CHAPTER 18. URETHRAL CATHETERIZATION
Sushruta, a surgeon of ancient India (circa 6th century BC), described gold, silver, iron and wood tubes lubricated with ghee for the evacuation of urine. Aulus Cornelius Celsus (25 BC–AD 50) described bronze and lead pipes for urethral catheterization in De Re Medicina. Frederick Foley, a medical student in Boston, designed the modern catheter in the 1930s. Fortunately catheters now come in latex, silicone, Teflon and PVC, with some coated in silver alloy to reduce catheter-related infection.
INTRODUCTION
Catheterization is an invasive procedure. It should be carried out in a sensitive manner, maintaining the patient’s dignity at all times. The indication of catheterization determines whether long- or short-term catheters are used and should be considered prior to the procedure.
MALE CATHETERIZATION
INDICATIONS
• Acute urinary retention.
• Haematuria.
• Accurate assessment of urinary output (a measure of organ perfusion) and volume status (e.g. in circulatory shock or acute renal failure).
 Tip Box
Tip Box
A three-way catheter may be required if the indication is urinary retention due to clots (clot-retention). The same technique for catheter insertion as described above applies, with bladder irrigation being delivered via a third catheter lumen.
CONTRAINDICATIONS
• Lack of consent.
• Phimosis/paraphinosis (a relative contraindication).
• Urethral stricture.
• Penile fracture.
EQUIPMENT
• Dressing pack.
• Male catheter.
• Catheter drainage bag.
• Normal saline cleaning solution.
• Gauze.
• Sterile lidocaine anaesthetic gel (e.g. Instillagel®).
• 10 mL sterile water.
• 10 mL syringe.
• Sterile gloves.
• Disposable, loose-fitting outer sterile gloves.
• Kidney bowl.
CATHETER SIZE
Urethral catheters are measured in charrières (ch) after the 19th century French instrument maker Joseph Charrières, representing the outer diameter of the catheter. The size of the catheter in charrières is equivalent to three times its diameter in millimetres (mm): for example, a 12 ch catheter measures 4 mm in diameter. These measurements are commonly referred to as ‘French gauge’. A larger-gauge catheter may be required in circumstances such as haematuria or pyuria, where clots or debris may obstruct urinary flow. In these cases a three-way catheter may be required, with bladder irrigation being delivered via a third catheter lumen to maintain catheter patency. Larger catheters are more likely to cause urethral damage, but too small a catheter can result in leakage around the catheter. Various types are available: Foley, Coude tip (elbow shaped at the tip for negotiating the prostate) and straight. The smallest Foley catheter likely to be effective is normally first choice for general use, usually size 10, 12 or 14 ch in adults.
 Tip Box
Tip Box
If the catheter will not pass down the urethra (commonly due to an enlarged prostate or urethral stricture), consider using more anaesthetic gel and inserting a larger-sized catheter. Paradoxical though this may seem, a larger catheter will be less flexible in the urethra and hence more likely to negotiate the tighter prostatic urethra. However, never apply substantial force when inserting a catheter; if the catheter does not pass (secondary to a stricture, for example) withdraw the catheter and discuss with a urologist.
PRACTICAL PROCEDURE
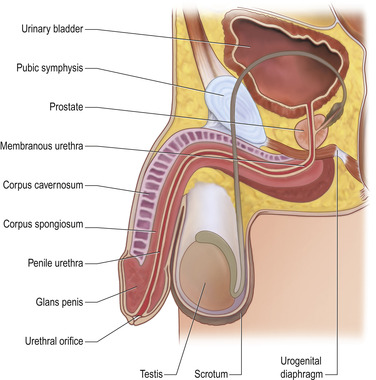 |
| Fig. 18.1. |
| Cross-section of male urogenital anatomy. |
• Explain the procedure to the patient and gain consent.
• Wash your hands and wear sterile gloves with a second overlying pair of disposable sterile gloves.
• Fill a syringe with 10 mL sterile water.
• Hold the penis with a sterile gauze swab around the shaft with your non-dominant hand.
• Retract the foreskin and gently cleanse the urethral meatus with gauze soaked in normal saline, directing the wiping motion away from the urethra.
• Place sterile drapes over the exposed groin and make a hole in the drape to place the penis through.
• Gently insert the pre-filled lidocaine gel syringe tip into the urethral meatus of the penis.
• Warn the patient of a stinging sensation and slowly insert 10 mL of the lidocaine gel.
• Dispose of the outer gloves.
• Expose the catheter tip from the inner packaging by tearing the perforations and gently insert the catheter into the urethral meatus with your dominant hand, holding it through its inner package.
• As you advance the catheter using a twisting or rotating motion continue to release it from its inner package by tearing the perforations hence maintaining a ‘non-touch technique’.
• Advance the full length of the catheter to its bifurcation and place a kidney bowl between the patient’s legs.
• Remove the last of the inner packaging and attach the catheter bag.
• Once urine is draining, inflate the balloon with 10 mL of sterile water.
• Gently pull back the catheter until resistance is felt and it resumes a fixed position (i.e. the catheter balloon is at the bladder neck).
• Pull forward the penile foreskin (to prevent paraphimosis).
• Wipe off any excess lidocaine gel.
