Procedure 19 Tendon Transfers for Ulnar Nerve Palsy
![]() See Video 15: Tendon Transfers for High Median and Ulnar Nerve Palsy
See Video 15: Tendon Transfers for High Median and Ulnar Nerve Palsy
Indications
 Delayed presentation (>1 year) of an ulnar nerve laceration
Delayed presentation (>1 year) of an ulnar nerve laceration
 Failed motor recovery after repair/reconstruction of the ulnar nerve
Failed motor recovery after repair/reconstruction of the ulnar nerve
 Failed motor recovery after release of ulnar nerve compression at Guyon canal or cubital tunnel
Failed motor recovery after release of ulnar nerve compression at Guyon canal or cubital tunnel
 Persistent motor weakness after completion of drug therapy in Hansen disease (leprosy)
Persistent motor weakness after completion of drug therapy in Hansen disease (leprosy)
 Neurologic disorders (for example, Charcot-Marie-Tooth disease, syringomyelia)
Neurologic disorders (for example, Charcot-Marie-Tooth disease, syringomyelia)
Examination/Imaging
Clinical Examination
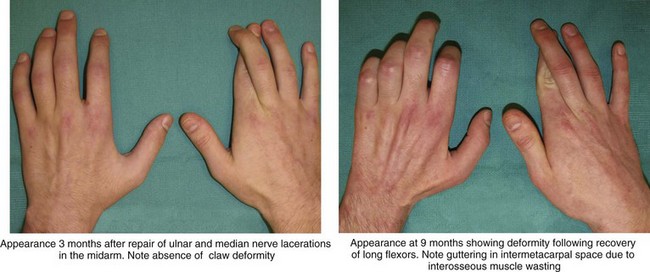
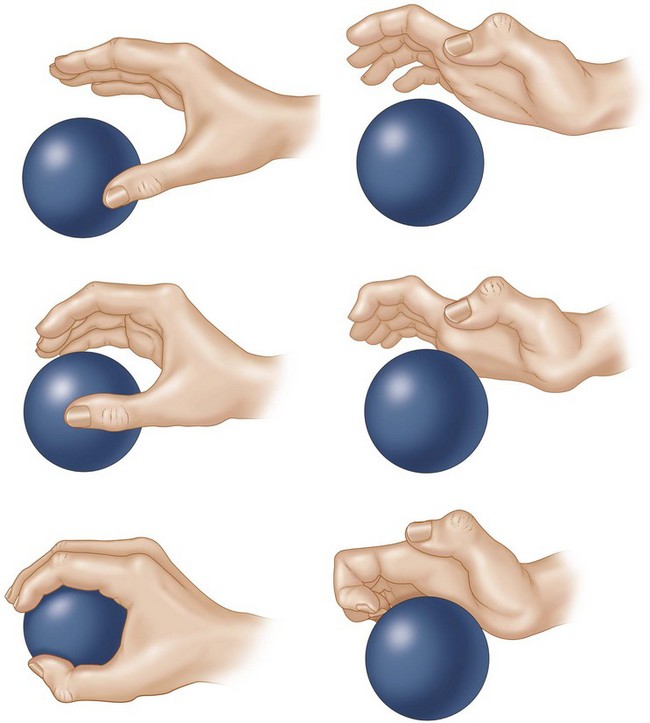
 Functional deficit: The loss of function in ulnar nerve palsy results from the claw deformity, which causes an abnormal pattern of finger flexion, weak thumb key pinch, small finger abduction deformity, and loss of ring and small finger distal interphalangeal (DIP) joint flexion (Fig. 19-1). However, these problems may not be functionally disabling in all patients, and some may require correction of only one aspect. It is important to determine this and then to set a sequence for the appropriate corrective procedures. It is better to correct the lack of DIP joint flexion first, followed by transfers for restoring thumb key pinch, and finally correction of the claw deformity because it is difficult to establish appropriate intrinsic plus posture of the hand.
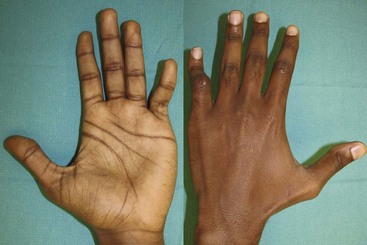
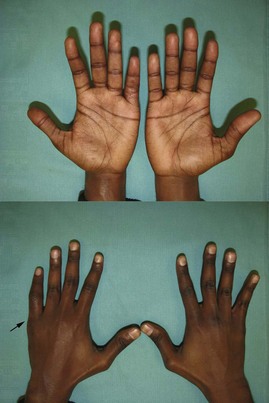
Functional deficit: The loss of function in ulnar nerve palsy results from the claw deformity, which causes an abnormal pattern of finger flexion, weak thumb key pinch, small finger abduction deformity, and loss of ring and small finger distal interphalangeal (DIP) joint flexion (Fig. 19-1). However, these problems may not be functionally disabling in all patients, and some may require correction of only one aspect. It is important to determine this and then to set a sequence for the appropriate corrective procedures. It is better to correct the lack of DIP joint flexion first, followed by transfers for restoring thumb key pinch, and finally correction of the claw deformity because it is difficult to establish appropriate intrinsic plus posture of the hand.
