Antiinflammatory, Musculoskeletal, and Antiarthritis Medications
Objectives
1. List medications commonly used for the treatment of minor musculoskeletal pain and inflammation.
2. Compare the actions of various antiinflammatory and muscle relaxant agents.
3. Identify the appropriate use for musculoskeletal relaxants.
4. Explain the mechanisms of action for different antiarthritis medications.
5. Describe adverse reactions frequently found in the use of antiarthritis medications.
6. Describe the clinical situations in which uricosuric therapy may be indicated.
Key Terms
arthritis (ărth-RĪ-tĭs, p. 324)
gout (gŏwt, p. 328)
nonsteroidal antiinflammatory drugs (NSAIDs) (p. 319)
osteoarthritis (ŏs-tē-ō-ărth-RĪ-tĭs, p. 324)
rheumatoid arthritis (RŪ-mă-tŏyd, p. 324)
salicylates (să-LĬS-ĭl-āts, p. 314)
skeletal muscle relaxants (SKĔL-ĭ-tăl, p. 321)
uric acid (Ū-rĭk, p. 328)
uricosuric agents (Ū-rĭ-kō-SŪR-ĭk, p. 328)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
This chapter includes the medications helpful in treating problems affecting the bones, joints, muscles, and ligaments. There are many musculoskeletal disorders that cause pain, stiffness, and boney deformity. Powerful drugs are used for the more serious problems; safer over-the-counter (OTC) drugs are used for less serious conditions. Many acute problems, such as sprains, fractures, or tears, require only short-term therapy. Some disorders, such as arthritis, may require long-term therapy with simpler drugs used initially, advancing to advanced drugs as the pain and mobility problems increase. Most of these products—even the drugs sold OTC have serious adverse reactions, and patient response to therapy must be monitored closely.
This chapter is divided into four sections. The first section deals with antiinflammatory and analgesic medications such as the salicylates and nonsteroidal antiinflammatory drugs (NSAIDs), which are used to treat both minor and severe pain and common orthopedic problems. The second section presents skeletal muscle relaxants. The third section introduces a variety of medications used to treat arthritis, the disease-modifying antirheumatic medications (DMARDS) and immune modulators. Agents used to treat high uric acid levels found in gout are presented in the fourth section. These are all common conditions that licensed practical and vocational nurses see and medicines they use frequently.
Muscular and Skeletal Systems
The muscular and skeletal systems work together to provide support and movement for the body (Figures 18-1 and 18-2). The skeletal system is made up of the bones, cartilage, ligaments, and joints, and the muscular system is those muscles attached to the skeleton.
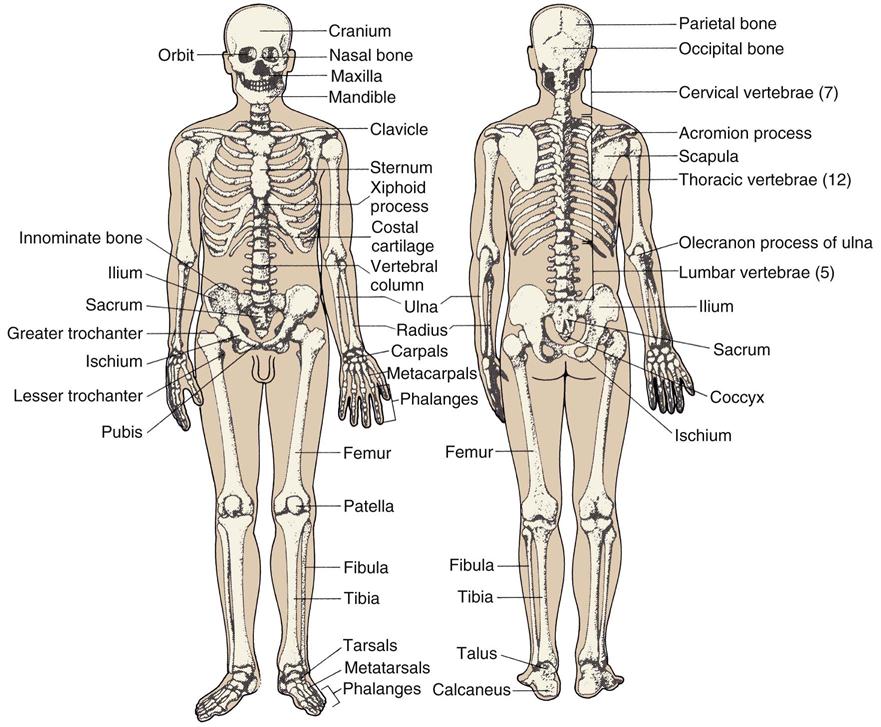
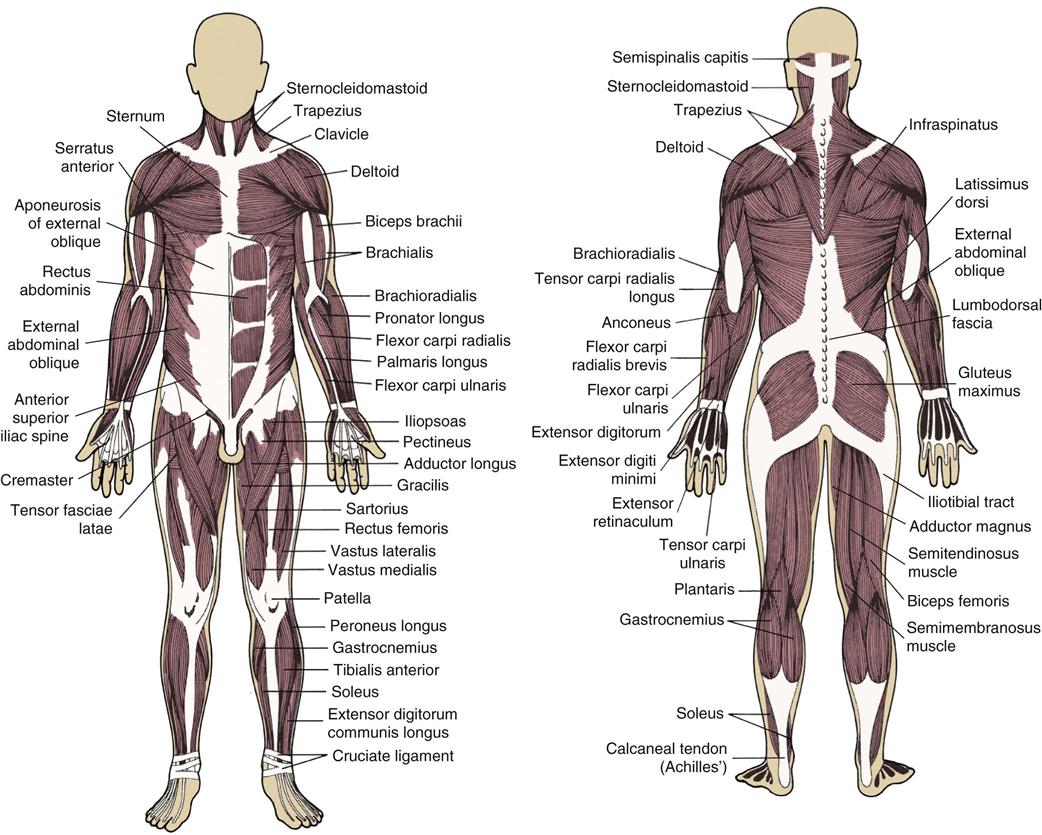
The skeleton protects, supports, and allows body movement, produces blood cells in the long bones, and stores minerals. The muscular system helps the body parts move, holds the body upright, and produces body heat.
Disease may attack just a small part of the body or the whole muscular and skeletal system. Injuries are often due to trauma, wear over many years, or overuse. Although some traumatic skeletal injuries heal well, some injury sites may continue to have pain and deformity.
