Procedure 18 Tendon Transfers for Carpal Tunnel Syndrome
![]() See Video 14: Tendon Transfer for Anterior Interosseous Nerve Palsy (FDS to FPL)
See Video 14: Tendon Transfer for Anterior Interosseous Nerve Palsy (FDS to FPL)
Examination/Imaging
Clinical Examination
 Sensation: It is important to document the level of sensation in the thumb and fingers preoperatively. Patients may also have diminished sensation in the ulnar nerve distribution. The potential functional benefit of a tendon transfer will be diminished in a patient with sensory loss, and these patients must be counseled about the likely poorer outcome after surgery.
Sensation: It is important to document the level of sensation in the thumb and fingers preoperatively. Patients may also have diminished sensation in the ulnar nerve distribution. The potential functional benefit of a tendon transfer will be diminished in a patient with sensory loss, and these patients must be counseled about the likely poorer outcome after surgery.
 Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the thumb metacarpophalangeal (MCP) joint and the thumb carpometacarpal (CMC) joint. It is not uncommon for patients to have basal joint arthritis with a supination and adduction deformity of the thumb and first web-space contracture. This should be addressed before a tendon transfer is considered.
Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the thumb metacarpophalangeal (MCP) joint and the thumb carpometacarpal (CMC) joint. It is not uncommon for patients to have basal joint arthritis with a supination and adduction deformity of the thumb and first web-space contracture. This should be addressed before a tendon transfer is considered.
 Motor: Many motors have been described for opponensplasty. Our first preference is the palmaris longus (PL) followed by the extensor indicis proprius (EIP), if the PL is absent. We rarely use the flexor digitorum superficialis (FDS) of the ring finger because of the greater morbidity (weakening the power grip, risk for proximal interphalangeal [PIP] joint flexion contracture, swan-neck deformity) and because the soft tissue pulley attenuates over time. Although the tension fraction of PL (1.2%) and EIP (1%) is theoretically less than the combined tension fraction of abductor pollicis brevis (APB) (1.1%) and opponens pollicis (OP) (1.9%), the transfer only needs enough strength to position the thumb in abduction.
Motor: Many motors have been described for opponensplasty. Our first preference is the palmaris longus (PL) followed by the extensor indicis proprius (EIP), if the PL is absent. We rarely use the flexor digitorum superficialis (FDS) of the ring finger because of the greater morbidity (weakening the power grip, risk for proximal interphalangeal [PIP] joint flexion contracture, swan-neck deformity) and because the soft tissue pulley attenuates over time. Although the tension fraction of PL (1.2%) and EIP (1%) is theoretically less than the combined tension fraction of abductor pollicis brevis (APB) (1.1%) and opponens pollicis (OP) (1.9%), the transfer only needs enough strength to position the thumb in abduction.
 The transfer of the PL (Camitz transfer) is typically performed for an elderly patient with CTS and severe thenar atrophy. The Camitz transfer is considered a “freebie” procedure because the incision used for CTS can be extended to the wrist in a zigzag fashion to obtain the PL augmented by the palmar fascia to attach into the ABP insertion at the radial MCP joint. As with any freebie procedure, however, the direction of tendon pull is not in line with the APB muscle but rather is more parallel to the forearm, which does diminish the biomechanical construct of this tendon transfer procedure. For an elderly patient with modest functional requirements, this transfer does serve the purpose of restoring some abduction and will permit the patient to recover acceptable thumb function.
The transfer of the PL (Camitz transfer) is typically performed for an elderly patient with CTS and severe thenar atrophy. The Camitz transfer is considered a “freebie” procedure because the incision used for CTS can be extended to the wrist in a zigzag fashion to obtain the PL augmented by the palmar fascia to attach into the ABP insertion at the radial MCP joint. As with any freebie procedure, however, the direction of tendon pull is not in line with the APB muscle but rather is more parallel to the forearm, which does diminish the biomechanical construct of this tendon transfer procedure. For an elderly patient with modest functional requirements, this transfer does serve the purpose of restoring some abduction and will permit the patient to recover acceptable thumb function.
