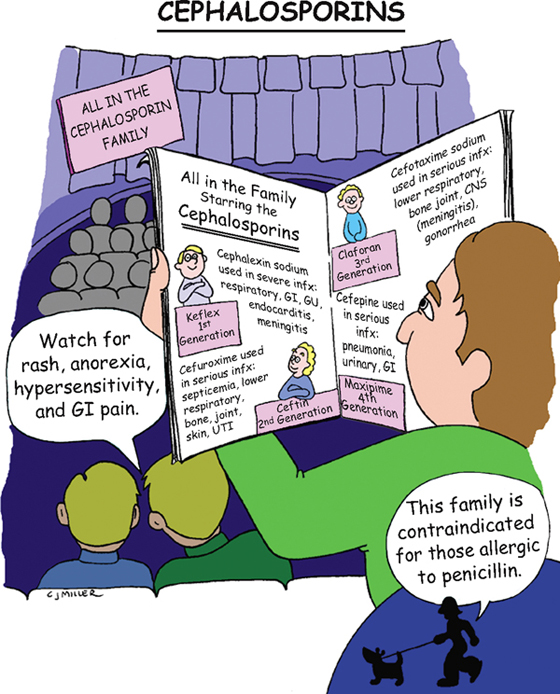
Cephalosporins
ACTION
Each generation has increasing bactericidal activity to break down gram-negative bacteria and anaerobes, as well as reach the cerebrospinal fluid. Cephalosporins interfere with bacterial cell wall synthesis and are considered broad-spectrum. The cell weakens, swells, bursts, and dies as a result of increased osmotic pressure inside the cell.
USES
• Is used widely in a variety of infections.
CONTRAINDICATIONS
• Because of cross-sensitivity, patients with allergies to penicillins
SIDE EFFECTS
• †Hypersensitivity reactions:† **rash, pruritus, fever**
• Anorexia, **nausea,** flatulence, **vomiting, diarrhea**
• Third-generation medications: †possible suprainfection†
NURSING IMPLICATIONS
1. Evaluate intramuscular (IM) and intravenous (IV) sites for reaction, such as abscess and thrombophlebitis. Minimize complication of thrombophlebitis by rotating injection sites and slowly injecting in a dilute solution.
2. *Monitor rate of infusion; check labeling for rate of IV infusion.*
3. *Monitor renal and hepatic studies throughout therapy.*
4. ‡Advise patient to hydrate; notify health care provider if patient is experiencing diarrhea.‡
5. With medications that cause bleeding tendencies, monitor for bleeding.
6. *If gastrointestinal (GI) upset occurs, patient can take medication with food.*
7. ‡Teach patient to refrigerate oral suspensions.‡
8. IM injections are frequently painful; forewarn patient.
9. Instruct patient to report any signs of allergy (e.g., skin rash, itching, hives).
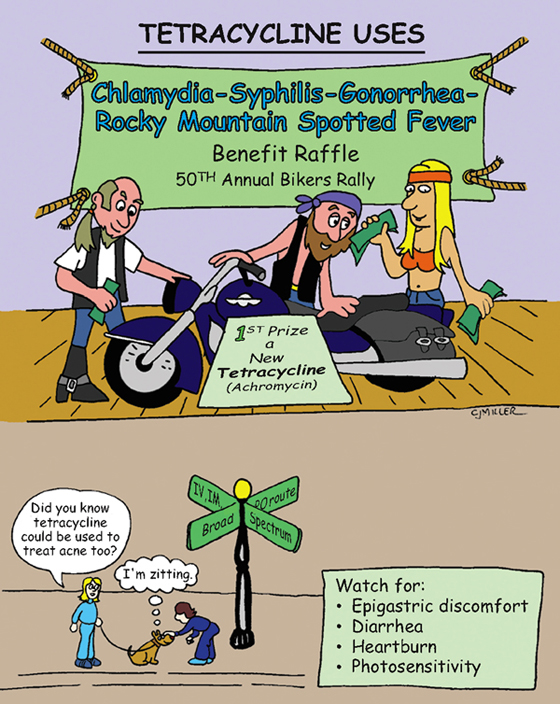
Tetracyclines
CLASSIFICATION
Antibiotic
ACTION
Tetracyclines are bacteriostatic, broad-spectrum antibiotics that suppress bacterial growth and replication but do not kill the bacterial cells outright. These antibiotics are considered second-line drug agents used for infections resistant to first-line drugs by passive diffusion and active transport, competing for binding at subunit sites of RNA ribosome interfering with the bacteria’s ability to function and reproduce. This antibiotic is a bactericidal in large doses.