The Inflammatory Response
The inflammatory response is necessary for the body’s survival when faced with stress or injury. A number of things can trigger the inflammatory response. These include infectious agents, ischemia (lack of blood supply to a tissue), antigen-antibody interactions, and thermal (heat or cold) or other injury. The inflammatory response has three phases:
2. A delayed, subacute infiltration (movement) of leukocytes and phagocytic cells into the tissue
3. Chronic proliferative tissue degeneration (breakdown) and fibrosis
The inflammatory response of the body produces the symptoms of erythema (redness or irritation), edema (fluid buildup in the body tissues), tenderness, and pain. This happens when the affected blood cells release a variety of inflammatory mediators (substances that continue the inflammatory response). The inflammatory mediators act to increase blood flow to the area and increase capillary permeability, allowing movement of large molecules across cell walls into the site. One of the most important inflammatory mediators is histamine, which causes vasodilation to increase blood flow to the area. Cytokines help control the inflammatory process. Prostaglandins also have a role in the inflammatory reaction.
Prostaglandins have several actions in the body. The useful functions of prostaglandins have to do with “housekeeping” actions in the tissues, especially in protecting the mucosa of the gastrointestinal (GI) tract. They also maintain normal renal function, platelet aggregation (clumping together), consciousness and mental functions in the brain, and temperature. Prostaglandins also cause erythema and an increase in local blood flow, and they can remove the vasoconstrictor effects of substances such as norepinephrine and angiotensin. These actions of prostaglandins are controlled by a series of reactions at sites of tissue injury and inflammation. Prostaglandins are helpful when they are kept in check, but harmful when they are not.
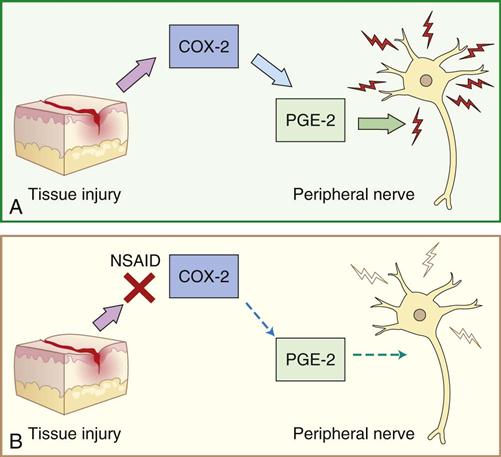
The housekeeping functions of prostaglandins are controlled by cyclooxygenase-1 (COX-1). Cyclooxygenase-2 (COX-2) is created where there is inflammation caused by cytokines and other inflammatory mediators. It is also found in the brain, where it plays a role in fever and perception of pain. COX-2 is an active participant in the inflammatory process and produces harmful results in the body if not controlled.
Although it is important to have medications that can block the harmful actions of prostaglandins, the important physiologic functions of prostaglandins that are helpful in the body must be preserved. Most antiinflammatory drugs block the actions of both COX-1 and COX-2. A group of drugs known as COX-2 inhibitors or blockers was developed to reduce the inflammatory response in some tissues without destroying the tissue of the GI tract (Figure 18-3). Although these drugs reduce the incidence of gastric bleeding, current research suggests that they may do so at the expense of the heart. All but one of these drugs have been removed from the market because of this problem.
Antiinflammatory and Analgesic Agents
Overview
Aspirin is one of the most commonly taken medications. The ease with which it can be bought and the fact that people decide when and if they need it should not decrease the importance given to this drug in treating common and significant musculoskeletal problems. Aspirin (acetylsalicylic acid [ASA]) has greater antiinflammatory action than other salicylates and is preferred in the treatment of many problems. Acetaminophen is also used for analgesia in generalized pain and arthritis because of its safety. Acetaminohen is an analgesic but not an NSAID because it has no antiinflammatory properties. The NSAIDs are powerful agents to help decrease pain and inflammation. Prostaglandins may make peripheral pain receptors more sensitive to painful stimuli. Both salicylates and NSAIDs are thought to limit the production of prostaglandins.
Salicylates
Action
Salicylates have analgesic (pain-reducing), antipyretic (temperature-reducing), and antiinflammatory effects. It also has growing use as an emergency antiplatelet drug in patients who are having a myocardial infarction (MIs) or to prevent other MIs or strokes in men. Salicylates stop the production of prostaglandins, which affects the pain and inflammatory processes through a depressant effect on the central and peripheral pain receptors. They do this by blocking the production of cyclooxygenase, an enzyme that is necessary for the production of prostaglandins.
Uses
Aspirin is stronger or more potent in stopping prostaglandin synthesis than are other salicylates, and it has greater antiinflammatory effects. Aspirin is used in the treatment of mild to moderate pain. Aspirin is the only drug in this category to slow the clumping of platelets for the life of the platelet (7 to 10 days). It also interferes with factor III of the clotting mechanism. This makes it useful in reducing the risk for strokes or for treating transient ischemic attacks (TIAs) in patients who have had some types of TIAs. However, it is of no benefit for men who have already had strokes. Research shows that aspirin does not seem to prevent TIAs or strokes in women.
Small daily doses of aspirin are also used to reduce the risk of death or nonfatal MI in patients with previous infarction or unstable angina pectoris. Lower doses are just as effective and have fewer side effects than higher doses for this purpose. Unlabeled uses of aspirin in low doses also include prevention of colorectal cancer and preeclampsia.
Salicylates are used as first-line therapy to treat various forms of arthritis (rheumatoid arthritis, osteoarthritis, degenerative joint disease) through inhibition of cyclooxygenase (COS). The inflammatory and analgesic effects of aspirin are roughly equivalent to those of many other NSAIDS. Their use has declined somewhat with the option of NSAIDS. They are used to treat fever produced by bacterial illnesses and in therapy for pain from trauma to soft tissue or muscle. Pain in the muscles, nerves, and joints (myalgias, neuralgias, and arthralgias), as well as headache and dysmenorrhea, are also treated with salicylates. The antiinflammatory effects are useful in treating systemic lupus erythematosus, acute rheumatic fever, and similar conditions. An aspirin should be chewed immediately by any patient suspected of having an acute MI to help limit tissue damage.
Adverse Reactions
The greatest concern in use of aspirin for chronic disease is the production of GI distress and bleeding. Bleeding may often occur suddenly and without pain. It is estimated that a normal person taking Aspirin loses 10 mL of blood every day from minor GI irritation. Hypersensitivity (allergy) is also common and may produce anaphylaxis. In those with allergy, there may also be cross-sensitivity to other medications, including NSAIDS and acetaminophen. Other adverse reactions to antiinflammatory analgesics include tinnitus (ringing in the ears), visual disturbances, edema, urticaria (hives), rashes, anorexia (lack of appetite), epigastric discomfort, and nausea. Aspirin has been associated with the occurrence of Reye syndrome when given to children with varicella (i.e. chickenpox) or influenza. In Reye syndrome, symptoms may affect all organs of the body, but most seriously affects the brain and liver. Rapid development of severe neurological symptoms, including lethargy, confusion, seizures, and coma, make Reye syndrome a life-threatening emergency. Most authorities advise against the use of aspirin in these and other viral infections. In overdosage, symptoms may progress from mild to severe, beginning with hyperventilation, diaphoresis (sweating), thirst, headache, drowsiness, skin eruptions, and electrolyte imbalance, and progressing to central nervous system (CNS) depression, stupor, convulsions and coma, tachycardia (rapid heartbeat), and respiratory insufficiency. Respiratory and metabolic acidosis are most often seen in children.
