CHAPTER 2 Dynamic Pathophysiology of Acupoints
INTRODUCTION
Acupoints in different parts of the human body have different anatomic characteristics. All acupoints, however, have one element in common: they are able to become sensitive, tender, or even painful when exposed to a pathologic disorder. The process of sensitizing is still a puzzle to scientists and clinicians. Recent research data and clinical observations related to muscle pain1 help to explain more clearly some of the characteristics of acupoints.
It is important to clarify confusion regarding the differences between acupoints and trigger points.
DYNAMIC PHASES OF ACUPOINTS
Dr. H.C. Dung described three phases of acupoints: latent, passive, and active.3 Generally in healthy people some acupoints are neither sensitive nor tender. These nonsensitive acupoints are referred to as latent acupoints.
Latent acupoints represent normal tissues. Neurologically passive acupoints have a lower mechanical threshold than normal tissues do and start to fire impulses to the spinal cord and brain under normal mechanical pressure. The same amount of pressure will not induce impulses on latent points. Active acupoints have the lowest mechanical threshold; they may continuously fire impulses to the brain, even without being submitted to external mechanical pressure, and may finally sensitize the neurons in the spinal cord and brain. As the mechanical threshold decreases, the physical size of a sensitized acupoint increases. The phase transition from latent to passive or from passive to active is a continuous process without any clear demarcation; so there is no quantitative measurement for differentiating acupoints of different phases. Table 2-1 provides some criteria, based on our clinical experience, to differentiate the three phases of acupoints. The pressure used to palpate the acupoints is about 2 or 3 pounds. In the clinic we use the thumb to press the points. The pressure is about 2 or 3 pounds when the thumbnail turns from pinkish to whitish. The pressure used to palpate may need to be adjusted because some patients tolerate less pressure if their acupoints are very sensitive or even painful.
| Physiologic Phase | Physiologic Feature | Physical Features (Size) |
|---|---|---|
| Latent | Nonsensitive | Normal tissue |
| Passive | Sensitive on palpation | Diameter <2 cm |
| Active | Painful without palpation | Diameter usually >2 cm |
Clinical cases show that there are direct and indirect events that stimulate or activate the transition of acupoints from latent to passive and from passive to active phases. Acute injuries, overuse fatigues, repetitive motions, compression of nerves such as radiculopathy, and joint dysfunctions such as arthritis directly turn the local (symptomatic) acupoints tender. Chronic disorders, fever, cold, visceral diseases (such as those of the heart, lung, gallbladder, stomach), and emotional distress indirectly sensitize both homeostatic (systemic) and symptomatic (local) acupoints. In the latter cases, the tender symptomatic acupoints often appear neurosegmentally related to the disturbed organs, possibly through neural viscerocutaneous reflex.
PHYSICAL PROPERTIES OF ACUPOINTS
Physical properties of acupoints refer to the physical representation of acupoints on the body surface in terms of quality (sensitivity) and quantity (size of each tender acupoint and total number of tender acupoints in the body). Physical properties of acupoints include three parameters: sensitivity, specificity, and sequence.3 These physical properties of acupoints indicate the severity or chronicity of pain symptoms.
Specificity
Specificity refers to the size and precise location of a passive acupoint. In the beginning of the passive phase, the area or surface size of a tender acupoint is relatively small, about 0.5 cm (1/5 inch) in diameter, and difficult to locate. This means the sensitized acupoint is related only to a limited tissue structure and restricted to a particular anatomic location. This condition is referred to as higher specificity. When symptoms become more severe, the sensitivity of the acupoint spreads to surrounding tissues, and consequently the surface size of the acupoint grows. The surface size of the acupoint may grow by up to or even more than 3 to 4 cm (1.5 inches) in diameter, and the acupoint becomes more easily palpable. This condition is referred to as lower specificity. Some practitioners4 found that careful palpation reveals large, tender regions varying from 16 to 200 cm2 (about 1.5 to 5 inches in diameter) surrounding a tender point.