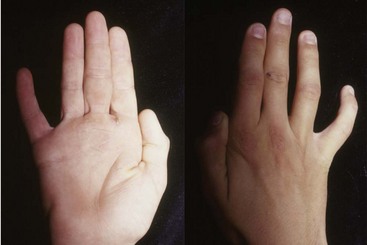
 Sensation: It is important to document the level of sensation in the thumb and the fingers preoperatively. Loss of sensation on the dorsoulnar aspect of the hand, which is innervated by the dorsal branch of ulnar nerve, can help differentiate a high ulnar nerve lesion (e.g., cubital tunnel compression) from a low ulnar nerve lesion (e.g., Guyon canal compression), which should have preserved sensation over the dorsal-ulnar hand (Fig. 19-7).
Sensation: It is important to document the level of sensation in the thumb and the fingers preoperatively. Loss of sensation on the dorsoulnar aspect of the hand, which is innervated by the dorsal branch of ulnar nerve, can help differentiate a high ulnar nerve lesion (e.g., cubital tunnel compression) from a low ulnar nerve lesion (e.g., Guyon canal compression), which should have preserved sensation over the dorsal-ulnar hand (Fig. 19-7).
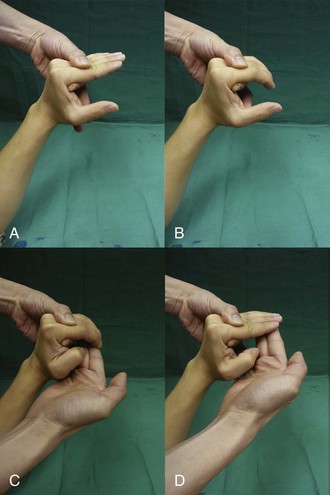
 Joints: To achieve a good result from the tendon transfer, patients must have good passive range of motion at the IP and the MCP joints. The most important aspect of assessment of an ulnar nerve palsy is determining whether the patient can extend the PIP joint with the examiner correcting the MCP joint hyperextension (Bouvier maneuver) (Fig. 19-8).
Joints: To achieve a good result from the tendon transfer, patients must have good passive range of motion at the IP and the MCP joints. The most important aspect of assessment of an ulnar nerve palsy is determining whether the patient can extend the PIP joint with the examiner correcting the MCP joint hyperextension (Bouvier maneuver) (Fig. 19-8).
 Selection of motor: We use a static procedure (MCP joint volar plate advancement) for correction of the claw deformity in patients who are able to achieve full active extension of the PIP joint. In patients unable to achieve full PIP joint extension, we use a dynamic transfer and prefer the long or ring finger FDS as a motor. We prefer to use the ring finger FDS in low ulnar nerve palsy because the FDS is important for chuck grip, which is predominantly a function of the thumb and index and long fingers. In patients with high ulnar nerve palsy with a weak or absent FDP to the ring finger, the FDS remains the only flexor of the ring finger, and it is prudent to use the long finger FDS. Other motors that have been described include the extensor indicis proprius (EIP) and EDM (both have insufficient length, resulting in excessive tension of the extensor apparatus), wrist flexors (flexor carpi radialis [FCR], palmaris longus [PL]), and wrist extensors (extensor carpi radialis longus [ECRL], extensor carpi radialis brevis [ECRB]). (All need a tendon graft.) We use the ECRB lengthened with a PL tendon graft as the motor for restoring thumb pinch. Other motors that have been described include the brachioradialis, ECRL, extensor carpi ulnaris (ECU), EIP, and FDS.
Selection of motor: We use a static procedure (MCP joint volar plate advancement) for correction of the claw deformity in patients who are able to achieve full active extension of the PIP joint. In patients unable to achieve full PIP joint extension, we use a dynamic transfer and prefer the long or ring finger FDS as a motor. We prefer to use the ring finger FDS in low ulnar nerve palsy because the FDS is important for chuck grip, which is predominantly a function of the thumb and index and long fingers. In patients with high ulnar nerve palsy with a weak or absent FDP to the ring finger, the FDS remains the only flexor of the ring finger, and it is prudent to use the long finger FDS. Other motors that have been described include the extensor indicis proprius (EIP) and EDM (both have insufficient length, resulting in excessive tension of the extensor apparatus), wrist flexors (flexor carpi radialis [FCR], palmaris longus [PL]), and wrist extensors (extensor carpi radialis longus [ECRL], extensor carpi radialis brevis [ECRB]). (All need a tendon graft.) We use the ECRB lengthened with a PL tendon graft as the motor for restoring thumb pinch. Other motors that have been described include the brachioradialis, ECRL, extensor carpi ulnaris (ECU), EIP, and FDS.