Drug Interactions
Alcohol taken with any of the antiinflammatory analgesics increases the chance of GI bleeding. There is an increased effect of anticoagulants, sulfonylureas, and sulfonamides if they are used at the same time as salicylates. Ascorbic acid increases the effect of salicylates by increasing renal tubular reabsorption. Salicylates interact with other NSAIDs to increase effects, side effects, and toxicities. Salicylates also increase or potentiate the effects of phenytoin (Dilantin) and inhibit hyperuricemia produced by pyrazinamide. Salicylates can affect the results of many laboratory test results.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn all possible details about the patient’s health history. Check for the presence of allergy to aspirin or other NSAIDs, history of asthma or nasal polyps, GI problems or ulcer disease, current use of other drugs that may cause interactions, or other hepatic or renal disease. These conditions are precautions or contraindications to the use of salicylates.
The health care provider may ask the nurse to get a stool specimen to check for occult blood before beginning the medication. This will help decide whether or not the patient had bleeding in the stool before the medication was started.
n Diagnosis
Careful attention should be paid to other medications and disease processes of the patient. Are there conditions that would make the use of NSAIDs or salicylates dangerous? What is the risk for GI bleeding in this patient? How much caffeine, alcohol, or tobacco does this patient use? Are there other problems related to weight, mobility, safety, or nutrition?
n Planning
Antiinflammatory analgesics should not be used in patients with hepatic (liver) disease. Patients on anticoagulant therapy or with blood clotting problems must be very careful when they use these products. These drugs also should not be used before surgery (because of their effect on platelet aggregation) or before labor (because bleeding may increase). They should be used with caution in patients with symptoms suggesting TIAs. In patients with musculoskeletal pain that persists for more than 10 days, further evaluation of the pain is needed.
Antiinflammatory analgesics should not be used during pregnancy, especially during the third trimester, because they may have adverse effects on the fetus. Salicylates are excreted in breast milk.
These drugs should be used carefully if the patient has gastric irritation, especially in patients with a past history of upper GI problem, blood dyscrasias, or decreased renal function.
Hydration (supply of fluids) should be monitored carefully in children, because they seem to be more likely to get salicylate intoxication or overdose.
Reye syndrome is an acute, life-threatening problem seen in children that produces vomiting and lethargy that may go on to delirium and coma with permanent brain damage and possible death. Use of aspirin after influenza, chickenpox, or other viral conditions in children seems to be closely related to the development of Reye syndrome and should be avoided.
Many salicylate products are not recommended for use in children younger than 12 years of age. When salicylates are ordered for children, check the specific drug to make certain that the product is safe for children.
n Implementation
The administration and dosage for each of the salicylate products vary. There are tablets, capsules, drops, chewable preparations, suppositories, and injectable forms of these products. Aspirin is the most active agent and has the greatest amount of salicylate per unit. Individual products should be checked for dosing specifics by age.
Patients (particularly poorer patients or immigrants) with diabetes who are testing their urine with Benedict’s Clinitest may get incorrect readings. They may need to switch to another form of urine testing while using salicylate products. Salicylates also increase the action of oral hypoglycemic agents, and patients with diabetes should be alert to signs of hypoglycemia (low blood sugar level).
A summary of dosing information for the salicylates is provided in Table 18-1.
![]() Table 18-1
Table 18-1
| GENERIC NAME | TRADE NAME | COMMENTS |
| Salicylates and Acetaminophen | ||
| acetaminophen |
Acephen Aceta Acetaminophen Apacet FeverAll Panadol Tempra 3 Tylenol |
Used as an analgesic-antipyretic in the presence of aspirin allergy and for patients with blood coagulation disorders being treated with oral anticoagulants, bleeding diatheses, upper GI disease, gastritis, hiatal hernia, and gouty arthritis. Also used for a variety of soft-tissue injuries and for acute pain relief. |
| acetylsalicylic acid (ASA, aspirin) |
Aspergum Bayer Ecotrin Empirin |
The most commonly used antiinflammatory agent. Standard against which all other agents are compared. Hypersensitivity often exists. |
| acetylsalicylic acid (ASA) buffered choline salicylate | Alka-Seltzer Ascriptin Bufferin |
Aspirin-antacid combinations are used in patients who experience GI distress from plain aspirin. Dosage and administration are the same as for plain aspirin. |
| diflunisal | Dolobid | Salicylic acid nonsteroidal derivative. |
| magnesium salicylate | Doan’s caplets | Sodium-free salicylate with lower incidence of GI problems than ASA. |
| salsalate | Amigesic Salflex |
Take in divided doses. |
| sodium salicylate | Sodium Salicylate | Comes in an enteric-coated pill. |
| Nonsteroidal Antiinflammatory Drugs | ||
| diclofenac | Cataflam Voltaren |
Used for chronic long-term therapy. Also comes in a delayed-release tablet. |
| fenoprofen | Nalfon | Administer medication 30 min before or 2 hr after meals; food interferes with absorption. |
| flurbiprofen | Ansaid | Used in rheumatoid arthritis and osteoarthritis. |
| ibuprofen |
Advil Motrin Nuprin |
Approved for use in the treatment of dysmenorrhea. Used in acute, chronic pain and for inflammatory processes. |
| indomethacin | Indocin | A potent prostaglandin synthesis inhibitor with significant toxic side effects; many adverse reactions (including blood dyscrasias) and drug interactions. Acute gouty arthritis. Take for 5 days, then reduce dosage. Patient should be weaned off medication as soon as possible. |
| ketorolac | Toradol | Given IM for short-term management of pain and orally for short duration. Do not use longer than 5 days. |
| meclofenamate | Has ability to block action of prostaglandins and inhibit their synthesis, whereas other NSAIDs only inhibit prostaglandin synthesis. | |
| mefenamic acid | Ponstel | Recommended for treatment of dysmenorrhea rather than arthritis or other acute musculoskeletal problems. |
| meloxicam | Mobic | Take with or without food. |
| naproxen | Aleve Anaprox Naprosyn |