Sequence
Acupoints appear in the human body according to two models: systemic or symptomatic.3 A physically healthy person always has from a few to about 20 passive acupoints in the body. More passive acupoints will appear symmetrically all over the body when the healthy person gradually develops chronic problems, such as chronic diseases, and degenerative problems related to age, poor diet, bad posture, lack of exercise, or persisting physical or emotional stress. This phenomenon is referred to as the systemic model of acupoint formation, which indicates that passive acupoints appear all over the body systemically when homeostasis declines. Most important, in the systemic model all passive acupoints are formed in predictable locations and in a predictable sequence. The predictable sequence shows which acupoint becomes sensitive first and which acupoint will be sensitized next. This predictability in all people, healthy or sick, provides a quantitative basis for evaluation of a patient’s health status and allows the development of a standardized treatment protocol for acupuncture therapy aimed to restore homeostasis (see Chapter 6). We call these predictable acupoints homeostatic acupoints because they are related to homeostatic decline. Once homeostasis is restored, some HAs are gradually desensitized and eventually the tenderness disappears.
In physically healthy bodies HAs are transformed from latent phase into passive phase following a highly predictable pattern. For example, the H1 deep radial acupoint (located on the deep radial nerve where the nerve enters the lateral side of the forearm to supply the extensor muscles of the wrist and fingers) is always first to become tender in everyone (refer to the figure on the inside cover).
The number of tender HAs in the body serves as a quantitative indicator of the patient’s health status. Usually a healthier person has less tender acupoints in his or her body. If a healthy person has acute pain, a few acupuncture sessions will relieve the pain. Less healthy people have more tender acupoints, and such patients will need more acupuncture sessions to achieve relief of even minor acute pain. Thus the number of tender HAs in the body is the quantitative indicator of (1) health status, (2) self-healing capacity (healthy persons heal better and faster), and (3) the number of acupuncture treatments that may be needed to achieve pain relief. This quantitative indicator provides us with a reasonably objective method to evaluate patients and to predict the prognosis of treatments (see Chapter 6).
ELECTROPHYSIOLOGY OF ACUPOINTS
Muscles and nerves are excitable tissues that generate electrical signals when stimulated. When not disturbed, that is, in the so-called healthy state, muscles and nerves are electrically silent at rest. Dr. David G. Simmons and his colleagues investigated the electrical activity in trigger points.1 They found two significant components of electrical activity in trigger points:
ACUPUNCTURE NEEDLING RESTORES NORMAL ENERGY METABOLISM OF ACUPOINTS
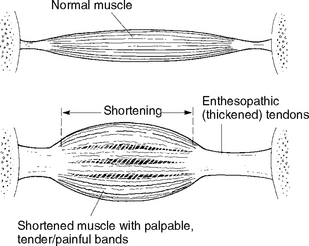
Dr. David G. Simmons has shown that muscular contraction knots are the histopathologic characteristics of trigger points.5 Dr. C. Chan Gunn also suggests a similar histologic structure of the shortened muscles with palpable tender or painful bands or points (Figure 2-1).
In 1950 medical scientist Y. Nakatani (see Chapter 1) from Japan’s Kyoto University discovered that acupoints on the skin have a high level of electrical conductivity. Moreover the electrical conductivity of some acupoints increased significantly during sickness. He found 370 such points, incorporated them into the classic meridians system, and called these acupoints Ryodoraku points,6 which in both Japanese and Chinese languages means meridian point with good electrical conductivity.
In 1977 Nakatami noted that Ryodoraku points were situated on areas containing sweat glands and inferred that the higher electrical conductivity of Ryodoraku is due to the high electrical conductivity of the sweat glands. Modern Ryodoraku theory focuses on interactions between the sympathetic and somatic nervous systems.6 There is no doubt that abnormal energy metabolism is actively involved in the formation of passive and active acupoints related to soft tissue metabolism, as discussed below.