Surgical Anatomy
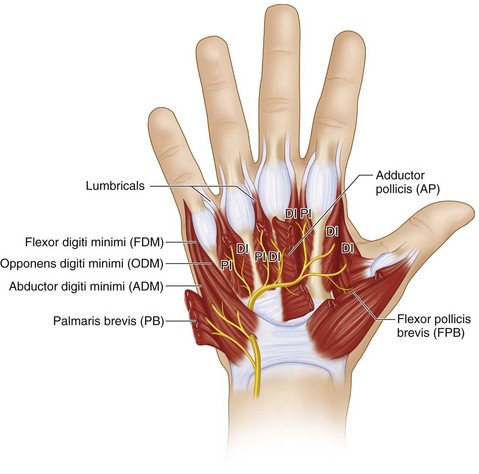
 The muscles affected after low ulnar nerve palsy are the four hypothenar muscles (abductor digitorum minimus [ADM], flexor digitorum minimus [FDM], opponens digitorum minimus [ODM], and palmaris brevis [PB]), seven interossei muscles (four dorsal and three palmar), third and fourth lumbricals, and two thenar muscles (adductor pollicis [AP] and the deep head of the flexor pollicis brevis [FPB]). All these muscles are innervated by the deep motor branch of the ulnar nerve (Fig. 19-10).
The muscles affected after low ulnar nerve palsy are the four hypothenar muscles (abductor digitorum minimus [ADM], flexor digitorum minimus [FDM], opponens digitorum minimus [ODM], and palmaris brevis [PB]), seven interossei muscles (four dorsal and three palmar), third and fourth lumbricals, and two thenar muscles (adductor pollicis [AP] and the deep head of the flexor pollicis brevis [FPB]). All these muscles are innervated by the deep motor branch of the ulnar nerve (Fig. 19-10).
 In high ulnar nerve palsy, the flexor carpi ulnaris (FCU) and the ulnar half of the FDP (ring and small fingers) are affected in addition to the muscles listed earlier.
In high ulnar nerve palsy, the flexor carpi ulnaris (FCU) and the ulnar half of the FDP (ring and small fingers) are affected in addition to the muscles listed earlier.
Procedure 1—Static Correction of Claw Deformity with an MCP Joint Volar Plate Advancement
Exposures
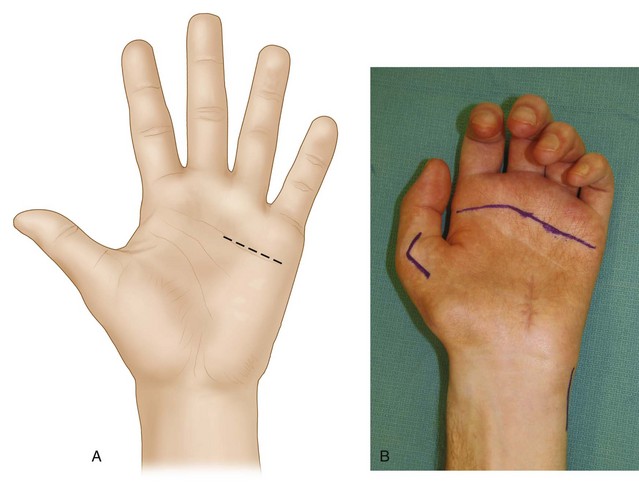
 A 3-cm transverse incision is made in line with the distal palmar crease overlying the ring and small finger MCP joints (Fig.19-11A and B).
A 3-cm transverse incision is made in line with the distal palmar crease overlying the ring and small finger MCP joints (Fig.19-11A and B).
 The skin and subcutaneous fat are dissected, and common digital neurovascular bundles are identified and protected.
The skin and subcutaneous fat are dissected, and common digital neurovascular bundles are identified and protected.
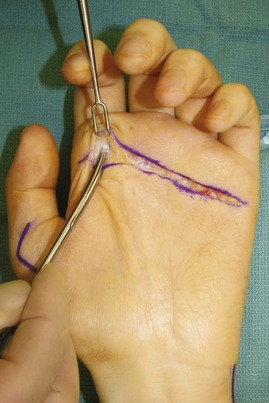
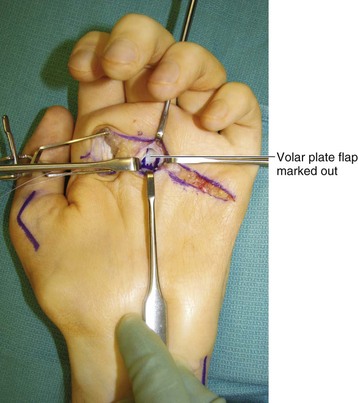
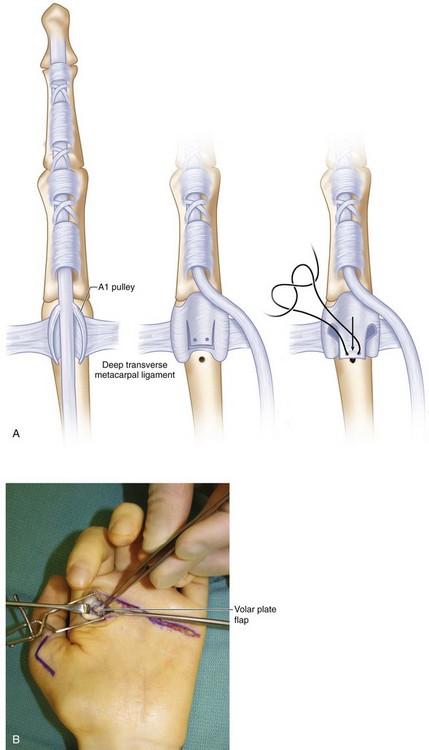
 The flexor tendon sheaths of the ring and small fingers are identified, and the A1 pulley is exposed (Fig. 19-12).