Used for mild to moderate pain, rheumatoid arthritis, osteoarthritis, ankylosing spondylitis. Long-term therapy may require the higher dosage range. If no symptomatic effect in 2 wk, trial should be continued for 2 more wk before drug discontinued. Used to treat acute gout. |
| piroxicam | Feldene | Indicated in the treatment of acute exacerbations and long-term management of rheumatoid arthritis and osteoarthritis. |
| sulindac | Clinoril | Used for arthritis and ankylosing spondylitis, acute painful shoulder or gout. |
| Cyclooxygenase-2 Inhibitor | ||
| celecoxib | Celebrex | Used in osteoarthritis, rheumatoid arthritis, acute pain, and dysmenorrhea. Long-term use may damage heart. Do not use in patients allergic to sulfa. |
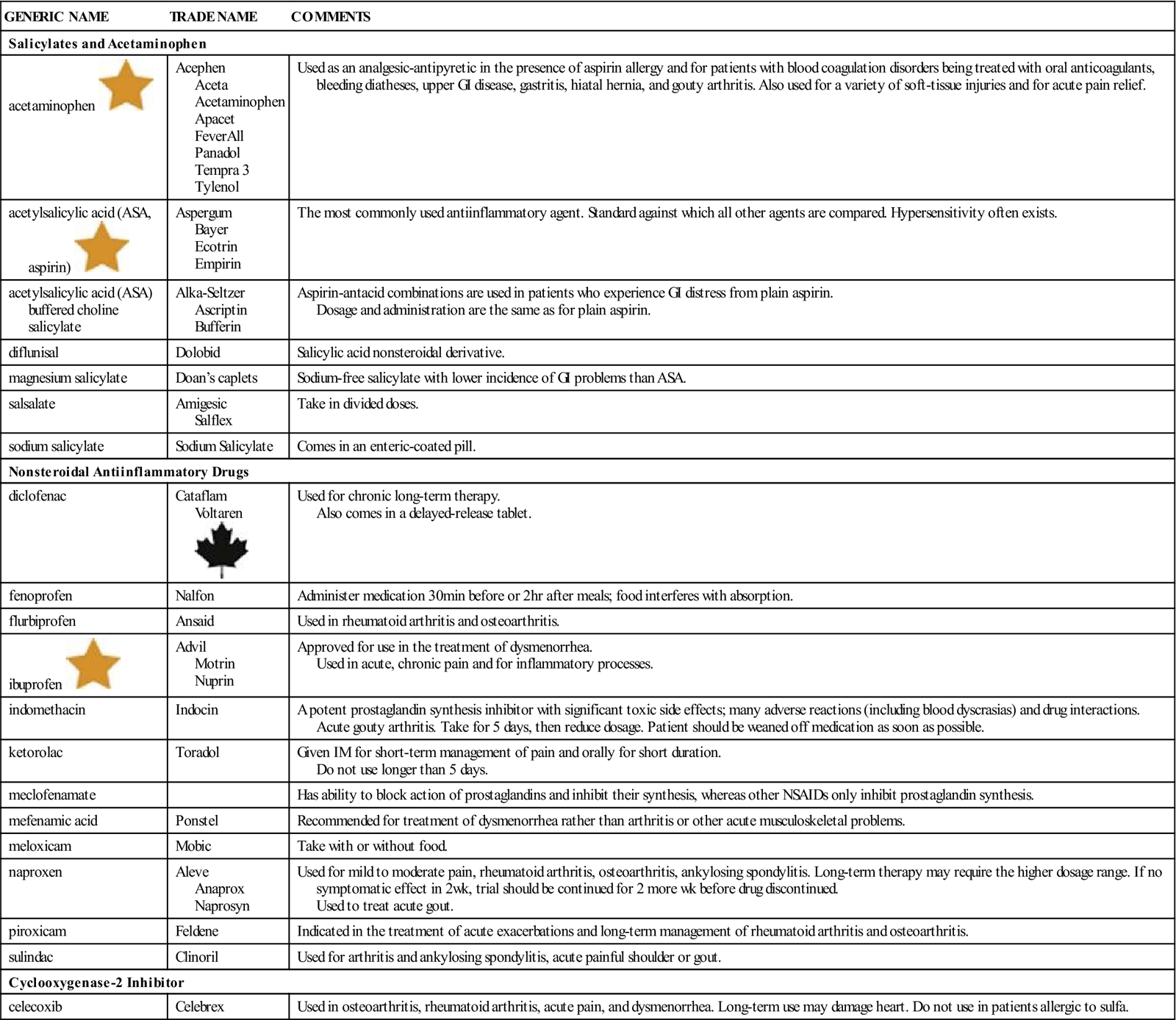
GI, Gastrointestinal; IM, intramuscular; NSAID, nonsteroidal antiinflammatory drug.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
The patient should be monitored to see that symptoms resolve (i.e., pain is gone and temperature is reduced to 101° F or lower). The dosage should be reduced or the drug stopped if tinnitus (ringing in ears) develops. Observe for fever that does not fall or other symptoms that suggest the patient is getting worse, and notify the health care provider.
For arthritis, higher dosages are usually needed to control pain and stiffness. The dosage should be slowly increased as necessary while the patient is watched not only for pain relief, but for improvement in such things as increased strength of grip, increased mobility, and improved ability to carry on normal activities of daily living. Patients taking medication over a long time should be monitored for signs of occult (hidden) bleeding with regular blood counts and stool checks. Check for signs of aspirin toxicity, especially tinnitus. Periodic checks of serum salicylate levels may be helpful if the dosage is reaching maximum levels or if there is a question of patient compliance.
n Patient and Family Teaching
Tell the patient and family the following:
Acetaminophen
Overview
Acetaminophen (Tylenol) is an OTC medication commonly used to decrease fever and mild pain. It can be used in patients who have experienced gastric irritation with aspirin or other NSAIDs. Acetaminophen is similar to aspirin in its effectiveness in treating fever and pain. It is the drug of choice for relief of minor pain in children. Acetaminophen is different from aspirin in that it does not have an antiinflammatory effect or an effect on platelet aggregation.
Acetaminophen is a metabolite of phenacetin, a product that was taken off the market because of a link with nephropathy (kidney damage). It is also linked to hepatotoxicity (liver damage) when dosage is increased. Acetaminophen may be included with other OTC drugs used to treat common illnesses.
Action and Uses
Acetaminophen works as an antipyretic by direct action on the hypothalamic heat-regulating center, lowering the temperature to a normal level. It does this by blocking the action of pyrogenic cytokines on the heat-regulating center. This helps get rid of body heat via vasodilation and sweating.
The mechanism of analgesic action is not clear. It may be due to inhibition of prostaglandin synthetase in the CNS. Acetaminophen differs from aspirin in that it does not inhibit peripheral prostaglandin synthesis. This may account for the absence of inflammatory and platelet-inhibiting effects. Acetaminophen is a very effective medication for treating chronic pain of both malignant and nonmalignant origin. Other medications are often combined with acetaminophen to enhance their effectiveness.
Acetaminophen is the initial drug of choice for treatment of osteoarthritis. It is effective in pain relief and has fewer adverse reactions than aspirin or NSAIDs.
Adverse Reactions
If used as directed, adverse reactions are rare. The symptoms of hypersensitivity are skin eruptions, urticaria, erythema, and fever. Extremely rare hematologic reactions include hemolytic anemia, leukopenia, neutropenia, and pancytopenia. Other reactions are hypoglycemia, liver toxicity, and jaundice (yellow color of skin, eyes, and mucous membranes). Overdosage is possible and may be fatal. This is particularly a problem in young children and older adults.
Drug Interactions
Use of acetaminophen with the following drugs may increase the risk of hepatotoxicity (damage to the liver): barbiturates, hydantoins (Dilantin), carbamazepine (Tegretol), rifampin, and ethanol.
Activated charcoal reduces acetaminophen absorption. Acetylcysteine (Mucomyst) is used as an antidote in acetaminophen overdose.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the patient’s health history. Ask questions to learn about other problems the patient may have that might have produced pain. Does the patient have any risk factors for drug interactions?
n Diagnosis
What other products does that patient take for symptoms of common colds or minor pains at the same time as using it for treatment of osteoarthritis? If so, do the products contain acetaminophenen that might place them at risk for overdose or developing toxicity.
n Planning
Acetaminophen is available OTC, and many patients decide when and how much medicine to take. Ask specifically about acetaminophen use when taking a medication history to include all OTC medications, herbal medicine, and prescription drugs. Generic acetaminophen is equally effective and less expensive than brand-name products.
n Implementation
Acetaminophen is the drug of choice for reduction of fever. Treatment of minor fever is not indicated unless the fever is making the patient uncomfortable. Symptomatic relief of a temperature greater than 40° C is usually required. Treatment of a temperature higher than 41° C or 105° F to 106° F is a medical emergency. Caution the patient against overdosing.
Dosing information for acetaminophen is provided in Table 21-1.
n Evaluation
Monitor fever or pain control. Watch for symptoms of gastric distress, nausea, or bleeding.
n Patient and Family Teaching
Nonsteroidal Antiinflammatory Drugs
Action
Nonsteroidal antiinflammatory drugs ((NSAIDs) have analgesic, antiinflammatory, and antipyretic effects and are used to treat rheumatic diseases, degenerative joint disease, osteoarthritis, and acute musculoskeletal problems. The exact mode of action of NSAIDs is not known, although it is believed that the analgesic and antiinflammatory effects of NSAIDs are largely the result of their ability to stop the production of prostaglandins. All NSAIDs inhibit cyclooxygenase, thus blocking the production of prostaglandins. One NSAID celecoxib (Celebrex) specifically works to inhibit COX-2, the chemical created at sites of inflammation by cytokines and inflammatory mediators. These agents also inhibit platelet clumping or aggregation, but this effect appears to be dose related.