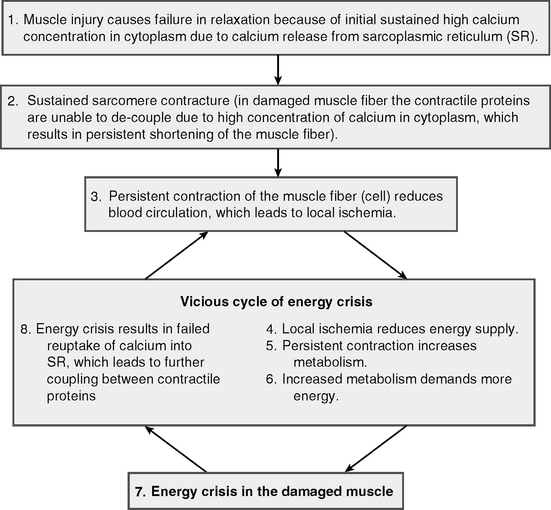
The sustained contraction significantly increases the demand for energy and leads to “energy crises.” Sustained muscle contraction shuts the capillary network that supplies the region with nutrition and oxygen and therefore generates a low-oxygen environment (hypoxia). Without energy and oxygen, the cellular machine cannot pump calcium from cytoplasm back to its storage pool (SR), which results in sustained high calcium concentration in the cytoplasm and the consequent persistent sustained muscle contraction. Thus the vicious cycle is built and perpetuated (Figure 2-2).
If a muscle fiber is damaged, SR is unable to reuptake the cytoplasmic calcium back for storage, which creates a persistent high concentration of cytoplasmic calcium. The two contractile protein molecules cannot decouple because of this high concentration of cytoplasmic calcium. This results in persistent contraction of the muscle fiber, even without any impulse from the motor nerve. If this energy-consuming process (the energy crisis) continues, tender muscle bands or acupoints will be formed and the tender bands will become a permanent contracture if the energy crisis persists a long time. Finally, this energy crisis may cause chronic inflammation in the involved soft tissues. Both energy crisis and inflammation increase the local temperature.
The needled lesion disturbs the surrounding tissue and generates a small electrical current of up to 500 mA/cm,7 which we call the lesion current. The needle lesion causes a tiny local bleeding, which stimulates secretion of numerous growth factors, such as platelet-derived growth factors and neurotrophic factors.
The electrical current generated by the lesion and the bleeding caused by needling promote healing and regeneration of damaged tissues and induce DNA synthesis of new proteins and collagens, which repair damaged cellular organelles and restore normal functions. A needle-induced lesion may last at least 2 days or longer before the body heals it, which means that lesion-induced stimulation may last as long. During the healing period, the lesioned cells are digested and replaced by the same types of tissue cells. This explains why acupuncture needling can achieve longer-lasting results. After the needles are removed, the needle-induced lesions keep working for at least 48 hours.
Another important feature is that needling and needle-induced lesions also trigger the local and systemic immune and antiinflammatory reaction that controls the inflammation in the area of needle-induced lesions (see Chapter 4). This explains the antiinflammatory function of acupuncture therapy.
1 Mens S, Simons DG. Muscle pain. Philadelphia: Lippincott–Williams & Wilkins, 2001.
2 Kellgren HJ. The distribution of pain arising from deep somatic structures with charts of segmental pain areas. Clin Sci. 1939;4:35-46.
3 Dung HC. Anatomical acupuncture. San Antonio: Antarctic Press, 1997.
4 Macdonald AJR. Acupuncture’s non-segmental and segmental analgesic effects: the point of meridians. In: Filshie J, White A, editors. Medical acupuncture. Edinburgh: Churchill Livingston, 1998.
5 Simons DG, Travell JG, Simons LS. Travell & Simons’ myofascial pain and dysfunction: the trigger point manual, vol 1, Upper half of body. Philadelphia: Lippincott–Williams & Wilkins, 1999.
6 Nakatani Y, Yamashita K. Ryodoraku acupuncture. Osaka: Ryodoraku Research Institute, 1977.
7 Jaffe LF. Extracellular current measurements with a vibrating probe. TINS. 1985;December:517-521.