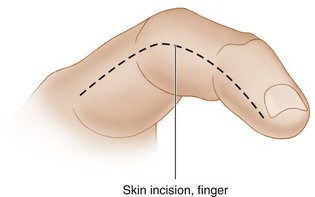
 Finger decompression is done by a midaxial incision on the noncontact side of the fingers (ulnar side of index and long finger and radial side of thumb, ring, and small fingers) (Fig. 2-11).
Finger decompression is done by a midaxial incision on the noncontact side of the fingers (ulnar side of index and long finger and radial side of thumb, ring, and small fingers) (Fig. 2-11).
Forearm
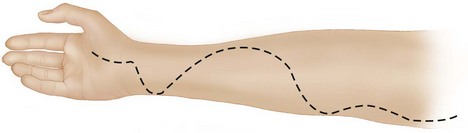
 The standard incision for release of the forearm is a curvilinear incision extending from the medial epicondyle to the proximal wrist crease. It is important to curve this incision over the distal forearm so that a flap of skin can cover the median nerve and the flexor carpi radialis (FCR) tendon (Fig. 2-12).
The standard incision for release of the forearm is a curvilinear incision extending from the medial epicondyle to the proximal wrist crease. It is important to curve this incision over the distal forearm so that a flap of skin can cover the median nerve and the flexor carpi radialis (FCR) tendon (Fig. 2-12).
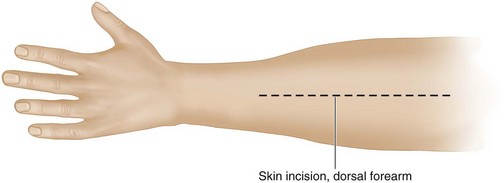
 A 10- to 15-cm dorsal longitudinal incision beginning 3 to 4 cm distal to the lateral epicondyle toward the Lister tubercle can decompress the dorsal compartment and the mobile wad of muscles (Fig. 2-13). We prefer to use two parallel longitudinal incisions instead of the standard incision.
A 10- to 15-cm dorsal longitudinal incision beginning 3 to 4 cm distal to the lateral epicondyle toward the Lister tubercle can decompress the dorsal compartment and the mobile wad of muscles (Fig. 2-13). We prefer to use two parallel longitudinal incisions instead of the standard incision.
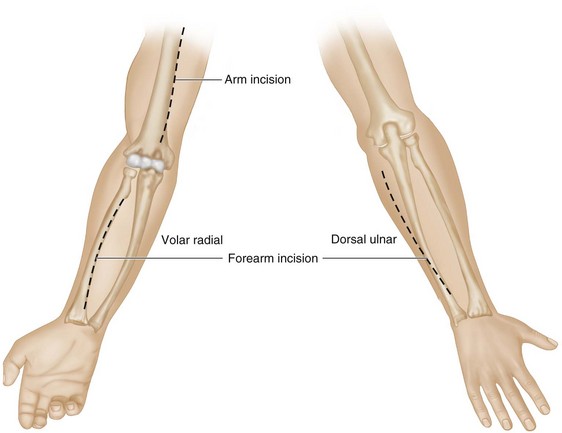
 One incision is made over the volar radial aspect of the forearm overlying the flexor muscles, and the other is made over the dorsal ulnar aspect over the extensor muscles. This double incision allows decompression of the volar and dorsal compartments and does not expose the median nerve or the tendons at the distal forearm (Fig. 2-14).
One incision is made over the volar radial aspect of the forearm overlying the flexor muscles, and the other is made over the dorsal ulnar aspect over the extensor muscles. This double incision allows decompression of the volar and dorsal compartments and does not expose the median nerve or the tendons at the distal forearm (Fig. 2-14).
Arm
 A medial incision extending from the anterior axillary line to the medial epicondyle can access the anterior and posterior compartments (see Fig. 2-14). The medial incisions can also be used for exposure of the major neurovascular structures in the arm.
A medial incision extending from the anterior axillary line to the medial epicondyle can access the anterior and posterior compartments (see Fig. 2-14). The medial incisions can also be used for exposure of the major neurovascular structures in the arm.
 A separate incision over the midportion of the deltoid may be required in rare situations.
A separate incision over the midportion of the deltoid may be required in rare situations.
Pearls
One should aim to preserve the cutaneous nerves and veins whenever possible.
The incision for release of the hypothenar compartment should not be over the ulnar border of the hand, but slightly radial to prevent pressure over the scar when the hand is rested (see Fig. 2-9).
When dorsal and volar forearm compartments are involved, it is preferable to release the volar compartment first because the relaxation afforded by the skin and fascia often decompresses the dorsal compartment at the same time.
Procedure
Fasciotomy of the Hand
Step 1: Carpal Tunnel Release
 The incision is deepened, and the palmar aponeurosis is identified. The fibers of the palmar aponeurosis are split longitudinally to expose the transverse carpal ligament (TCL). The distal free edge of the TCL is identified, and the ligament is divided from distal to proximal taking care to protect the median nerve (Fig. 2-15).