Uses
Use of NSAIDs may be indicated for acute or chronic musculoskeletal pain.
Most NSAIDs are used in the treatment of both rheumatoid arthritis and osteoarthritis. They are used specifically in the relief of arthritic signs and symptoms, in treatment of acute inflammatory flare-ups and worsening of symptoms, and for long-term management of arthritis. NSAIDs are also used in treatment of pain from dental extraction, minor surgery, and soft-tissue athletic injuries. Ibuprofen (Advil, Motrin) has been approved for use in dysmenorrhea because of its inhibition of prostaglandin production.
Adverse Reactions
Adverse reactions to NSAIDs include asthma, fluid retention, hypertension (high blood pressure), confusion, dizziness, blurred or decreased vision, malaise (weakness), sleepiness, tinnitus, pruritus, skin irritation or rash related to sun exposure, abdominal pain, anorexia, bloating, constipation, diarrhea, dyspepsia (stomach discomfort after eating), excessive gas in the GI tract, GI bleeding (upper or lower), heartburn, nausea, vomiting, hematuria (blood in the urine; occurs with some NSAIDs or with worsened renal failure), and many forms of blood-cell changes.
Drug Interactions
Because the various NSAIDs are somewhat different structurally, their specific drug interactions vary. Therefore each agent should be checked for drug interactions that should be monitored. Most products have many significant drug interactions.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health and drug history of the patient, including sensitivity to aspirin or any of the products within this group, GI problems, renal dysfunction, history of asthma or allergic respiratory problems, anticoagulant therapy, bleeding problems, other drugs being taken that may cause drug interactions, and the possibility of pregnancy or breastfeeding.
Low doses of ibuprofen are often the first choice for pain relief in the older adult patient. The patient may complain of musculoskeletal pain or tenderness of involved areas, inflammation, stiffness, and an alteration in the normal activities of life. The onset may be gradual—the patient may show only tiredness—or it may be sudden or may occur after a change in activity or minor trauma, depending on the type of arthritic problem. The individual history of onset, duration, and location are important factors in diagnosing the type of arthritis. Evaluate the patient for signs of inflammation: tenderness, erythema, increased warmth, and swelling. Joint stiffness, decreased range of motion, or crepitus (a peculiar crackling sound) may also be present. Distribution, location, pattern (for example, on one side of the body or on both sides), and number of involved joints must be determined.
NSAIDs are not to be used in patients with past sensitivity to the drug. They are also not to be used in patients who have allergy or hypersensitivity to aspirin, because all of the specific agents are closely related to aspirin, and there is the chance for cross- sensitivity. (That is, a patient who is sensitive to aspirin may be sensitive to NSAIDs also.) Other agents in this category should not be given to patients who have had symptoms of bronchospasm, asthma, rhinitis, urticaria, nasal polyps, or angioedema (swelling of the skin and mucous membranes) after using any agents within this group.
n Diagnosis
What other medical problems or risk factors does the patient have that might make taking this drug a problem? Does the patient have concerns about weight, nutrition, safety, or mobility? Is the patient suffering from depression? Does the patient drink alcohol, smoke, or have high caffeine intake that may make his or her GI tract more sensitive to problems with this drug?
n Planning
Some agents will only be prescribed for short-term therapy because of their toxic side effects. The length of therapy should be considered by the health care provider when a particular drug is selected for treating chronic arthritis.
In problems that occur in only one joint, all infectious processes should be ruled out. This is because NSAIDs may relieve symptoms but will not affect any infectious agent. That would allow greater damage to take place if the patient continues to take NSAIDs.
n Implementation
NSAIDs are first-line drugs in the treatment and control of various forms of arthritis and in many of the single-joint inflammatory processes (for example, bursitis). If symptoms fail to improve with the use of one agent, this does not mean there will be no improvement with another. Because of the low cost, efficacy, and low toxicity of salicylates, all NSAIDs are compared with them in terms of their therapeutic benefits and side or adverse effects (see Table 18-1).
n Evaluation
Watch the patient for therapeutic effects: reduction of symptoms and ability of the patient to return to previous activities without pain. The patient should be evaluated 3 to 4 weeks after starting the medication for the first signs of improvement. If there is no reduction in symptoms or if side effects develop, another drug in the NSAID group can be tried.
The patient should be asked about adverse effects, particularly GI and CNS symptoms. Periodic laboratory analysis should also be carried out while the patient is taking this medication. Collect stool specimens to check for occult bleeding. Complete blood cell counts with differential for anemia or other blood dyscrasia problems, and ability to fight infection should be done at least twice a year.
n Patient and Family Teaching
Muscle Relaxants
Overview
Muscle relaxants are used to help reduce pain caused by muscular tension or tightness.
Action
Skeletal muscle relaxants limit the transmission or movement of impulses in the motor pathways at the level of the spinal cord and brainstem (centrally acting), or they interfere with the mechanism that shortens skeletal muscle fibers (direct myotrophic blocking), so they contract.
The main action of skeletal muscle relaxants is to reduce muscle tone and involuntary (uncontrolled) movement without loss of voluntary (controlled) motor function. Other actions include mild sedation, reduction of anxiety and tension, and changes in pain perception.
Uses
Skeletal muscle relaxants are used to relieve pain in musculoskeletal and neurologic disorders involving peripheral injury and inflammation, such as muscle strain or sprain, arthritis, bursitis, low back syndrome, cervical syndrome, cerebral palsy, and multiple sclerosis. They are often used following trauma, such as a motor vehicle or sporting accidents, when many muscles may be tender or stiff.
Adverse Reactions
Adverse reactions to skeletal muscle relaxants include flushing (red color in the face and neck), hypotension, syncope (light-headedness and fainting), tachycardia, ataxia (poor coordination), blurred vision, confusion, drowsiness, headache, insomnia (inability to sleep), irritability, abdominal pain, anorexia, bleeding, diarrhea, hiccups, nausea, many blood cell disorders, anaphylactic (shock) reactions, asthma-like reaction, dermatoses, erythema, fever, pruritus, rash, dysuria (painful urination), incontinence, urinary retention, dyspnea (uncomfortable breathing), nasal congestion, shortness of breath, wheezing, dyspepsia, euphoria (excessive happiness), metallic taste, pain or sloughing at injection site, and tremors. Cyclobenzaprine (Flexeril) has a contraindication against using the drug in patients with cardiovascular problems and hyperthyroidism. It may also be associated with Long QT syndrome, leading to lethal arrhythmias.
Drug Interactions
Skeletal muscle relaxants are known to increase the effect of CNS depressants, including sedatives, narcotic analgesics, antianxiety agents, hypnotics, and alcohol. They also increase the effects of general anesthetics, monoamine oxidase inhibitors, and tricyclic antidepressants. Cyclobenzaprine (Flexeril) and orphenadrine (Norflex) have the same effects as anticholinergic drugs. Cyclobenzaprine may interfere with the antihypertensive activity of the alpha-adrenergic blockers.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the patient’s health history, including the presence of hypersensitivity, use of other drugs that might produce drug interactions, and history of respiratory, renal, hepatic, or cardiac dysfunction. These drugs should not be given to women who are pregnant or breastfeeding or to persons with a history of drug dependency.
The patient may have a history of pain caused by acute muscular injury or inflammation (sprains or strains), low back pain syndrome, arthritis, multiple sclerosis, muscular tension with or without intermittent relief, headache, and muscle rigidity.
n Diagnosis
Does this patient have other problems that the nurse should be concerned about? Is the patient able to take care of activities of daily living, including personal hygiene and eating? Is the patient able to travel or is he or she confined at home? Is depression a problem? Has the problem made a significant difference in the patient’s activity level? All of these things may require nursing intervention. Is the patient upset or worried about being involved in a lawsuit or criminal inquiry as a result of the trauma? Is the patient concerned about legal or financial issues that make him or her tense or stressed?
n Planning
Using a skeletal muscle relaxant with other CNS drugs, including alcohol, increases the sedative actions of this drug. Therefore these drugs are not recommended for persons with a history of alcoholism or alcohol abuse.
