CASE 198
History: A 53-year-old man presents with hematemesis. Upper endoscopy identified an extramucosal mass distorting the gastric greater curvature.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
A. Colonic splenic flexure mass
2. Which of the following statements regarding the differences between splenic artery aneurysms and pseudoaneurysms is true?
B. Pseudoaneurysms are usually clinically silent and diagnosed as incidental findings.
C. Most splenic artery aneurysms occur as a complication of pancreatitis.
D. Splenic artery pseudoaneurysms are more common than aneurysms.
3. What is the most common site of aneurysm formation in the abdomen?
4. What is the usual first line of treatment of a splenic artery pseudoaneurysm?
D. Percutaneous thrombin injection
ANSWERS
CASE 198
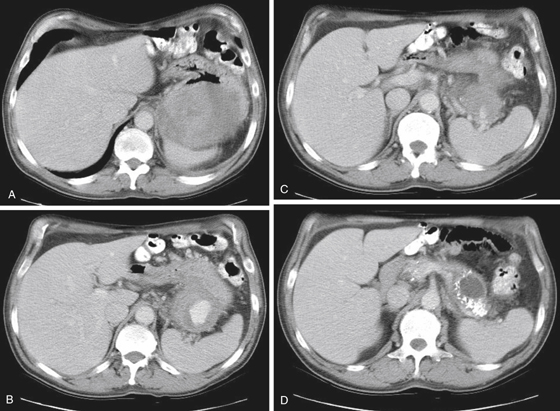
Pseudoaneurysm of the Splenic Artery
1. B, C, and D
2. A
3. D
4. C
References
Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. Radiographics. 2007;27(4):992-999.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 161.
Comment
Pseudoaneurysm of vessels in the pancreatic bed associated with chronic pancreatitis is uncommon but can be seen in a small percentage of patients (usually <5%). The most common vascular structure involved is the splenic artery, as in this case (see figures). The gastroduodenal artery is the next most commonly affected vessel. If the abnormality is seen in the region of the head of the pancreas, it is usually the gastroduodenal artery. If it is in the body of the pancreas, it is the splenic artery. Apart from the expected symptoms of chronic pancreatitis, patients often may have other symptoms relative to this vascular abnormality. Cases of gastrointestinal bleeding have been reported if the pseudoaneurysm breaks into the lumen of the gut or pancreatic duct, bile duct, or retroperitoneum itself. A few pancreaticoduodenal artery pseudoaneurysms have also been reported. These findings usually go undiagnosed without the use of CT or Doppler ultrasound.
The differential consideration that has to be excluded is a pancreatic pseudocyst. CT scanning with the use of intravenous contrast material can be definitive in most cases. Blood flow in the pseudoaneurysm can be detected with Doppler ultrasound in most cases. Physical examination is usually not productive, although pulsations detected during physical examination in the pancreatic bed of patients with chronic pancreatitis were diagnostic before widespread imaging; much of this art is lost today. Gastroduodenal artery pseudoaneurysms can occur in settings other than chronic alcoholism. Any condition that can result in pancreatitis can theoretically result in such a complication.