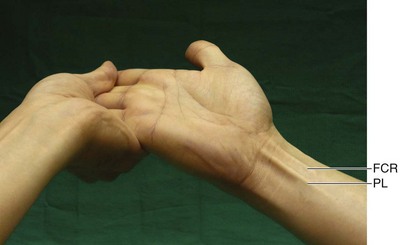
 We use the test described by Mishra to determine the presence of the PL. The traditional test described by Schaeffer requires the patient to abduct and oppose the thumb to the small finger and flex the wrist. A patient with thenar atrophy will find it difficult to do so. The Mishra test is performed by holding the patient’s wrist and fingers in hyperextension, while asking the patient to flex the wrist. This stretches the palmar aponeurosis and makes the PL taut when the patient attempts wrist flexion (Fig. 18-1).
We use the test described by Mishra to determine the presence of the PL. The traditional test described by Schaeffer requires the patient to abduct and oppose the thumb to the small finger and flex the wrist. A patient with thenar atrophy will find it difficult to do so. The Mishra test is performed by holding the patient’s wrist and fingers in hyperextension, while asking the patient to flex the wrist. This stretches the palmar aponeurosis and makes the PL taut when the patient attempts wrist flexion (Fig. 18-1).
Surgical Anatomy
 Thumb opposition is a complex movement produced by a combination of flexion, palmar abduction, and pronation and requires participation of both the MCP and CMC joints. The prime muscle of thumb opposition is believed to be the APB with contributions from the OP and flexor pollicis brevis (FPB).
Thumb opposition is a complex movement produced by a combination of flexion, palmar abduction, and pronation and requires participation of both the MCP and CMC joints. The prime muscle of thumb opposition is believed to be the APB with contributions from the OP and flexor pollicis brevis (FPB).
 The muscles affected after low median nerve palsy are the APB, OP, superficial head (radial head) of the FPB, and the radial two lumbricals (first and second). The first three muscles are innervated by the recurrent motor branch of the median nerve, whereas the latter two are innervated by the first and second common palmar digital nerve branch of the median nerve.
The muscles affected after low median nerve palsy are the APB, OP, superficial head (radial head) of the FPB, and the radial two lumbricals (first and second). The first three muscles are innervated by the recurrent motor branch of the median nerve, whereas the latter two are innervated by the first and second common palmar digital nerve branch of the median nerve.
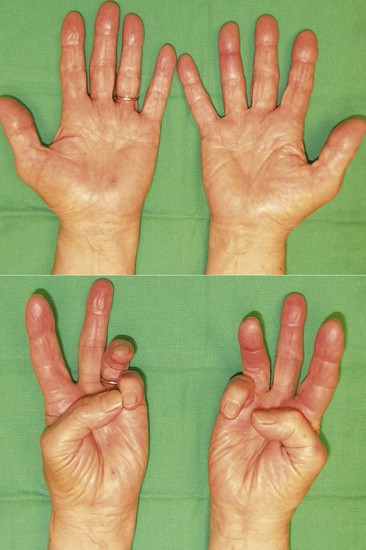
 Reasonable thumb abduction and opposition may be retained after isolated median nerve injury or severe carpal tunnel syndrome as a result of preserved ulnar nerve function (retained innervation of the deep head of the FPB and variability in thenar muscle innervation by connection between the ulnar and median nerves). Figure 18-2 shows the preoperative appearance of the hand with severe CST on the right. Note the thenar atrophy and inability to palmarly abduct the right thumb.
Reasonable thumb abduction and opposition may be retained after isolated median nerve injury or severe carpal tunnel syndrome as a result of preserved ulnar nerve function (retained innervation of the deep head of the FPB and variability in thenar muscle innervation by connection between the ulnar and median nerves). Figure 18-2 shows the preoperative appearance of the hand with severe CST on the right. Note the thenar atrophy and inability to palmarly abduct the right thumb.
 The midpalmar portion of the palmar aponeurosis has three layers: superficial longitudinal fibers, deeper transverse fibers, and deepest vertical fibers. Only the superficial longitudinal fascia is obtained in continuity with the PL to maximize the length of this tendon to reach the APB insertion.
The midpalmar portion of the palmar aponeurosis has three layers: superficial longitudinal fibers, deeper transverse fibers, and deepest vertical fibers. Only the superficial longitudinal fascia is obtained in continuity with the PL to maximize the length of this tendon to reach the APB insertion.
Positioning
 The procedure is performed under tourniquet control. It is usually performed under sedation and local anesthesia because this procedure is rather expedient and there is no need to take unnecessary anesthetic risk in elderly patients. The patient is positioned supine with the affected extremity on a hand table.