While there are pediatric doses for some of the drugs to treat spasticity, the efficacy and safe use of these drugs have not been established in children.
The nurse should be particularly careful in recording observations and patient care and be aware of the likelihood that nursing records might be examined if a law suit is involved because of the injury.
n Implementation
Skeletal muscle relaxants are often given to hospitalized patients and available in both tablet and injectable forms. Although many muscle relaxants are given orally (PO), research suggests these drugs may not always be effective when given by this route. The oral dose must be 5 to 10 times greater than the injectable (parenteral) dose to obtain true muscle relaxation. For this reason, the parenteral form of these drugs is recommended versus the oral form. However, the parenteral form of the drug can cause local tissue irritation with injection.
In rare instances, the first dose of skeletal muscle relaxants produces an idiosyncratic (unique and unknown cause) reaction within minutes or hours. Symptoms include extreme weakness, transient quadriplegia, dizziness, ataxia (imbalance in walking), temporary loss of vision, diplopia (double vision), mydriasis, dysarthria, agitation, euphoria, confusion, and disorientation.
Table 18-2 provides a summary of skeletal muscle relaxants.
![]() Table 18-2
Table 18-2
| GENERIC NAME | TRADE NAME | COMMENTS |
| Centrally Acting | ||
| baclofen | Lioresal | Muscle relaxant, antispastic: Dosage regimen begun with 5 mg 3 times daily for 3 days. Thereafter dosage increased until desired response is obtained. Dosage adjusted according to reversal of spasticity symptoms. Maximum daily dose: 80 mg. |
| carisoprodol | Soma | Muscle relaxant: Take daily and at bedtime. Administration with meals will help reduce gastric distress. |
| chlorzoxazone | Paraflex Parafon Forte DSC Remular-S |
Initial dose for painful musculoskeletal conditions: If adequate response not obtained, dosage increased, then gradually reduced to maintenance dose once therapeutic effect achieved. Administration with meals may help avoid GI irritation. |
| cyclobenzaprine | Flexeril | Relieves acute skeletal muscle spasm of local origin without interfering with muscle function. Not to be administered for longer than 2-3 wk. |
| diazepam |
Valium | For use with geriatric or debilitated patients. This is strongly addictive and should be used for a short time. |
| metaxalone | Skelaxin | Used for muscle relaxation. Use for short time. |
| methocarbamol | Robaxin | Drug may change color of standing urine to green or black. Used for relief of muscle spasm. |
| orphenadrine citrate | Norflex Banflex |
Used for relief of muscle spasm. |
| tizanidine | Zanaflex | Given as a single oral dose. Effects are dose related. |
| Direct Acting | ||
| dantrolene | Dantrium | Spasticity: Each dosage level should be maintained 4-7 days to determine patient’s response. |
| Combination Products | ||
| carisoprodol and aspirin (also comes with codeine) | Soma Compound | Combination centrally acting skeletal muscle relaxant. Used to treat acute muscle spasms and relieve pain associated with musculoskeletal conditions. Has CNS depressant effects and physical and psychologic addictive effects; withdrawal effects occur if drug abruptly stopped. |
| orphenadrine citrate, aspirin, and caffeine | Norgesic | Combination centrally acting skeletal muscle relaxant indicated for relief of mild to moderate pain and muscle spasms of acute musculoskeletal conditions. |
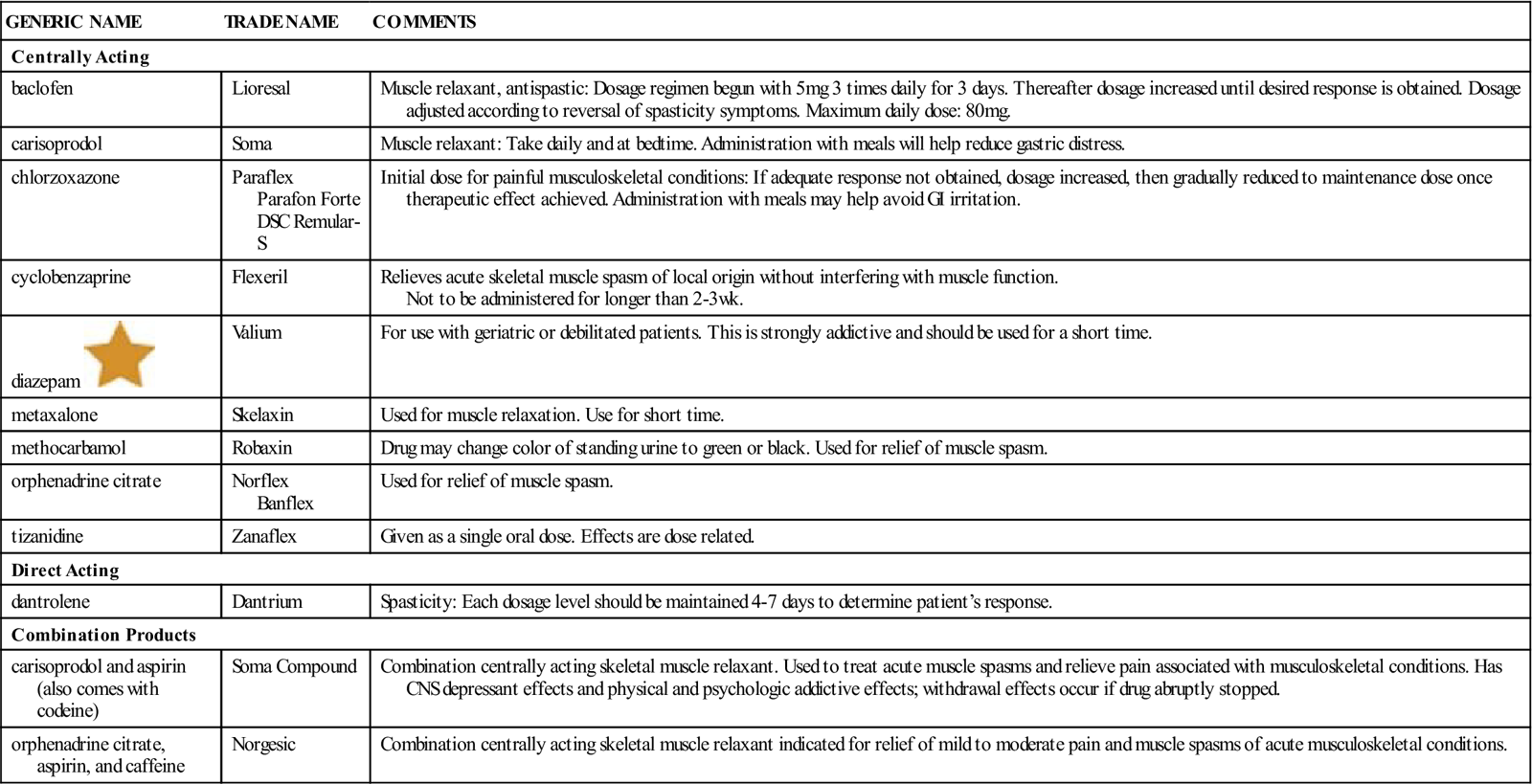
CNS, Central nervous system; GI, gastrointestinal.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
Hepatotoxicity (liver toxicity), nephrotoxicity (kidney toxicity), and abnormal blood cells have been reported with the use of skeletal muscle relaxants. Signs of hepatotoxicity include abdominal pain, high fever, nausea, and diarrhea. Signs of blood dyscrasias include fever, sore throat, mucosal irritation, malaise, and petechiae (tiny red spots on the skin). Side effects that occur most commonly include drowsiness, diplopia, dizziness, weakness, mild muscular incoordination, anorexia, nausea, vomiting, syncope, and hypotension.