USES
• Rickettsial diseases (Rocky Mountain spotted fever, typhus)
• Chlamydia infections, peptic ulcer disease (Helicobacter pylori infection)
• Acne, Mycoplasma pneumoniae, Lyme disease, periodontal disease
PRECAUTIONS
• May result in renal and hepatic dysfunction.
• *Do not give to children (<8 yr) or pregnant women.*
• *May cause staining of developing teeth.*
SIDE EFFECTS
• **Nausea,** abdominal cramping, vomiting, diarrhea, †suprainfection,† **photosensitivity**
NURSING IMPLICATIONS
1. ‡Take on an empty stomach; antacids, milk products, and iron supplements should not be consumed until at least 2 hours after dose was taken.‡
2. *Do not administer to pregnant women or children under age 8 years to avoid tooth discoloration.*
3. †Monitor carefully for diarrhea because diarrhea may indicate a suprainfection of bowel (Clostridium difficile).†
4. Check dose and rate when delivering intravenously.
5. ‡Wear sunscreen and protective clothing.‡
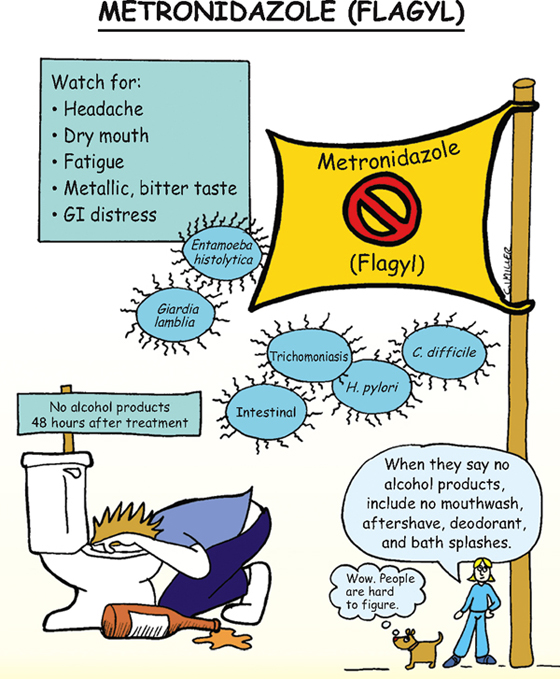
Metronidazole (Flagyl)
CLASSIFICATION
Antibacterial
ACTION
Direct trichomonacidal and amebicidal activity against Trichomonas vaginalis, Entamoeba histolytica, Clostridium difficile, and Giardia lamblia. Antibacterial activity against anaerobic bacteria, gram-negative anaerobic bacilli, and clostridia.
USES
• Asymptomatic and symptomatic trichomoniasis in female and male patients
• Acute intestinal amebiasis, giardiasis, and antibiotic-associated colitis
CONTRAINDICATIONS
• Active central nervous system (CNS) disease, blood dyscrasias
• First-trimester pregnancy, breast-feeding mothers
PRECAUTIONS
• Second- and third-trimester pregnancies
SIDE EFFECTS
• **Nausea, headache, dry mouth,** vomiting, anorexia, epigastric distress
• **Metallic taste,** darkening of the urine, seizures
NURSING IMPLICATIONS
1. Take on an empty stomach if possible; may take with food if nauseated.
2. ‡Teach not to apply cologne, aftershave lotion, or bath splashes or ingest alcohol products to avoid a disulfiram-type reaction (e.g., flushing, nausea and vomiting, palpitations, tachycardia, psychosis).‡
3. ‡Mothers should wait until 3 days after last dose of drug to resume breast-feeding.‡
4. ‡Teach patient that harmless darkening of the urine may occur.‡
Isoniazid (INH)
CLASSIFICATION
Antituberculosis agent
ACTIONS
Bacteriostatic to “resting organisms” and bactericidal to actively dividing organisms. Interferes with biosynthesis of bacterial protein, nucleic acid, and lipids.