The flexor tendon sheaths of the ring and small fingers are identified, and the A1 pulley is exposed (Fig. 19-12).
Procedure
Step 1
Step 3
Step 4
Step 5
Step 5 Pearls
It is better to pass the sutures for all the fingers through the volar plate and tie them at the end instead of completing one finger and then proceeding to the next (Fig. 19-16). Passing the suture through the volar plate requires significant retraction, and an adjacent flexed finger will hinder this.
The suture must hold a good bite of the thick portion of the volar plate.
Step 6
 The wrist is maintained in a neutral position, and the ring finger capsular flap is sutured down to the neck of the metacarpal using the bone anchor sutures such that the MCP joint is flexed to about 45 to 50 degrees. The ring finger MCP joint should have slightly greater flexion compared with the long finger (Fig. 19-17).
The wrist is maintained in a neutral position, and the ring finger capsular flap is sutured down to the neck of the metacarpal using the bone anchor sutures such that the MCP joint is flexed to about 45 to 50 degrees. The ring finger MCP joint should have slightly greater flexion compared with the long finger (Fig. 19-17).
 The small finger flap is sutured next to obtain 50 to 55 degrees of MCP joint flexion and should be slightly more in comparison to the ring finger.
The small finger flap is sutured next to obtain 50 to 55 degrees of MCP joint flexion and should be slightly more in comparison to the ring finger.
Step 6 Pearls
The amount of MCP joint flexion required to produce full PIP joint extension preoperatively can guide the surgeon regarding the degree of MCP joint flexion required intraoperatively.
Some authors recommend excising a 1.5-cm ellipse of skin (dermodesis) to prevent stretching the volar plate and overcorrecting the deformity.
Postoperative Care and Expected Outcomes
 The hand is splinted with the wrist in neutral and the MCP joint in 50 to 60 degrees of flexion. The IP joints are left free to move.
The hand is splinted with the wrist in neutral and the MCP joint in 50 to 60 degrees of flexion. The IP joints are left free to move.
 Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is encouraged to move the MCP joint, and a knuckle-bender splint is provided. One should avoid passive stretching of the MCP joint. A protective removable splint is also provided for night wear and general protection for the next 4 weeks. The knuckle-bender and protective splints are discontinued 2 months after surgery, and the patient is allowed unrestricted activity.
Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is encouraged to move the MCP joint, and a knuckle-bender splint is provided. One should avoid passive stretching of the MCP joint. A protective removable splint is also provided for night wear and general protection for the next 4 weeks. The knuckle-bender and protective splints are discontinued 2 months after surgery, and the patient is allowed unrestricted activity.
 Volar plate advancement is a simple procedure that gives good results in patients who can fully extend the PIP joint when the MCP joint is held in flexion. A bone anchor fixation of the volar plate reduces the incidence of loss of correction over time as a result of stretching. This procedure is not recommended for patients engaged in heavy manual labor who will certainly stretch the volar plate. A dynamic transfer may be more appropriate.
Volar plate advancement is a simple procedure that gives good results in patients who can fully extend the PIP joint when the MCP joint is held in flexion. A bone anchor fixation of the volar plate reduces the incidence of loss of correction over time as a result of stretching. This procedure is not recommended for patients engaged in heavy manual labor who will certainly stretch the volar plate. A dynamic transfer may be more appropriate.
Procedure 2—Dynamic Correction of Claw Deformity with Transfer of Ring Finger FDS
Exposures
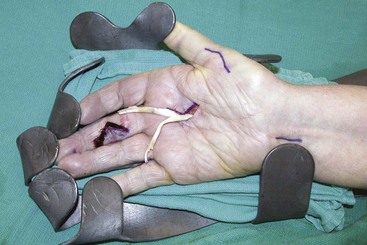
 A Bruner-type incision centered over the PIP joint is made over the ring finger. Both neurovascular bundles are identified and retracted laterally to expose the flexor tendon sheath. Subsequently, the radial neurovascular bundle is retracted ulnarly, and a tissue plane is developed deep to it to expose the radial lateral band, which will receive the tendon transfer.
A Bruner-type incision centered over the PIP joint is made over the ring finger. Both neurovascular bundles are identified and retracted laterally to expose the flexor tendon sheath. Subsequently, the radial neurovascular bundle is retracted ulnarly, and a tissue plane is developed deep to it to expose the radial lateral band, which will receive the tendon transfer.
 A second 3-cm longitudinal zigzag incision is made in the midpalm proximal to the proximal palmar crease. The skin and subcutaneous fat are dissected, and the common digital neurovascular bundles and the superficial arch are identified and protected. The flexor tendons are exposed.
A second 3-cm longitudinal zigzag incision is made in the midpalm proximal to the proximal palmar crease. The skin and subcutaneous fat are dissected, and the common digital neurovascular bundles and the superficial arch are identified and protected. The flexor tendons are exposed.