The lowest dosage possible should be used, and the patient should be checked for signs and symptoms of hepatotoxicity, blood dyscrasias, dependence, and adverse drug reactions. The drug should be discontinued by the health care provider if no improvement occurs after 45 days, because the risk of hepatotoxicity increases with long-term use of these drugs.
The severity of the musculoskeletal or neurologic problem determines how long the patient should take the drug. Discontinuing the drugs suddenly may cause withdrawal symptoms after long-term use, so the dosage should be gradually reduced before being stopped.
The patient should be checked for relief of signs and symptoms, and increase in range of motion, relief from muscle spasm, pain relief, and so on.
n Patient And Family Teaching
Antiarthritis Medications
Overview
The term arthritis covers more than 100 different types of joint disease in which inflammation or destruction is present. The most common types are rheumatoid arthritis and osteoarthritis. Rheumatoid arthritis is a systemic disease that involves an autoimmune response caused by failure of the body to recognize its own tissue; this results in the body destroying its own joints. Osteoarthritis is a more localized form of joint destruction, particularly in joints that carry weight like hips and knees or have a lot of stress like hands and feet. This type of arthritis progresses gradually over time from overuse and increasing age.
Symptoms of arthritis depend upon the type of arthritis but almost all include swelling, pain, and stiffness in one or more joints. In rheumatoid arthritis, as the disease progresses, there is degeneration and destruction of the joint with permanent changes that produce deformities and immobility.
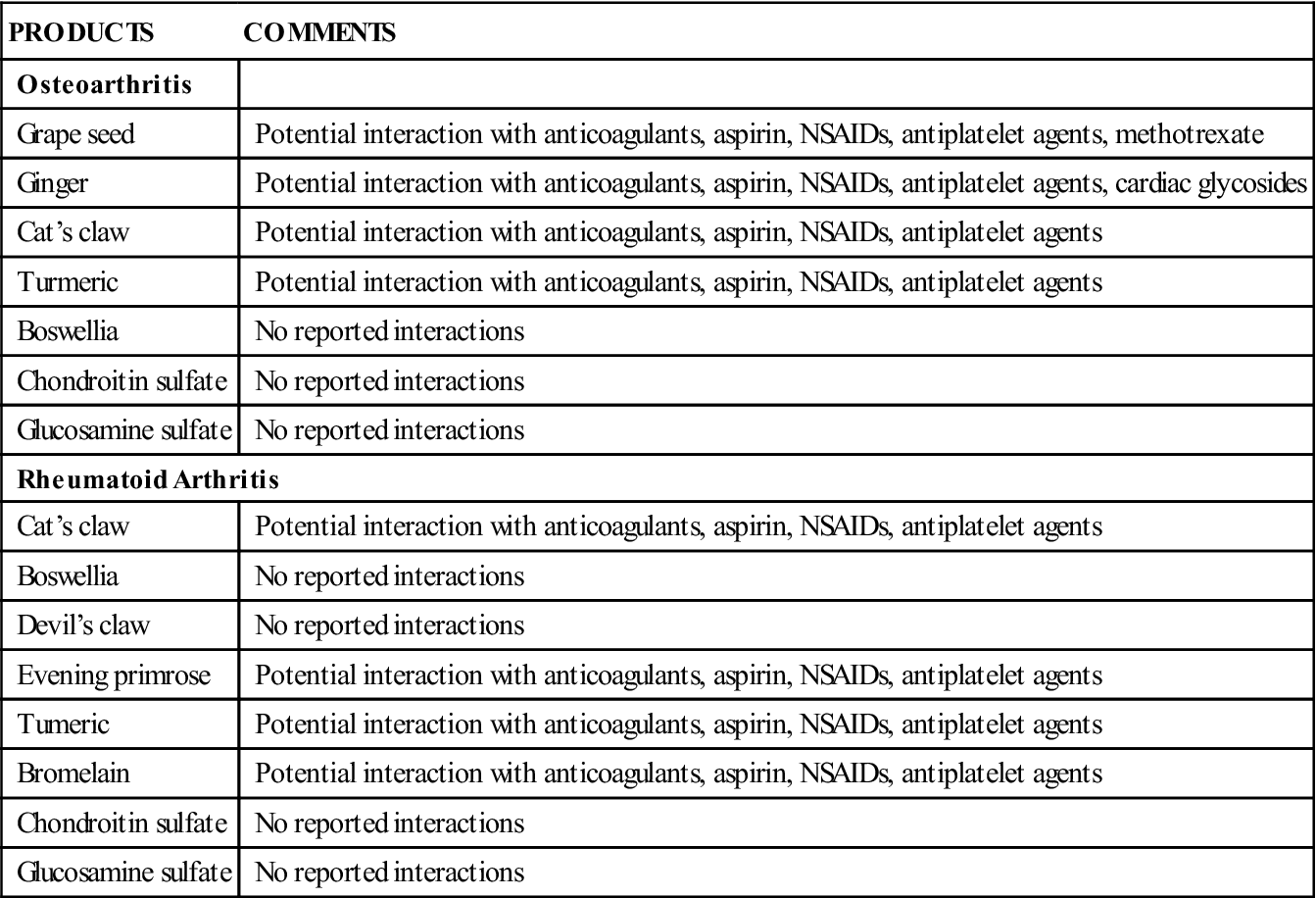
Arthritis is one of the most common disorders. Patients often do not get much relief from any of the medications they try, so they may turn to alternative medicine and herbal products to reduce arthritic symptoms and reduce pain. These herbal products have many possible interactions with other medications (see the Complementary and Alternative Therapies box).
 Disease-Modifying Antirheumatic Medications and Immune Modulators
Disease-Modifying Antirheumatic Medications and Immune Modulators
Salicylates and NSAIDs are first-line drugs for the treatment of arthritis. Steroids may also be used for antiinflammatory antirheumatic purposes and these will be discussed in Chapter 21. DMARD medications are prescribed primarily by specialists and used only in diagnosed cases of rheumatoid arthritis that have been getting worse despite other types of treatment, including high doses of NSAIDs. Nurses should know something about these drugs because none of these agents is without significant risk and toxic effects. Patients taking these drugs need constant follow-up and regular evaluation and may be admitted to the hospital or seen in offices for other problems.
The DMARDs or conventional drugs are useful in treating significant cases of rheumatoid arthritis and include hydroxychloroquine sulfate (Plaquenil), a drug typically used for malaria, a sulfonamide (sulfasalazine), and methotrexate (Rheumatrex, Folex). Most of these medications are designed to reduce pain, swelling, and inflammation; these drugs cannot stop the arthritic process. Gold compounds and penicilliamine were once prescribed but have fallen into disuse because of severe allergic reactions and will not be discussed here.
The specialty drugs most commonly used now are the immunomodulators. These include the cytokine-blockers Tumor Necrosis Factor (TNF)-α inhibitors, cytokine blockers, IL-1 receptor antagonists, and T-cell modulators. These drugs do have the ability to reduce pain and halt the destructive inflammatory processes that deform the joints.