USES
• Treatment of all forms of active tuberculosis
CONTRAINDICATIONS AND PRECAUTIONS
• History of isoniazid-associated hypersensitivity reaction
• Convulsive disorders or alcoholism
SIDE EFFECTS
• **Peripheral neuropathy,** clumsiness, unsteadiness, muscle ache
• Epigastric distress, jaundice, †drug-induced hepatitis†
NURSING IMPLICATIONS
1. ‡Teach patient to take orally on an empty stomach 1 hour before or 2 hours after meals.‡
2. *Depletes vitamin B6 (pyridoxine) and will need supplementation during treatment.*
3. *Peripheral neuritis, the most common adverse effect, is preceded by paresthesias (e.g., numbness, tingling, burning, pain) of the feet and hands.*
4. ‡Teach patients to reduce or eliminate consumption of alcohol to reduce risk of hepatotoxicity.‡
5. *Antituberculosis treatment always involves two or more medications;* INH is often combined with rifampin.
Remember this mnemonic for antibiotics used in TB: STRIPE
ST—streptomycin R—rifampin I—isoniazid P—pyrazinamide E—ethambutol
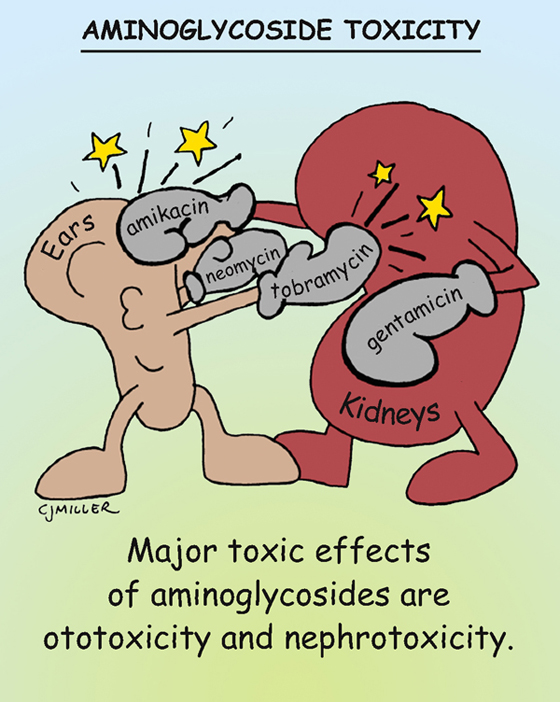
Aminoglycosides
ACTION
Bactericidal against a wide variety of gram-negative bacteria (narrow-spectrum) and certain gram-positive organisms. Disrupts bacterial protein synthesis.
USES
• Parenteral use restricted to treatment of serious infection of the gastrointestinal, respiratory, and urinary tracts; central nervous system (CNS); bone; skin and soft tissue, including burns
• Topically—primary and secondary skin infection
CONTRAINDICATION
• History of hypersensitivity or toxic reaction with aminoglycoside antibiotics
PRECAUTIONS
• Patients who have renal impairment
• History of eighth cranial nerve impairment
• Patients with myasthenia gravis
• Possible fetal damage when given to pregnant and lactating women
SIDE EFFECTS
• **Nephrotoxicity** (reversible injury) and **ototoxicity** (irreversible injury)
• †Neuromuscular blockade leading to flaccid paralysis and fatal respiratory depression that can occur in patients receiving skeletal muscle relaxants†
NURSING IMPLICATIONS
1. Peak and trough levels should be assessed. Ototoxicity is associated with persistent high trough levels, rather than high peak levels.