The procedure is performed under tourniquet control. It is usually performed under sedation and local anesthesia because this procedure is rather expedient and there is no need to take unnecessary anesthetic risk in elderly patients. The patient is positioned supine with the affected extremity on a hand table.
Exposures
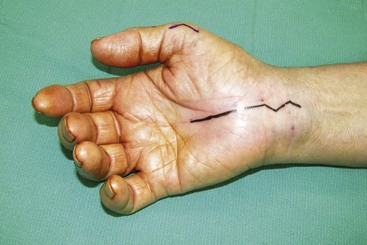
 An incision is made in line with the third web space extending from 1 cm proximal to the proximal palmar crease to a point 2 cm proximal to the wrist crease (Fig. 18-3).
An incision is made in line with the third web space extending from 1 cm proximal to the proximal palmar crease to a point 2 cm proximal to the wrist crease (Fig. 18-3).
 The incision is extended in a zigzag fashion at the wrist crease.
The incision is extended in a zigzag fashion at the wrist crease.
 The skin and subcutaneous tissue are dissected sharply with a no. 15 knife blade to expose the tendon of the PL in the distal forearm and the palmar aponeurosis in the palm (Fig. 18-4).
The skin and subcutaneous tissue are dissected sharply with a no. 15 knife blade to expose the tendon of the PL in the distal forearm and the palmar aponeurosis in the palm (Fig. 18-4).
 A second 2-cm longitudinal chevron-shaped incision is made over the dorsoradial aspect of the thumb MCP joint.
A second 2-cm longitudinal chevron-shaped incision is made over the dorsoradial aspect of the thumb MCP joint.
 The skin and subcutaneous tissue are dissected free to expose the tendon of the APB.
The skin and subcutaneous tissue are dissected free to expose the tendon of the APB.
Procedure
Step 1
 A 1- to 1.5-cm–wide strip of palmar aponeurosis is marked out and elevated from distal to proximal by maintaining continuity with the palmaris longus tendon over the carpal tunnel (Fig. 18-5).
A 1- to 1.5-cm–wide strip of palmar aponeurosis is marked out and elevated from distal to proximal by maintaining continuity with the palmaris longus tendon over the carpal tunnel (Fig. 18-5).
Step 1 Pearls
Identify the digital neurovascular bundles in the palm distal to the superficial transverse palmar ligament (thickening of the transverse fibers of the palmar aponeurosis between the proximal and distal palmar creases).
The previously marked segment of the palmar aponeurosis can be elevated in the plane superficial to the neurovascular bundle. This plane lies between the deeper vertical fibers of the palmar aponeurosis and the superficial transverse and longitudinal fibers.
It is better to elevate a longer and wider strip of palmar aponeurosis than what is required.
Step 1 Pitfalls
Elevating a structurally intact strip of palmar aponeurosis is the most challenging aspect of this procedure, and attention must be paid to maintaining the integrity of the palmar aponeurosis while protecting the underlying neurovascular structures.
Many small perforating vessels pass through the aponeurosis to supply the overlying soft tissue. They must be carefully cauterized to prevent postoperative hematoma.
Step 2
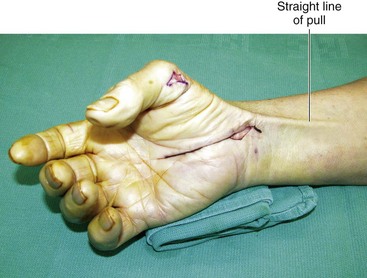
 The strip of palmar aponeurosis and contiguous PL tendon are pulled distally and freed from any tissue in the forearm that restricts movement of the PL (Fig. 18-6).
The strip of palmar aponeurosis and contiguous PL tendon are pulled distally and freed from any tissue in the forearm that restricts movement of the PL (Fig. 18-6).
Step 3
Step 4
 A wide subcutaneous tunnel is created between the thumb MCP joint incision and the distal forearm incision.
A wide subcutaneous tunnel is created between the thumb MCP joint incision and the distal forearm incision.
Step 5
 A hemostat passed from the thumb MCP joint through the subcutaneous tunnel is used to grasp the palmar aponeurosis extension of the PL and to bring it out from the thumb incision.
A hemostat passed from the thumb MCP joint through the subcutaneous tunnel is used to grasp the palmar aponeurosis extension of the PL and to bring it out from the thumb incision.