 A third 2-cm longitudinal incision is made on the radial aspect of the small finger proximal phalanx. The soft tissue is dissected to expose the radial lateral band (Fig. 19-18).
A third 2-cm longitudinal incision is made on the radial aspect of the small finger proximal phalanx. The soft tissue is dissected to expose the radial lateral band (Fig. 19-18).
Pearls
Additional lateral incisions can be made on the ulnar aspect of the index finger and radial aspect of the long finger if a claw correction of all four fingers is required.
The ulnar lateral band of the index and the radial lateral bands of the long, ring, and small fingers are chosen so that the tendon transfer can produce some adduction of these digits in addition to flexion at the MCP joint and extension at the PIP joint.
The long finger FDS should be used in patients with a high ulnar nerve palsy.
Step 1
 The A3 pulley of the ring finger is opened, and both slips of the FDS are identified.
The A3 pulley of the ring finger is opened, and both slips of the FDS are identified.
 Both slips of the FDS are divided as distally as possible.
Both slips of the FDS are divided as distally as possible.
 The divided ends are held with a hemostat and pulled distally to identify the chiasma, which is then divided.
The divided ends are held with a hemostat and pulled distally to identify the chiasma, which is then divided.
Step 1 Pearls
In patients who have a hyperextensible PIP joint, dividing the FDS proximal to the PIP joint can prevent the development of a swan neck deformity because the distal FDS insertion may be adherent to the volar plate and serve as a restraint. In patients who have a stiff PIP joint, the FDS should be divided distal to the PIP joint to prevent development of a flexion contracture.
Step 2
 The ring finger FDS tendon is identified at the midpalmar incision and withdrawn out of the incision.
The ring finger FDS tendon is identified at the midpalmar incision and withdrawn out of the incision.
 The distal split in the FDS tendon is completed all the way in the visible portion of the tendon (Fig. 19-19).
The distal split in the FDS tendon is completed all the way in the visible portion of the tendon (Fig. 19-19).
Step 3
 The origin of the lumbrical muscle from the FDP is identified. A mosquito forceps or a tendon passer is passed from the palmar incision along the lumbrical through the lumbrical canal (remaining superficial/palmar to the deep transverse metacarpal ligament) to exit on the incision made on the radial side of the small finger (Fig. 19-21).
The origin of the lumbrical muscle from the FDP is identified. A mosquito forceps or a tendon passer is passed from the palmar incision along the lumbrical through the lumbrical canal (remaining superficial/palmar to the deep transverse metacarpal ligament) to exit on the incision made on the radial side of the small finger (Fig. 19-21).
 The jaws of the mosquito forceps are used to hold another mosquito forceps, which is brought into the palmar wound by withdrawing the first forceps. The tip of the mosquito forceps holds the distal end of the ulnar slip of the FDS and brings it out of the radial aspect of the small finger. The mosquito forceps is not removed and continues to hold the tendon.
The jaws of the mosquito forceps are used to hold another mosquito forceps, which is brought into the palmar wound by withdrawing the first forceps. The tip of the mosquito forceps holds the distal end of the ulnar slip of the FDS and brings it out of the radial aspect of the small finger. The mosquito forceps is not removed and continues to hold the tendon.
 The same procedure is repeated to bring the radial slip of the FDS through the lumbrical canal on the radial aspect of the ring finger (Fig. 19-22).
The same procedure is repeated to bring the radial slip of the FDS through the lumbrical canal on the radial aspect of the ring finger (Fig. 19-22).
Step 5
 The forearm is pronated, and a rolled-up towel is placed in the palm so that the wrist is in neutral position and the MCP joints are flexed beyond the rolled towel.
The forearm is pronated, and a rolled-up towel is placed in the palm so that the wrist is in neutral position and the MCP joints are flexed beyond the rolled towel.
 The hemostat holding the FDS slip on the radial side of the ring finger is pulled to bring the MCP joint into about 60 degrees of flexion. (Aim to get slightly greater flexion than the adjacent long finger so that the normal cascade can be obtained.) The PIP joint is held in full extension by the assistant, and a single preliminary suture of the FDS to the lateral band is made.
The hemostat holding the FDS slip on the radial side of the ring finger is pulled to bring the MCP joint into about 60 degrees of flexion. (Aim to get slightly greater flexion than the adjacent long finger so that the normal cascade can be obtained.) The PIP joint is held in full extension by the assistant, and a single preliminary suture of the FDS to the lateral band is made.
 The tension and the finger cascade are confirmed by taking the wrist through a gentle range of motion. If the tension is correct, two or three nonabsorbable horizontal mattress sutures are placed between the FDS and the lateral bands.
The tension and the finger cascade are confirmed by taking the wrist through a gentle range of motion. If the tension is correct, two or three nonabsorbable horizontal mattress sutures are placed between the FDS and the lateral bands.
Step 5 Pearls
The MCP joint cascade can be corrected by tightening or loosening the FDS attachment to the lateral band.