2. *Monitor renal function (e.g., blood urea nitrogen, creatinine levels).*
3. *Monitor for sensory problems (e.g., loss of hearing).* ‡Instruct patients to report tinnitus, high-frequency hearing loss, persistent headache, nausea, dizziness, vertigo.‡
4. *Anticipate antidote of intravenous (IV) calcium gluconate for treatment of neuromuscular blockade.*
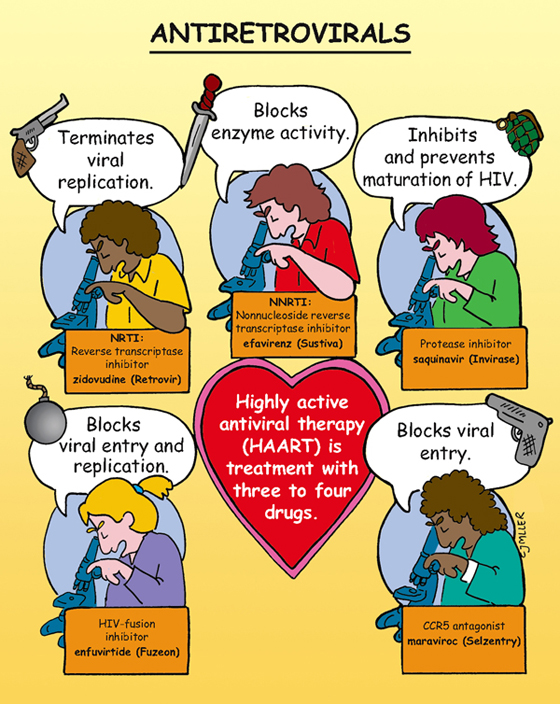
Antiretrovirals
ACTIONS
• Nucleoside/nucleotide reverse transcriptase inhibitors (NRTI)—inhibit human immunodeficiency viral (HIV) replication
• Nonnucleoside reverse transcriptase inhibitors (NNRTI)—disrupt enzyme activity
• Protease inhibitor (PI)—inhibits and prevents maturation of virus
• HIV fusion inhibitor—blocks entry of virus into CD4-T cells
• CCR5 antagonist—blocks viral entry; some strains of HIV require CCR5
CONTRAINDICATIONS AND PRECAUTIONS
• Hypersensitivity and hemophilia
SIDE EFFECTS
• NRTI: anemia, neutropenia, gastrointestinal (GI) upset; rarely lactic acidosis and hepatic steatosis (fatty liver)
• NNRTI: **central nervous system (CNS) symptoms** (dizziness, insomnia, drowsiness), **rash** may range from mild to severe; check liver function studies
• PI: **hyperglycemia,** fat maldistribution (pseudo-Cushing syndrome), hyperlipidemia, bone loss, elevation serum transaminases (liver injury)
• HIV-fusion inhibitor: **injection site reactions,** pneumonia, hypersensitivity
• CCR5 antagonist: **cough, dizziness,** pyrexia, abdominal pain
NURSING IMPLICATIONS
1. Check to see whether medication should be taken with or without food because this varies with drug classes.
2. ‡Instruct patient to take the full dose and complete treatment regimen.‡
3. *Pregnant woman should receive antiretroviral therapy regardless of pregnancy status.*
4. ‡Teach patient to report symptoms related to severe rash, CNS issues, diabetes, pneumonia.‡
Remember, vir at the start, middle, or end of a word means virus: acyclovir, efavirenz, enfuvirtide, Retrovir, saquinavir (Invirase), maraviroc.
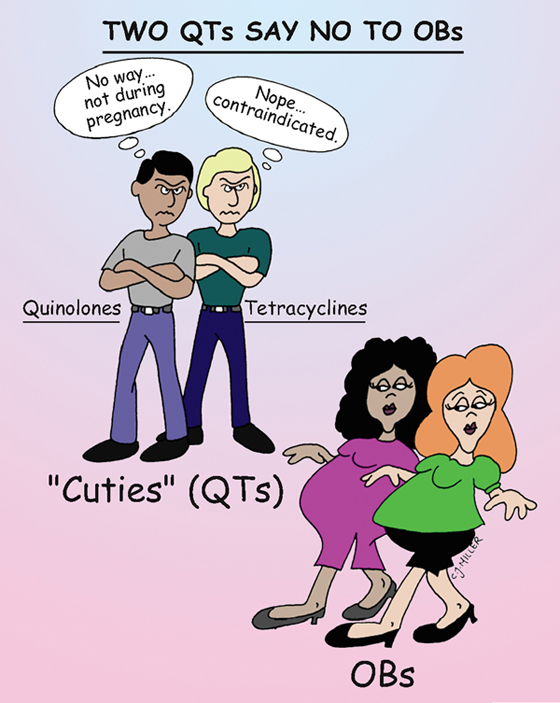
Drug Impact on Pregnancies
FDA PREGNANCY RISK CATEGORIES
• Category A: Remote risk of fetal harm
• Category B: Slightly more risk than category A
• Category C: Greater risk than category B
• Category D: Proven risk of fetal harm; labeled as warning
• Category X: Proven risk of fetal harm; labeled as contraindicated
CONTRAINDICATIONS
• *Women who are pregnant need to take a cautious approach to drug therapy during pregnancy.* The health care provider is responsible for ordering medications that are safe and appropriate for the ever-changing physiologic dynamics during pregnancy.
• Quinolones (category C) and tetracyclines (category D) are not routinely used during pregnancy.