Step 5 Pearls
A grasping suture can be passed through the distal end of the palmar aponeurosis and left long before tunneling. The hemostat can hold the suture instead of the aponeurosis to minimize injury to the aponeurosis. The length of the suture will also allow retrieval of the tendon, should it inadvertently slip back into the tunnel.
Maintain the tendon hemostat until the aponeurosis is sutured to the APB.
Step 7
 With an assistant holding the wrist in neutral position and the thumb in full palmar abduction, the palmar aponeurosis is weaved through the tendon of the APB and sutured to itself and the APB using 4-0 Ethibond sutures.
With an assistant holding the wrist in neutral position and the thumb in full palmar abduction, the palmar aponeurosis is weaved through the tendon of the APB and sutured to itself and the APB using 4-0 Ethibond sutures.
Step 7 Pearls
Alternate insertion sites for opponensplasty include (1) a dual insertion on the APB and the dorsal capsule to stabilize the MCP joint passively in addition to providing opposition and (2) an insertion on the dorsoulnar aspect of the MCP joint to provide pronation by an insertion onto the extensor pollicis brevis (EPB). We believe that a dual insertion may not serve a dual function and that the transfer will predominantly act on the tighter insertion. Also, pronation occurs passively with thumb abduction. We therefore prefer a simple APB insertion in isolated low median nerve palsy.
It should be sutured with enough tension so that the thumb can be maintained in full palmar abduction with the wrist in neutral position after the assistant is no longer maintaining the position (Fig. 18-9). A single preliminary suture can be placed to determine whether the tension is appropriate.
Check the effect of wrist tenodesis on thumb abduction with the single suture in situ to determine whether the repair is too tight or too loose. When the tension has been set correctly, one should be able to place the thumb in the plane of the hand with the wrist flexed, and the thumb should be in full palmar abduction with slight flexion of the wrist. Setting of tension is an admirable goal, but the length of this tendon is barely sufficient to reach the ABP insertion. This situation is similar to EIP transfer in that it is unnecessary to be precise in setting the tension because the tension is already set by the just-enough length of the transferred tendon to reach the ABP insertion.
Postoperative Care and Expected Outcomes
 A thumb spica splint that maintains the thumb in full palmar abduction and the wrist in flexion is applied postoperatively. Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable thumb spica splint that the patient will wear for another 3 weeks (provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand). Thereafter, the patient is encouraged to move the thumb and is started on gradual strengthening exercises. A protective removable splint is also provided for night wear and general protection for the next 4 weeks. The protective splint is discontinued 2 months after surgery, and the patient is allowed unrestricted activity.
A thumb spica splint that maintains the thumb in full palmar abduction and the wrist in flexion is applied postoperatively. Ten days after surgery, the wound is inspected, sutures are removed, and the position is maintained using a removable thumb spica splint that the patient will wear for another 3 weeks (provided that the patient is reliable in keeping the splint on at all times, except in the daily cleaning of the hand). Thereafter, the patient is encouraged to move the thumb and is started on gradual strengthening exercises. A protective removable splint is also provided for night wear and general protection for the next 4 weeks. The protective splint is discontinued 2 months after surgery, and the patient is allowed unrestricted activity.
 The PL transfer (Camitz transfer) restores palmar abduction and is not a true opponensplasty. It gives good results in severe CTS because the patients may regain some opposition over time as a result of carpal tunnel release. It is usually not recommended for traumatic median nerve palsy when the PL is divided or scarred. Most authors have reported more than 90% restoration of thumb abduction with a Camitz transfer in severe CTS.
The PL transfer (Camitz transfer) restores palmar abduction and is not a true opponensplasty. It gives good results in severe CTS because the patients may regain some opposition over time as a result of carpal tunnel release. It is usually not recommended for traumatic median nerve palsy when the PL is divided or scarred. Most authors have reported more than 90% restoration of thumb abduction with a Camitz transfer in severe CTS.
Braun RM. Palmaris longus tendon transfer for augmentation of the thenar musculature in low median palsy. J Hand Surg [Am]. 1978;3:488-491.
Foucher G, Malizos C, Sammut D, et al. Primary palmaris longus transfer as an opponensplasty in carpal tunnel release: a series of 73 cases. J Hand Surg [Br]. 1991;16:56-60.
Terrono AL, Rose JH, Mulroy J, Millender LH. Camitz palmaris longus abductorplasty for severe thenar atrophy secondary to carpal tunnel syndrome. J Hand Surg [Am]. 1993;18:204-206.