CASE 186
History: A 51-year-old man presents with dysphagia.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the most common systemic disorder that may be complicated by esophageal motility dysfunction?
3. What is the most common gastrointestinal (GI) manifestation of paraneoplastic syndrome?
4. What is the most common malignancy that gives rise to paraneoplastic syndrome?
ANSWERS
CASE 186
Paraneoplastic Syndrome
1. A, D, and E
2. B
3. D
4. A
References
Rutherford GC, Dineen RA, O’Connor A. Imaging in the investigation of paraneoplastic syndromes. Clin Radiol. 2007;62(11):1021-1035.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 27.
Comment
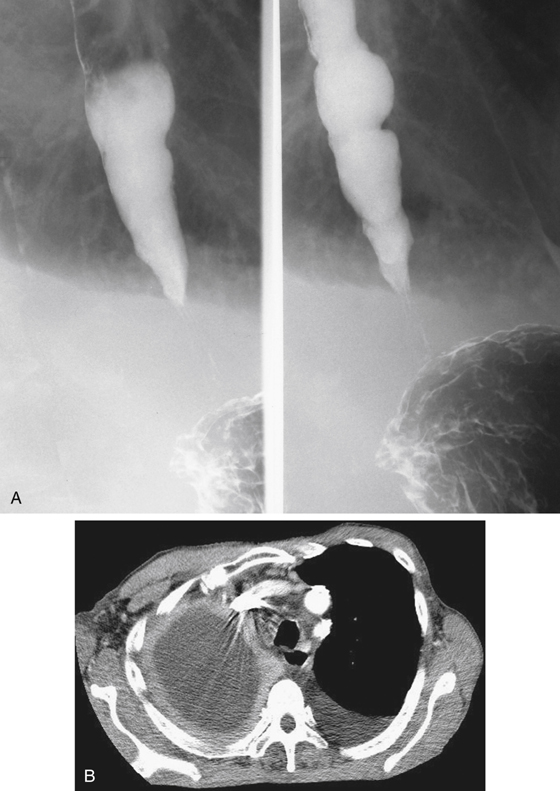
In some malignant conditions, secondary (nonmetastatic) systemic effects can be seen accompanying primary malignant disease. The achalasialike appearance of the esophagus, as seen in this case, is an example and is most commonly seen in patients with small cell carcinoma of the lung (see figures). However, paraneoplastic syndromes may encompass much more than the neuromuscular functions of the esophagus. They can affect skin, muscle, joints, kidneys, and endocrine function. Some cases of scleroderma have been determined to be a paraneoplastic syndrome, secondary to a primary lesion elsewhere in the body.
The exact mechanism of paraneoplastic manifestations is not well understood. The tumors may excrete hormones, which affect a specific target organ. There is considerable discussion in the literature of tumor antibodies produced by the body to resist the tumor but that have a secondary effect in the body. The presentation of a patient who has carcinoma of the lung with concomitant achalasialike symptoms and findings is uncommon but is not rare. Other GI manifestations of paraneoplastic syndrome have been reported, including malabsorption in the small bowel (the most common manifestation according to some) and unexplained diarrhea.
GI manifestations of paraneoplastic syndrome are of great interest and the subject of considerable research. It is possible that the problem is much larger than is appreciated at the present time. Although lung tumors have been mostly shown to be involved with paraneoplastic syndromes, more recent work has shown that malignancies from almost every body system have that capability. Imaging may be used to show either the primary lesions or paraneoplastic manifestations. However, most of the paraneoplastic effects have been detected by laboratory studies.