NURSING IMPLICATIONS
1. Evaluate patient’s level of understanding about her physiologic, mental, and emotional conditions.
2. ‡Teach patient to call the prenatal clinic or physician’s office before using any over-the-counter medications.‡
4. ‡Advise patient to avoid all alcoholic beverages during the term of the pregnancy.‡
5. Advise patient to report any unusual signs or symptoms of reactions to the treatment plan.
Think of the mnemonic MCAT to remember other antibiotics contraindicated in pregnancy. M—Metronidazole (contraindicated in first trimester; category B—second and third trimesters); C—Chloramphenicol (category C); A—Aminoglycoside (category C): T—Tetracycline (category D)
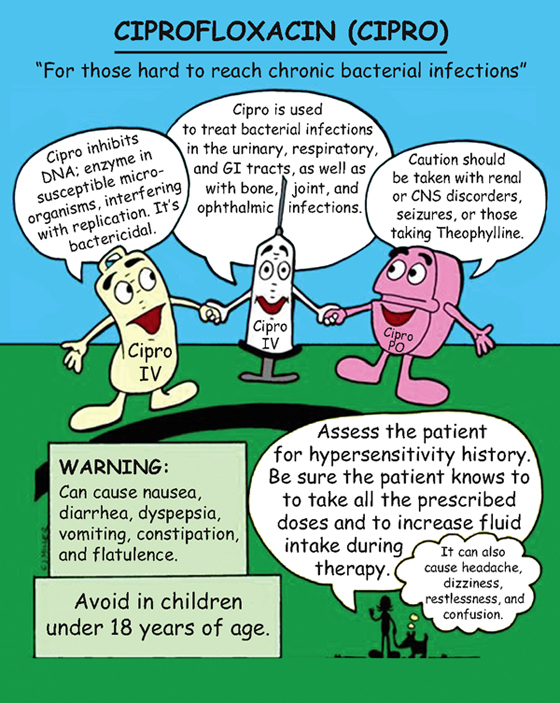
Ciprofloxacin (Cipro)
ACTIONS
Bactericidal inhibits DNA enzyme that interferes with replication; is considered broad spectrum. Is not useful against anaerobic infections.
USES
• Respiratory, urinary, gastrointestinal (GI), bone, joint, skin, and soft-tissue infections
• Preferred drug for treatment of inhaled anthrax
CONTRAINDICATIONS AND PRECAUTIONS
• Children under age 18 years (systemic treatment should be avoided)
SIDE EFFECTS
• **GI upset—nausea, vomiting, diarrhea, abdominal pain**
• **Dizziness, headache, restlessness**
• In older adult—significant risk of confusion, somnolence, psychosis, visual disturbances
• Tendon rupture, †seizures† (rarely)
NURSING IMPLICATIONS
1. ‡Teach patient to avoid antacids, iron supplements, and milk and dairy products for at least 2 hours after taking medication.‡
2. ‡Teach patient to report any tendon pain or inflammation.‡
3. Encourage adequate fluid intake, 6 to 8 glasses daily.
4. *Administer intravenous (IV) Cipro over 60 minutes.*
5. *Dosage regimen for anthrax inhalation is over a 60-day period.*
6. ‡Teach patient to wear sunscreen and protective clothing when in sunlight.‡
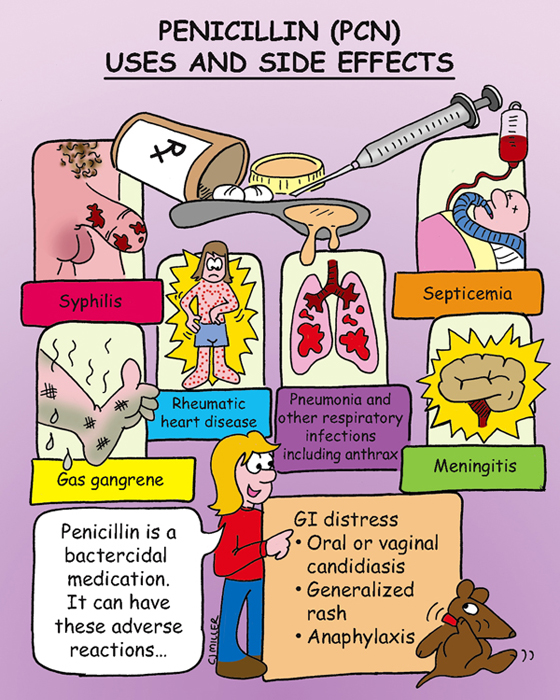
Penicillin
ACTION
Bactericidal disrupts and weakens the cell wall, leading to cell lysis and death.