• The catheter bag should hang below pelvis level to avoid retrograde flow and catheter-borne infections.
• Record the date and time the catheter was inserted in the patient’s medical notes.
— the type and size of catheter used
— the volume of sterile water used to inflate the catheter balloon
— the residual volume
— post-procedure investigations and complications.
FEMALE CATHETERIZATION
INDICATIONS
• Acute retention of urine.
• Haematuria.
• Accurate assessment of urinary output (a measure of organ perfusion) and volume status (e.g. in circulatory shock or acute renal failure).
CONTRAINDICATIONS
• Lack of consent.
EQUIPMENT
• Dressing pack.
• Female catheter.
• Catheter drainage bag.
• Normal saline cleaning solution.
• Gauze.
• Sterile lidocaine anaesthetic gel (e.g. Instillagel®).
• 10 mL sterile water.
• 10 mL syringe.
• Sterile gloves.
• Disposable, loose-fitting outer sterile gloves.
• Kidney bowl.
PRACTICAL PROCEDURE
• Explain the procedure to the patient and gain consent.
• Position the patient supine on the bed with their legs bent and then relaxed open, exposing the perineum (take care when positioning patients with prosthetic hip or knee replacements). Ensure that the perineum is well lit (e.g. using a gynaecology bedside lamp).
• Open the equipment onto a clean trolley, ensuring the urinary catheter remains inside the internal packaging.
• Wash your hands and wear sterile gloves with a second overlying pair of disposable sterile gloves.
• Fill a syringe with 10 mL sterile water.
• Part the labia with the fingers of your non-dominant hand. Using your dominant hand gently cleanse the perineum with gauze soaked in sterile normal saline wiping from anterior to posterior (i.e. towards the anus to avoid introducing microbes from this region).
• Place sterile drapes over the groin leaving the perineum exposed.
• Dispose of the outer gloves.
• Expose the catheter tip from the inner packaging by tearing the perforations and apply 2–3 mL of lidocaine gel.
• Part the labia with the fingers of your non-dominant hand, and gently insert the catheter into the urethra with your dominant hand holding it through its inner package.
• As you advance the catheter continue to release it from its inner package by tearing the perforations, hence maintaining a ‘non-touch technique’.
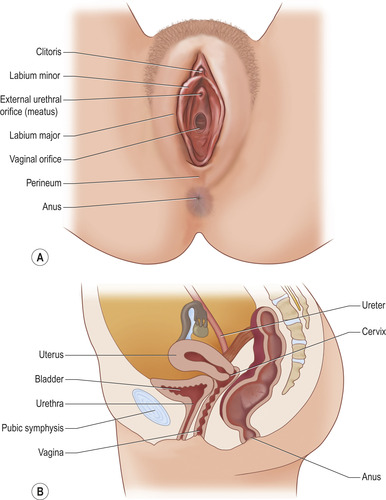 |
| Fig. 18.2. |
| (A) External anatomy of the female urogenital area. (B) Cross-section of female urogenital anatomy. |
 Tip Box
Tip Box
If resistance is felt while attempting to advance the catheter, ask the patient to relax and take deep breaths or cough and slowly pass the catheter using a twisting or rotating motion. These manoeuvres aim to alleviate the perineal muscle spasm that commonly hinders passage of the urethral catheter.
• Remove the last of the inner packaging and attach the catheter bag.
• Once urine is draining, inflate the balloon with 10 mL of sterile water.
• Gently pull back the catheter until resistance is felt and it resumes a fixed position (i.e. the catheter balloon is at the bladder neck).
• Wipe away any excess lidocaine gel.
• The catheter bag should hang below pelvis level to avoid retrograde flow and catheter-borne infections.
• Record the date and time the catheter was inserted in the patient’s medical notes. Note:
— the type and size of catheter used
— the volume of sterile water used to inflate the catheter balloon
— the residual volume
— post-procedure investigations and complications.
 Tip Box
Tip Box
The absence of urine on inserting the catheter its full length to the bifurcation implies one of two possibilities: an empty bladder or insertion into a false passage. Try to flush the catheter with 50 mL of sterile normal saline using a bladder syringe. If this flushes easily and can subsequently be aspirated, it is most likely that the catheter tip is situated in the bladder. If, however, doubt remains then remove the catheter and discuss with a urologist.
 Tip Box
Tip Box
Antibiotic cover is likely to be required when changing a catheter due to catheter-associated urinary tract infection. Consult with local protocols or microbiology for advice as to specific antimicrobials.
POST-PROCEDURE INVESTIGATIONS
• Catheter sample urine for urine dip and microscopy, culture and sensitivity.
• Urine output on a fluid balance chart.
COMPLICATIONS
• Local discomfort – offer topical lidocaine gel and simple oral analgesia.
• Catheter-associated urinary tract infection (or abscess formation reported with large-gauge catheters).
• Stricture formation or the formation of a false passage.
• Slowing of urine/no urine post catheter insertion:
— secondary to catheter blockage (e.g. debris from pyuria or excess anaesthetic gel occluding catheter tip)
— empty bladder
— haematuria (clots blocking catheter).
In these circumstances consider flushing the catheter with 50 mL sterile normal saline or a three-way catheter (see tip Boxes).