CASE 195
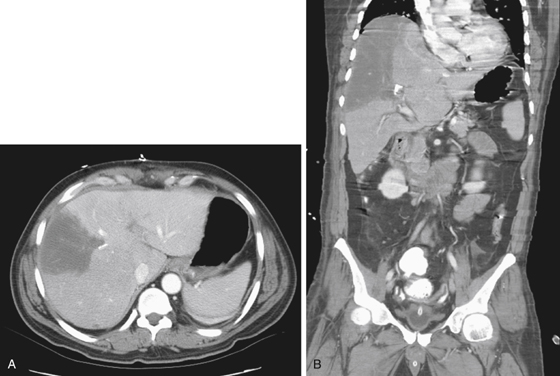
History: A 45-year-old man has abnormal liver function tests.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the most common cause of hepatic infarction secondary to hepatic artery occlusion?
3. Which of the following statements regarding the imaging appearances of hepatic infarction is true?
A. The presence of gas is diagnostic of infection.
B. Infarction may be complicated by formation of bile lakes.
C. Contrast-enhanced imaging is required to make the diagnosis.
D. Infarction is characterized by nonenhancement of the affected segment.
4. What is the primary blood supply of the liver?
ANSWERS
CASE 195
Focal Hepatic Artery Occlusion
1. A, C, and E
2. A
3. B
4. A
References
Lipson JA, Qayyum A, Avrin DE, et al: CT and MRI of hepatic contour abnormalities. AJR Am J Roentgenol. 2005;184(1):75-81.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 177.
Comment
The patient in this case developed the wedge-shaped defect after surgery as a result of the hepatic artery vessel being ligated (see figures). The wedge-shaped defect is the hepatic infarction resulting from the interruption of arterial blood to the involved segment. One might think that because the liver has two blood supplies, the portal venous and the hepatic arterial, infarction might be impossible. However, it has been shown that the portal venous system alone cannot protect the liver from possible infarction if there is occlusion of the hepatic artery or its branches. This situation may relate to function. While the portal veins are transporting absorbed content from the gastrointestinal tract to the liver for metabolism, the hepatic artery, rich in oxygen, has the primary function of delivering that oxygen to the hepatocyte.
Most infarcts occur in the right lobe of the liver, which is not surprising because this is the largest part of the liver. The best diagnostic tool at the present time is CT with images obtained in the late arterial phase of scanning. However, even in the portal venous phase, tissue damage still results in the wedge-shaped deformity well described in imaging literature. In the right clinical setting, the diagnosis can be made with confidence. However, the imaging appearance is not specific, especially in patients who present with CT findings similar to infarction but do not have the appropriate clinical history. Other etiologic factors must be considered, such as hepatic abscess, laceration, unusual metastatic lesion, and, in rare cases, lymphoma of the liver. However, with the continued refinement of CT arteriography, the ability to trace the hepatic artery as it swings away from the celiac axis, dividing into its right and left branches in the porta hepatis, has vastly improved.