The desired tension is to keep the MCP joint in about 60 to 70 degrees of flexion and the IP joint in full extension, with the wrist at about 20 degrees of extension. In most cases, the ideal tension cannot be established because of the large amount of excursion of the FDS, which reaches 70 mm. Therefore, getting close to this posture is acceptable because the FDS, which is considered a smart tendon because of its excursion, can modulate the tension to reach an acceptable posture (Fig. 19-23).
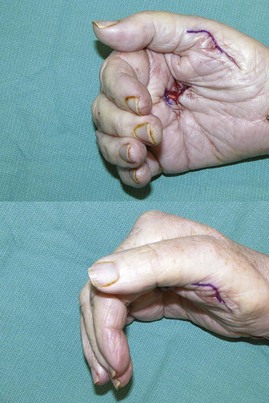
Postoperative Care and Expected Outcomes
 The hand is splinted with the wrist in neutral position, the MCP joint in 60 to 70 degrees of flexion, and the IP joints in full extension.
The hand is splinted with the wrist in neutral position, the MCP joint in 60 to 70 degrees of flexion, and the IP joints in full extension.
 Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is given a dorsal blocking splint that keeps the MCP joint flexed but allows full extension and flexion of the IP joint for another 4 weeks. The splint is discontinued 2 months after surgery, and the patient is allowed unrestricted activity.
Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is given a dorsal blocking splint that keeps the MCP joint flexed but allows full extension and flexion of the IP joint for another 4 weeks. The splint is discontinued 2 months after surgery, and the patient is allowed unrestricted activity.
 The transfer of FDS reliably corrects MCP joint hyperextension but does not improve grip strength and may not fully correct the loss of PIP joint extension. This procedure gives good results in supple joints, although the patient may develop a swan neck deformity from loss of volar restraint provided by the FDS.
The transfer of FDS reliably corrects MCP joint hyperextension but does not improve grip strength and may not fully correct the loss of PIP joint extension. This procedure gives good results in supple joints, although the patient may develop a swan neck deformity from loss of volar restraint provided by the FDS.
Procedure 3—Restoration of Thumb Adduction with an ECRB Tendon Transfer
Exposures
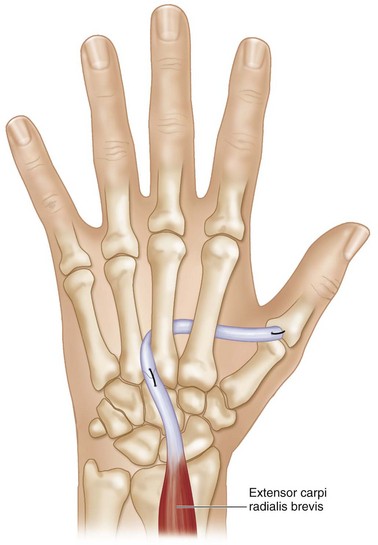
 A 3-cm longitudinal incision is made starting at the base of the ulnar aspect of the long finger metacarpal and extending distally. The soft tissue is dissected, and the ECRB is exposed at its insertion onto the base of the long metacarpal. Distally, the dorsal interosseous fascia overlying the interspace between the long and ring metacarpals is divided, and interosseous muscles are exposed (Fig. 19-24).
A 3-cm longitudinal incision is made starting at the base of the ulnar aspect of the long finger metacarpal and extending distally. The soft tissue is dissected, and the ECRB is exposed at its insertion onto the base of the long metacarpal. Distally, the dorsal interosseous fascia overlying the interspace between the long and ring metacarpals is divided, and interosseous muscles are exposed (Fig. 19-24).
 Through this incision, the ECRB tendon is identified immediately proximal to the extensor retinaculum.
Through this incision, the ECRB tendon is identified immediately proximal to the extensor retinaculum.
 A 1-cm longitudinal incision is made on the ulnar aspect of the thumb MCP joint, and the soft tissue is dissected to expose the insertion of the adductor pollicis.
A 1-cm longitudinal incision is made on the ulnar aspect of the thumb MCP joint, and the soft tissue is dissected to expose the insertion of the adductor pollicis.
 A 1-cm incision is made at the proximal wrist crease, and the tendon of the palmaris longus is identified and exposed.
A 1-cm incision is made at the proximal wrist crease, and the tendon of the palmaris longus is identified and exposed.
Step 3
Step 4
Step 6
 A curved hemostat is used to make a subcutaneous tunnel from the ulnar aspect of the thumb MCP joint to the third to fourth intermetacarpal space. This tunnel is made superficial (palmar) to the adductor pollicis but deep (dorsal) to the flexor tendons (Fig. 19-27).
A curved hemostat is used to make a subcutaneous tunnel from the ulnar aspect of the thumb MCP joint to the third to fourth intermetacarpal space. This tunnel is made superficial (palmar) to the adductor pollicis but deep (dorsal) to the flexor tendons (Fig. 19-27).
 The hemostat then grabs the ECRB extended by the PL graft and brings it out to the thumb.
The hemostat then grabs the ECRB extended by the PL graft and brings it out to the thumb.
Postoperative Care and Expected Outcomes
 The hand is splinted with the wrist and thumb in neutral position.
The hand is splinted with the wrist and thumb in neutral position.
 Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is given a protective splint and encouraged to move the thumb and wrist.
Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is given a protective splint and encouraged to move the thumb and wrist.
 The transfer of ECRB restores thumb pinch and improves the ability to perform activities of daily living. Patients recover about 50% of the pinch strength of the contralateral thumb. This transfer may restrict thumb opposition and palmar abduction.
The transfer of ECRB restores thumb pinch and improves the ability to perform activities of daily living. Patients recover about 50% of the pinch strength of the contralateral thumb. This transfer may restrict thumb opposition and palmar abduction.
Procedure 4—Correction of Abduction Deformity (Wartenberg Sign) of Small Finger
Exposures
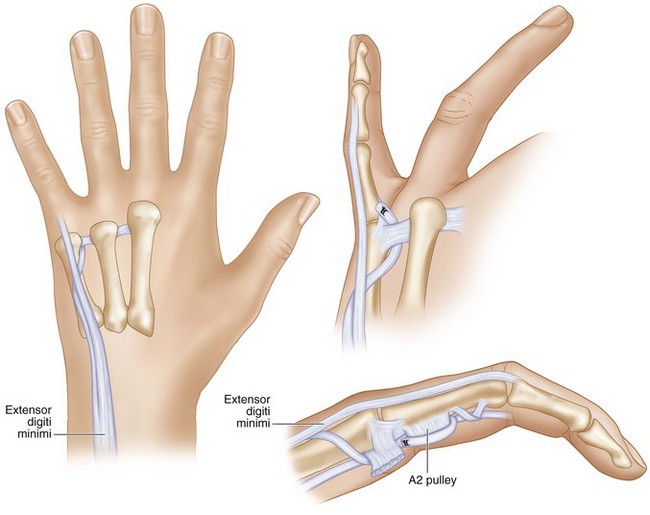
 A 3-cm chevron-shaped incision with the apex directed ulnarly is made over the dorsal aspect of the small finger MCP joint. The skin and soft tissue are dissected to expose the tendon of the EDM (Figs. 19-29 and 19-30).
A 3-cm chevron-shaped incision with the apex directed ulnarly is made over the dorsal aspect of the small finger MCP joint. The skin and soft tissue are dissected to expose the tendon of the EDM (Figs. 19-29 and 19-30).
 The radial collateral ligament of the small finger MCP joint is exposed by making a longitudinal incision in the proximal portion of the extensor hood overlying the radial aspect of the small finger MCP joint.
The radial collateral ligament of the small finger MCP joint is exposed by making a longitudinal incision in the proximal portion of the extensor hood overlying the radial aspect of the small finger MCP joint.
Step 1
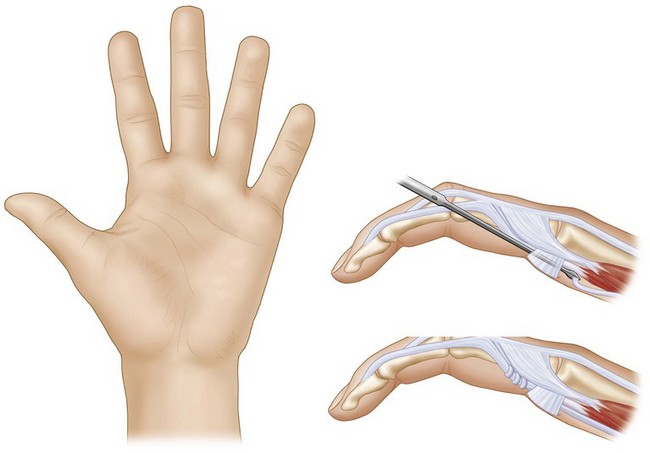
 The ulnar insertion of the EDM is detached from the extensor hood and dissected proximally from the remainder of the EDM for about 2 to 3 cm proximal to the MCP joint.
The ulnar insertion of the EDM is detached from the extensor hood and dissected proximally from the remainder of the EDM for about 2 to 3 cm proximal to the MCP joint.
 This tendon is now passed radially under the EDM and the extensor digitorum communis (EDC) to the small finger to reach the radial side of the small finger MCP joint.
This tendon is now passed radially under the EDM and the extensor digitorum communis (EDC) to the small finger to reach the radial side of the small finger MCP joint.
Step 2
 The tendon is sutured to the phalangeal attachment of the radial collateral ligament with the wrist in neutral position with the assistant holding the small finger adducted (Fig. 19-31).
The tendon is sutured to the phalangeal attachment of the radial collateral ligament with the wrist in neutral position with the assistant holding the small finger adducted (Fig. 19-31).
Step 2 Pearls
The transfer of the ulnar half of the EDM tendon to the radial collateral ligament is useful in patients with low ulnar nerve palsy who have an abduction deformity but do not have clawing or have clawing that has been corrected by a previous transfer.
In patients who have clawing, an additional 2.5-cm oblique palmar incision is made between the distal palmar crease and the proximal digital crease of the small finger. The common digital neurovascular bundle is identified and retracted radially to expose the deep transverse metacarpal ligament. The EDM tendon is retrieved using a hemostat and passed from dorsum to palmar between the fourth and fifth metacarpals, remaining palmar to the deep transverse metacarpal ligament. It is passed through a slit made in the proximal half of the A2 pulley and sutured to itself with the assistant holding the wrist in neutral position, the MCP joint in 20 degrees of flexion, and the small finger adducted (see Fig. 19-31).
