CASE 194
History: A 38-year-old woman presents with diarrhea and abdominal bloating.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. In scleroderma, what intestinal organ is most commonly involved?
3. What are the underlying pathologic changes seen in the bowel as a result of scleroderma?
A. Small vessel vasculitis and fibrosis
4. What is the term used to describe small bowel that appears dilated with crowding of normal thickness valvulae conniventes?
ANSWERS
CASE 194
Scleroderma of the Small Bowel and Colon
1. A, B, C, and D
2. C
3. A
4. A
References
Madani G, Katz RD, Haddock JA, et al: The role of radiology in the management of systemic sclerosis. Clin Radiol. 2008;63(9):959-967.
Pickhardt PJ. The “hide-bound” bowel sign. Radiology. 1999;213(3):837-838.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 113.
Comment
Numerous connective tissue diseases can affect the small bowel and colon. Scleroderma is caused by abnormal deposition of collagen in the skin, adjacent to blood vessels, and in various visceral organs. It may be isolated or may occur as part of CREST syndrome, which includes changes caused by calcinosis, Raynaud’s disease, esophageal dysmotility, sclerodactyly, and telangiectasia (CREST). Mixed connective tissue disease is considered a distinct disease that has features of several connective tissue diseases, including systemic lupus erythematosus, scleroderma, polymyositis, and rheumatoid arthritis. In this condition, as in scleroderma, the esophagus is the organ most often involved, with dysmotility being the main feature.
The major abnormality of scleroderma is the abnormal deposition of collagen into various tissues including the bowel. Fibrosis is a major feature of this disease, and although the esophagus is most commonly involved, fibrosis can also be seen in both colon and small bowel. There is also associated small vessel damage, particularly to the intestines, because much of this deposition produces vasculitis-type changes, with resultant long-term ischemia of the bowel. Malabsorption results because of stasis of the bowel contents, bacterial overgrowth, poor absorption of bile salts, and impaired lymphatic drainage. Diarrhea, weight loss, and bloating are symptoms of this condition.
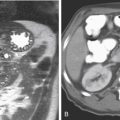
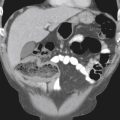
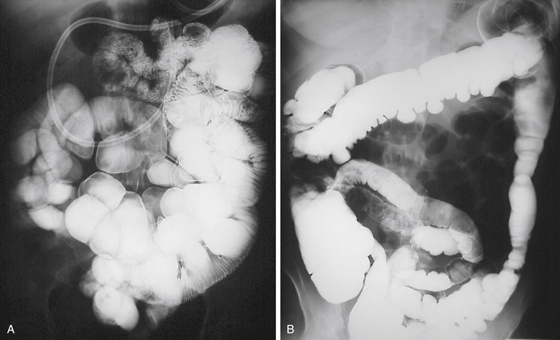
Radiologically, the changes of fibrosis, muscle atrophy, and vasculitis produce dilation of the small bowel, which is often termed pseudoobstruction. Pneumatosis is a known finding, especially pneumatosis coli, but its underlying cause is unclear. A pathognomonic change seen in the bowel is crowding of the valvulae, or a “hide-bound” appearance. The fibrosis of the bowel draws the valvulae closer together, producing more valvulae (>5) per inch than normal (see figures). The margins of the intestines also may be flattened. This flattening gives the bowel an accordion-pleated appearance. In the colon, the changes are often a diminished or disordered haustral pattern with wide-mouth diverticula-like deformities (see figures).