CASE 193
History: A 32-year-old woman presents with lower abdominal pain; a low hematocrit also is discovered.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the most common cause of small bowel hemorrhage?
3. What finding on CT is most suggestive of small bowel hemorrhage?
A. Circumferential bowel wall thickening
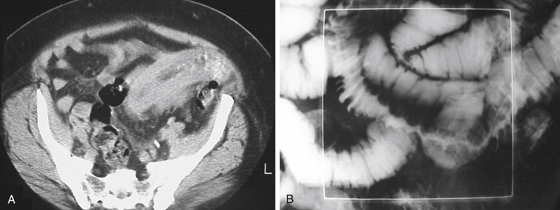
4. This patient underwent a barium small bowel study (see figures). In the involved segment, the mucosal folds are thickened but remain straight and parallel. What is this pattern of fold abnormality known as?
ANSWERS
CASE 193
Small Bowel Intramural Hemorrhage
1. A, B, C, and E
2. C
3. B
4. C
References
Abbas MA, Collins JM, Olden KW. Spontaneous intramural small-bowel hematoma: imaging findings and outcome. AJR Am J Roentgenol. 2002;179(6):1389-1394.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 120.
Comment
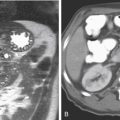
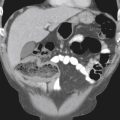
A patient presenting with abdominal pain and CT findings (see figures) such as in this case must raise many diagnostic possibilities in the mind of the radiologist. The fact that this patient is relatively young lessens, but does not exclude, the possibility of ischemic disease and intramural hemorrhage. Hypoperfusion, such as in hypovolemic shocked bowel, would be a consideration. Disease that manifests as an intramural vasculitis, such as Henoch-Schönlein purpura affecting the bowel with intramural bleeding, may also give such a picture. The CT images in this case show thickened small bowel wall and folds.
This patient underwent a barium small bowel study (see figures). In the involved segment, the folds are “stacked” together producing the well-known “stack of coins” or “picket fence” sign. This patient had a severe intramural hemorrhage of the small bowel. Multidetector CT showed no evidence of arterial occlusion of the major mesenteric vessels. The length of involved bowel would make blunt trauma less likely. An infiltrative process, neoplastic or nonneoplastic, is always a possibility. Carcinoid involvement of the bowel might be considered, although the desmoplastic distortion of bowel loops is not present in this case. Metastatic disease would not likely affect such an extended length of bowel. Nonneoplastic diagnostic considerations include intramural edema, intramural bleeding, and less likely possibilities such as lymphangiectasia and amyloid of the bowel. In this case, all findings were the result of mesenteric and intramural small bowel bleeding. A CT scan repeated 3 weeks later showed normal small bowel throughout, which is an almost sure diagnostic sign of bleeding.