Postoperative Care and Expected Outcomes
 A splint is applied that keeps the small and ring fingers MCP joints in 60 to 70 degrees of flexion and the wrist in neutral position. The IP joints are left free.
A splint is applied that keeps the small and ring fingers MCP joints in 60 to 70 degrees of flexion and the wrist in neutral position. The IP joints are left free.
 Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is encouraged to move the MCP joint, and a protective removable splint is also provided for night wear and general protection for the next 4 weeks. The protective splint is discontinued 2 months after surgery, and the patient is allowed unrestricted activity (Fig. 19-32).
Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable splint that the patient will wear for another 4 weeks, provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand. Thereafter, the patient is encouraged to move the MCP joint, and a protective removable splint is also provided for night wear and general protection for the next 4 weeks. The protective splint is discontinued 2 months after surgery, and the patient is allowed unrestricted activity (Fig. 19-32).
 This is a simple procedure to correct an annoying disability.
This is a simple procedure to correct an annoying disability.
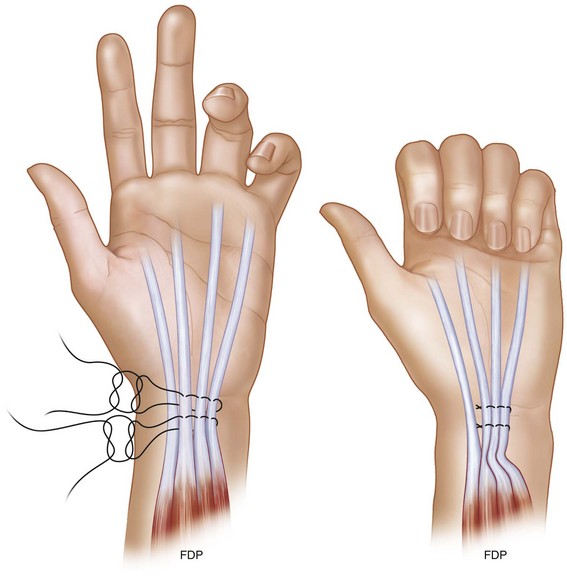
Procedure 5—Side-to-Side FDP Transfer for Restoration of Ring and Small Finger DIP Joint Flexion Strength (High Ulnar Palsy)
Exposures
 A 4-cm longitudinal incision is made 2 cm proximal to the wrist crease ulnar and parallel to the tendon of the palmaris longus. The antebrachial fascia is divided, and the PL tendon is retracted radially. The median nerve is identified and retracted radially. Next, the FDS tendons to the ring and long finger are identified and retracted radially. Immediately below are the FDS tendons to the small and index fingers. The index FDS is retracted radially, and the small FDS is retracted ulnarly. This exposes the four FDP tendons.
A 4-cm longitudinal incision is made 2 cm proximal to the wrist crease ulnar and parallel to the tendon of the palmaris longus. The antebrachial fascia is divided, and the PL tendon is retracted radially. The median nerve is identified and retracted radially. Next, the FDS tendons to the ring and long finger are identified and retracted radially. Immediately below are the FDS tendons to the small and index fingers. The index FDS is retracted radially, and the small FDS is retracted ulnarly. This exposes the four FDP tendons.
Postoperative Care and Expected Outcomes
 A protective dorsal blocking splint is provided that keeps the MCP joint in 60 to 70 degrees of flexion and the wrist in neutral position. The patient is allowed to actively move the IP joints.
A protective dorsal blocking splint is provided that keeps the MCP joint in 60 to 70 degrees of flexion and the wrist in neutral position. The patient is allowed to actively move the IP joints.
 Ten days after surgery, the wound is inspected, sutures are removed, and the protective splint is maintained for another 4 weeks. Thereafter, the splint is removed, and the patient is allowed unrestricted activity.
Ten days after surgery, the wound is inspected, sutures are removed, and the protective splint is maintained for another 4 weeks. Thereafter, the splint is removed, and the patient is allowed unrestricted activity.
 This procedure should be performed before claw correction, and patients should be warned that the surgery will exaggerate the claw deformity.
This procedure should be performed before claw correction, and patients should be warned that the surgery will exaggerate the claw deformity.
Hastings H, McCollam SM. Flexor digitorum superficialis lasso tendon transfer in isolated ulnar nerve palsy: a functional evaluation. J Hand Surg [Am]. 1994;19:275-280.
Ozkan T, Ozer K, Gulgonen A. Three tendon transfer methods in reconstruction of ulnar nerve palsy. J Hand Surg [Am]. 2003;28:35-43.
Smith RJ. Extensor carpi radialis brevis tendon transfer for thumb adduction: a study of power pinch. J Hand Surg [Am]. 1983;8:4-15.
Trevett MC, Tuson C, de Jager LT, Juon JM. The functional results of ulnar nerve repair: defining the indications for tendon transfer. J Hand Surg [Br]. 1995;20:444-446.