USE
Based on type of penicillin, treatment of infections caused by bacteria
TYPES
• Narrow spectrum that are penicillinase sensitive—penicillin G (Bicillin, Wycillin), penicillin V (Veetids)
• Penicillinase-resistant (antistaphylococcal penicillins)—nafcillin, oxacillin, dicloxacillin
CONTRAINDICATIONS AND PRECAUTIONS
• Hypersensitivity to penicillin, cephalosporins, or carbapenems
SIDE EFFECTS
• Allergic response (all types)—**rash, itching, hives,** †anaphylaxis†
NURSING IMPLICATIONS
1. ‡Instruct patient to check label with regard to administering with food.‡
2. ‡Instruct patient to wear medication-alert bracelet if allergic to penicillin.‡
3. Monitor renal, cardiac function and, electrolyte levels to avoid toxic levels.
4. *Monitor patient for 30 minutes when given parenterally; administer epinephrine if anaphylaxis occurs.*
5. *Collect any laboratory culture specimens before initiating penicillin therapy.*
7. *Monitor for circulatory overload and bleeding tendencies when patient receives ticarcillin and carbenicillin.*
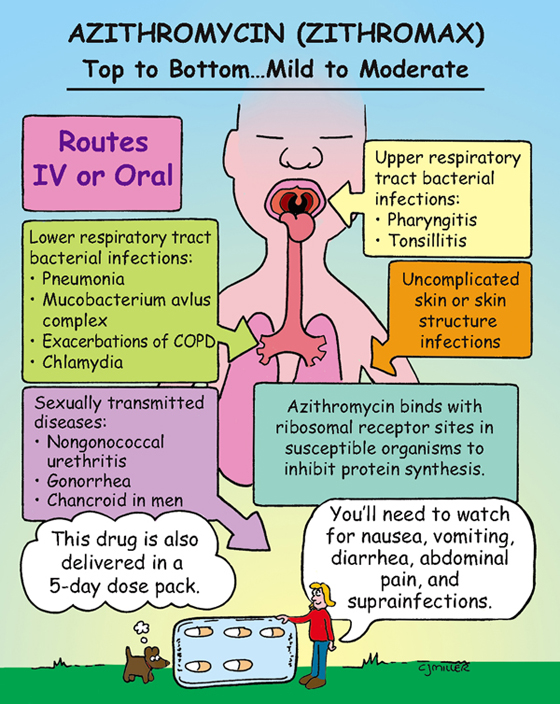
Azithromycin (Zithromax)
ACTION
Binds with ribosomal receptor sites in susceptible organisms to inhibit bacterial protein synthesis; is a derivative of erythromycin.
USES
Treats respiratory, ear, and skin infections; syphilis (for penicillin sensitive patients); Chlamydia trachomatis (drug of choice); cholera; and chancroid.
CONTRAINDICATION AND PRECAUTION
SIDE EFFECTS
NURSING IMPLICATIONS
1. *Take medication 1 hour before or 2 hours after food or antacids.*
2. Aluminum and magnesium antacids reduce rate of absorption but not extent.
3. *Observe for development of signs of suprainfection.*
4. ‡Instruct patient to take prescribed course of therapy, although symptoms may improve or disappear.‡
5. *Intravenous (IV) preparations are infused slowly over 60 minutes, followed by oral preparation of the medication.*
Aminoglycoside Toxicity
ACTION
Bactericidal against a wide variety of gram-negative bacteria (narrow-spectrum) and certain gram-positive organisms. Disrupts bacterial protein synthesis. Is used for serious infections.
CONTRAINDICATIONS AND PRECAUTIONS
• History of hypersensitivity or toxic reaction with aminoglycoside antibiotics
• Patients with renal impairment, history of eighth cranial nerve impairment
• Patients with myasthenia gravis
TOXICITY
• **Nephrotoxicity** (reversible injury) and **ototoxicity** (irreversible injury)
• †Neuromuscular blockade can lead to flaccid paralysis, and fatal respiratory depression can occur in patients receiving skeletal muscle relaxants.†
DRUG INTERACTIONS
• Ethacrynic acid (Edecrin) significantly increases ototoxicity.
NURSING IMPLICATIONS
1. Peak and trough levels should be assessed. Ototoxicity is associated with persistent high trough levels, rather than high peak levels.
2. Monitor renal function (e.g., blood urea nitrogen, creatinine levels).
3. Monitor for sensory problems (e.g., loss of hearing). ‡Instruct patients to report tinnitus, high-frequency hearing loss, persistent headache, nausea, dizziness, vertigo.‡
4. *Anticipate antidote of intravenous (IV) calcium gluconate for treatment of neuromuscular blockade.*