The incision is deepened, and the palmar aponeurosis is identified. The fibers of the palmar aponeurosis are split longitudinally to expose the transverse carpal ligament (TCL). The distal free edge of the TCL is identified, and the ligament is divided from distal to proximal taking care to protect the median nerve (Fig. 2-15).
Step 1 Pearls
It is important to do the carpal tunnel release through a regular extensile incision that extends to the proximal wrist crease. The limited carpal tunnel release incision used in carpal tunnel syndrome should not be used in this situation because the exposure is poor and fascial release may be inadequate.
Step 3: Hypothenar Decompression
Step 4: Decompression of the Dorsal Compartment
 The incision along the radial border of the index metacarpal is used to decompress the first dorsal interosseous and the adductor pollicis (Figs. 2-16 and 2-17). The second dorsal interosseous (between the index and long metacarpals) is also approached via the same incision (see Fig. 2-17).
The incision along the radial border of the index metacarpal is used to decompress the first dorsal interosseous and the adductor pollicis (Figs. 2-16 and 2-17). The second dorsal interosseous (between the index and long metacarpals) is also approached via the same incision (see Fig. 2-17).
 The incision along the radial border of the ring metacarpal is used to decompress the third and fourth dorsal interossei (see Fig. 2-17).
The incision along the radial border of the ring metacarpal is used to decompress the third and fourth dorsal interossei (see Fig. 2-17).
Procedure
Fasciotomy of the Forearm
Step 1: Volar Forearm Release
 The incision is deepened, and the deep fascia of the forearm is divided (Fig. 2-18).
The incision is deepened, and the deep fascia of the forearm is divided (Fig. 2-18).
 The deep flexor muscles (pronator quadratus, flexor pollicis longus, and flexor digitorum profundus) may also need to be decompressed. They can be approached by dissecting between the FCR and the palmaris longus (PL).
The deep flexor muscles (pronator quadratus, flexor pollicis longus, and flexor digitorum profundus) may also need to be decompressed. They can be approached by dissecting between the FCR and the palmaris longus (PL).
Step 1 Pearls
If the muscles appear pale, it may be necessary to incise the epimysium to further decompress individual muscles.
It is better to approach the deep muscles after identifying the median nerve and staying ulnar to the median nerve to protect the palmar cutaneous branch of the median nerve. This branch arises from the radial aspect of the median nerve and travels on the ulnar side of the FCR.
Step 2: Dorsal Forearm Release
Step 3: Two-Incision Release of Forearm
Step 4
 The tourniquet is released and hemostasis secured.
The tourniquet is released and hemostasis secured.
 Any secondary procedures, such as débridement of nonviable muscles and arterial reconstruction, should be done.
Any secondary procedures, such as débridement of nonviable muscles and arterial reconstruction, should be done.
 One or two tagging sutures may be placed in the distal volar forearm to cover the median nerve and the FCR.
One or two tagging sutures may be placed in the distal volar forearm to cover the median nerve and the FCR.
 A bulky dressing is applied, and a splint in functional position is provided.
A bulky dressing is applied, and a splint in functional position is provided.
Procedure
Postoperative Care and Expected Outcomes
 The limb should be elevated to decrease swelling and encourage venous return.
The limb should be elevated to decrease swelling and encourage venous return.
 The wound should be reexamined within 24 hours, and, if required, additional débridement is done.
The wound should be reexamined within 24 hours, and, if required, additional débridement is done.
 Wound closure should be planned within 3 to 5 days. Waiting longer makes closure difficult and increases the risk for secondary bacterial colonization. A skin graft may be required occasionally.
Wound closure should be planned within 3 to 5 days. Waiting longer makes closure difficult and increases the risk for secondary bacterial colonization. A skin graft may be required occasionally.
 The outcome of fasciotomy depends on how early it is performed. There is usually no morbidity if it is done within 3 to 4 hours. If it is delayed, however, there may be irreversible nerve and muscle injury that will require secondary reconstructive surgery.
The outcome of fasciotomy depends on how early it is performed. There is usually no morbidity if it is done within 3 to 4 hours. If it is delayed, however, there may be irreversible nerve and muscle injury that will require secondary reconstructive surgery.
Bae DS, Kadiyala RK, Waters PM. Acute compartment syndrome in children: contemporary diagnosis, treatment, and outcome. J Pediatr Orthop. 2001;21:680-688.
Ouellette EA, Kelly R. Compartment syndromes of the hand. J Bone Joint Surg [Am]. 1996;78:1515-1522.
Ragland RIII, Moukoko D, Ezaki M, et al. Forearm compartment syndrome in the newborn: report of 24 cases. J Hand Surg [Am]. 2005;30:997-1003.