CHAPTER 19 Anesthesia Circuits and Ventilators
3 Give an example of a semiopen circuit
The various semiopen circuits were fully described by Mapleson and are commonly known as the Mapleson A, B, C, D, E, and F circuits (Figure 19-1). All have in common a source of fresh gas, corrugated tubing (more resistant to kinking), and a pop-off or adjustable pressure-limiting valve. Differences among the circuits include the locations of the pop-off valve, fresh gas input, and whether or not a gas reservoir bag is present. Advantages of the Mapleson series are simplicity of design, ability to change the depth of anesthesia rapidly, portability, and lack of rebreathing of exhaled gases (provided the fresh gas flow is adequate). Disadvantages include lack of conservation of heat and moisture, limited ability to scavenge waste gases, and high requirements for fresh gas flow. These are rarely used today except for patient transport.
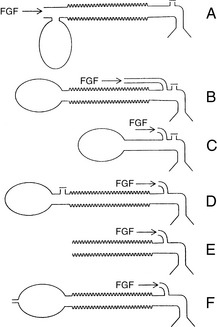
Figure 19-1 Mapleson A, B, C, D, E, and F circuits. FGF, Fresh gas flow.
(From Willis BA, Pender JW, Mapleson WW: Rebreathing in a T-piece: Volunteer and theoretical studies of the Jackson-Rees modification of Ayre’s T-piece during spontaneous respiration, Br J Anaesth 47:1239–1246, 1975, with permission.)
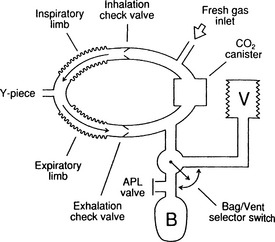
4 Give an example of a semiclosed circuit
The prototypical semiclosed circuit is the circle system, which is found in most operating rooms in the United States (Figure 19-2). Every semiclosed system contains an inspiratory limb, expiratory limb, unidirectional valves, carbon dioxide (CO2) absorber, gas reservoir bag, and a pop-off valve on the expiratory limb. Advantages of a circle system include conservation of heat and moisture, the ability to use low flows of fresh gas (thereby conserving volatile anesthetic and the ozone layer), and the ability to scavenge waste gases. A disadvantage is its complex design; it has approximately 10 connections, each of which has the potential for disconnection.
11 How do you know when the absorbent has been exhausted? What adverse reactions can occur between volatile anesthetic and CO2 absorbants?
A pH-sensitive dye added to the granules changes color in the presence of carbonic acid, an intermediary in the CO2 absorption chemical reaction. The most common dye in the United States is ethyl violet, which is white when fresh and turns violet when the absorbent is exhausted. Adverse reactions between volatile anesthetics and absorbants are discussed in Chapter 10.
13 How do anesthesia ventilators differ from intensive care unit ventilators?
Intensive care unit (ICU) ventilators usually are more powerful (allowing greater inspiratory pressures and tidal volumes, which is important in patients with decreased pulmonary compliance) and support more modes of ventilation. However, new generations of anesthesia machines continue to offer more ventilatory modes. See Chapter 21.
17 What parameters can be adjusted on an anesthesia ventilator?
Most anesthesia ventilators allow adjustment of:
KEY POINTS: Anesthesia Circuits and Ventilators 
22 When using very low flows of fresh gas, why is there sometimes a discrepancy between inspired oxygen concentration and fresh gas concentration?
1. Brockwell R.C., Andrews J.J. Inhaled anesthetic delivery systems. In: Miller R.D., editor. Miller’s anesthesia. ed 6. Philadelphia: Elsevier Churchill Livingstone; 2005:273-316.
2. Dorsch J.A., Dorsch S.E. Understanding anesthesia equipment, ed 5. Philadelphia: Lippincott Williams & Wilkins, 2008.