CASE 19 Coronary Dissection Involving the Aortic Root
Cardiac catheterization
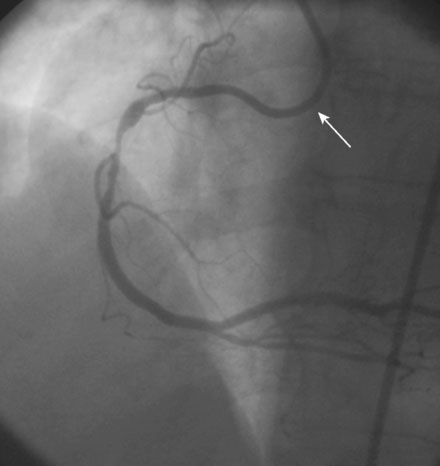
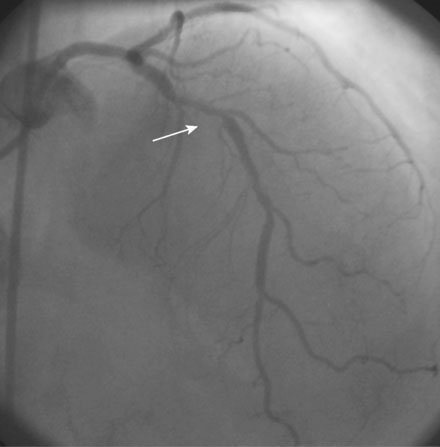
Diagnostic catheterization found normal left ventricular function and significant stenoses in the proximal segment of the right coronary artery (Figure 19-1 and Video 19-1) and in the left anterior descending artery (Figures 19-2, 19-3 and Video 19-2). The left circumflex artery appeared angiographically normal. Coronary calcification was noted in both the right coronary and left anterior descending arteries. After discussing the options of medical therapy, coronary bypass surgery, and percutaneous coronary intervention, the patient chose a percutaneous revascularization strategy.
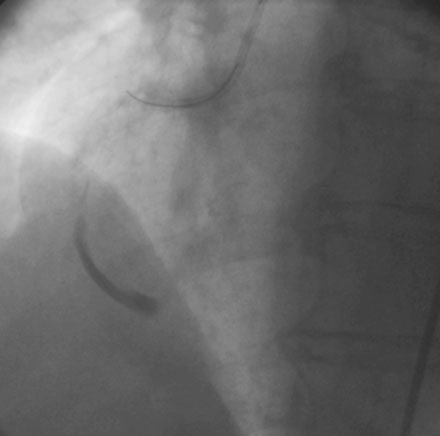
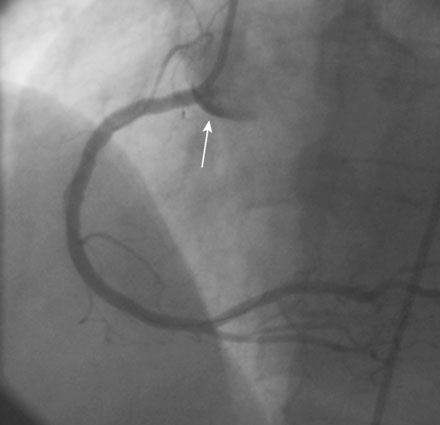
After administration of a bolus of 70 U/kg of unfractionated heparin followed by a double bolus and infusion of eptifibatide, the operator first approached the left anterior descending artery. The lesion was first dilated with a balloon and then treated with a sirolimus-eluting stent (Figure 19-4). The operator then turned attention to the right coronary artery. Anticipating the need for extra backup to support the intervention, due to the presence of coronary calcification noted on the diagnostic study, the operator chose a left Amplatz guide catheter (AL-2), as shown in Video 19-1. Although this guide catheter appeared to provide excellent support, pressure damping and retention of contrast in the arterial wall was observed in the proximal segment consistent with a guide-related dissection, leading to the exchange of the Amplatz guide for a right Judkins guide catheter. Upon engagement, the physician noted distal extension of the dissection, with retention of contrast nearly to the bifurcation of the posterior descending and posterolateral branches (Figure 19-5 and Video 19-3). The right coronary artery appeared to have reduced distal flow; ST-segment elevation was apparent on the monitored leads, and the patient reported severe substernal chest pain.
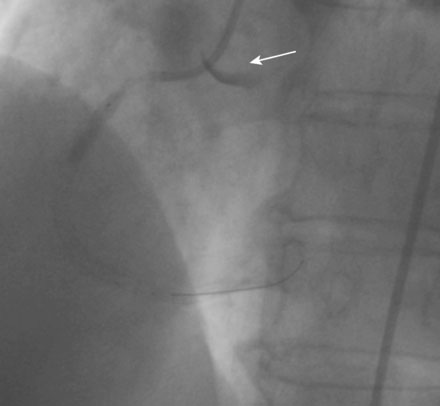
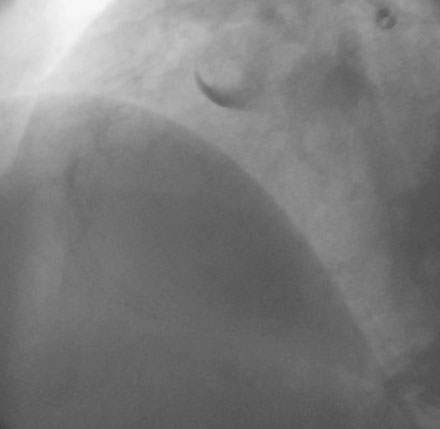
Fortunately, the 0.014 inch guidewire entered the true lumen distally and the physician was able to position a bare-metal stent, successfully sealing the distal extent of the dissection. Additional stents were placed in the midsection, successfully restoring flow to the distal right coronary artery and eliminating the patient’s chest discomfort and ST-segment changes. A substantial dissection remained in the proximal segment (Video 19-4). While deploying a stent in the proximal segment, the operator noted staining of the aortic cusp, suggesting that the dissection had propagated to the aorta (Figure 19-6). A final stent was placed to cover the ostium. The final angiographic result was excellent, but a large arc of contrast retention was noted in the aortic cusp (Figure 19-7 and Videos 19-5, 19-6). The patient remained asymptomatic except for mild residual chest discomfort, and suffered no hemodynamic consequences. Repeat angiography 15 minutes later showed patency of the artery but persistent contrast staining in the aorta (Figure 19-8).
Discussion
The development of an aortic dissection complicating a coronary dissection is very rare. A review of iatrogenic aortic dissection due to catheterization or coronary intervention found 9 cases out of 43,143 catheterizations (which included 20,475 coronary interventions) for an incidence of 0.02%.1 In this largest series to date, the authors described three types of dissection. Type I involved only the aortic cusp, similar to the example shown in this case. Type II involved the aortic cusp and extended up the aorta less than 40 mm, and Type III extended up the aorta greater than 40 mm. Similar to the case described here, all 9 events reported in this series involved the right coronary artery; the authors also comment that, of the 17 previously reported cases in the literature, 15 involved arose from a dissection in the right coronary artery. Also of note, the authors found that 44% of cases involved the use of an Amplatz catheter. Outcomes were excellent for Type I and II dissections but were poor for Type III dissections. Thus, if the aorta is involved in a limited manner, then optimal management consists of stenting of the dissection at its entry. Extensive involvement of the aorta (greater than 40 mm up the aorta), may require surgical intervention.