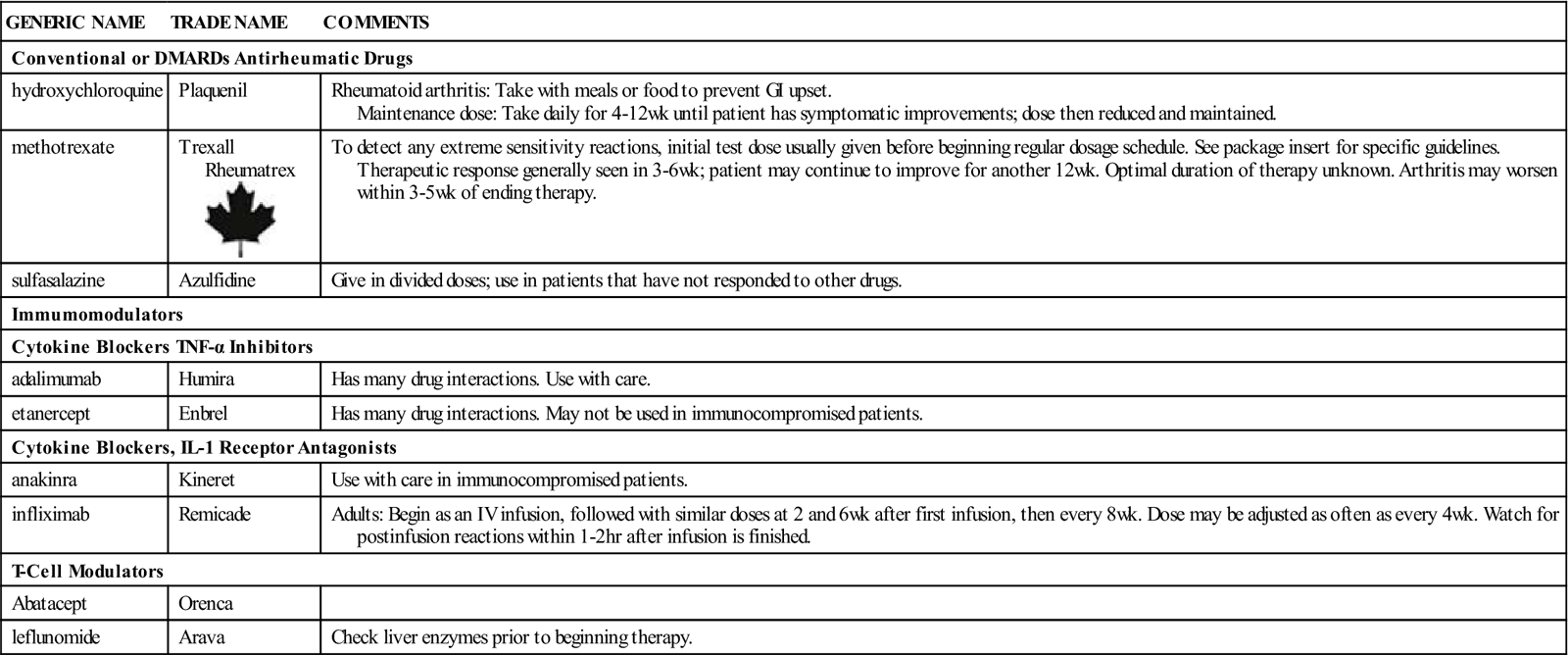
Each of these two categories are briefly described below and summarized in Table 18-3.
![]() Table 18-3
Table 18-3
| GENERIC NAME | TRADE NAME | COMMENTS |
| Conventional or DMARDs Antirheumatic Drugs | ||
| hydroxychloroquine | Plaquenil | Rheumatoid arthritis: Take with meals or food to prevent GI upset. Maintenance dose: Take daily for 4-12 wk until patient has symptomatic improvements; dose then reduced and maintained. |
| methotrexate | Trexall Rheumatrex |
To detect any extreme sensitivity reactions, initial test dose usually given before beginning regular dosage schedule. See package insert for specific guidelines. Therapeutic response generally seen in 3-6 wk; patient may continue to improve for another 12 wk. Optimal duration of therapy unknown. Arthritis may worsen within 3-5 wk of ending therapy. |
| sulfasalazine | Azulfidine | Give in divided doses; use in patients that have not responded to other drugs. |
| Immumomodulators | ||
| Cytokine Blockers TNF-α Inhibitors | ||
| adalimumab | Humira | Has many drug interactions. Use with care. |
| etanercept | Enbrel | Has many drug interactions. May not be used in immunocompromised patients. |
| Cytokine Blockers, IL-1 Receptor Antagonists | ||
| anakinra | Kineret | Use with care in immunocompromised patients. |
| infliximab | Remicade | Adults: Begin as an IV infusion, followed with similar doses at 2 and 6 wk after first infusion, then every 8 wk. Dose may be adjusted as often as every 4 wk. Watch for postinfusion reactions within 1-2 hr after infusion is finished. |
| T-Cell Modulators | ||
| Abatacept | Orenca | |
| leflunomide | Arava | Check liver enzymes prior to beginning therapy. |
 Dmards or Conventional Antirheumatic Drugs
Dmards or Conventional Antirheumatic Drugs
Hydroxychloroquine Sulfate
Action
The mechanism of action of hydroxychloroquine sulfate (Plaquenil) is not understood. This is an antimalarial drug that in some way stops the formation of antigens in the body. These antigens produce the hypersensitivity reactions leading to the physiologic changes of rheumatoid arthritis and systemic lupus erythematosus.
Uses
Hydroxychloroquine sulfate (Plaquenil) is used in diagnosed cases of rheumatoid arthritis that have been getting worse despite other methods of therapy, including high doses of NSAIDs. This agent is not without significant risk and toxic effects. Patients taking this drug need constant follow-up and regular evaluation. This drug may also be used in confirmed diagnosis of systemic or discoid lupus erythematosus.
Adverse Reactions
Hydroxychloroquine requires 4 to 12 weeks of therapy before improvement is seen. If there is no improvement after 6 months, the drug should be stopped.
If the drug is stopped because the patient is feeling relief from the symptoms, the agent can be reintroduced if the disease flares up again. Corticosteroids or NSAIDs may be used with this drug until the effects of this slow-acting drug become apparent.
Retinopathy is a serious adverse effect. The retinopathy does appear to be dose related, so patients should have an expert ophthalmologic evaluation before beginning the drug and periodic checkups every 3 to 6 months throughout therapy. The drug should be stopped if there are any visual complaints or symptoms, such as seeing flashes or streaks of light, because the retinal damage may progress even after the drug is stopped.
This product must not be used with other conventional antirheumatics because combined use will greatly increase the chance of dermatologic reactions.
Drug Interactions
Antacids and kaolin have been reported to reduce absorption of hydroxychloroquine. Use with digoxin can increase the serum digoxin levels. Hydroxychloroquine inhibits CYP2D6 in the liver and may increase anticholinergic side effects if these drugs are given at the same time. The drug may also reduce the renal clearance of methotrexate, another antiarthritic drugs. Close monitoring to detect methotrexate toxicity should be done, especially in patients with reduced renal function.
Sulfasalazine
Action and Uses
Sulfasalazine (Azulfidine) is a sulfonamide used in the treatment of rheumatoid arthritis and ulcerative colitis. Sulfasalazine is metabolized to its active components by bacteria in the colon into chemicals that have inflammatory actions.
Adverse Reactions
The most common (up to 33% of patients) adverse reactions occurring during sulfasalazine therapy I include anorexia, diarrhea, GI distress, headache, and nausea/vomiting. Agranulocytosis, aplastic anemia, and many other blood dyscrasias occur infrequently but can be fatal. These blood dyscrasias present as fever, pale skin, sore throat, fatigue, and unusual bleeding and bruising and require immediate discontinuation of the drug. Skin reactions such as rash, urticaria, and pruritus are also relatively frequent. Consult product information for other adverse reactions.
Drug Interactions
Sulfasalazine interacts with a wide variety of other drugs. It can inhibit the absorption and reduce the bioavailability of cardiac glycosides; has antifolate activity; potentiates the effects of warfarin and coumarin; and may be associated with methotrexate-induced pulmonary toxicity. It may reduce the action of Dilantin and diabetic drugs. It has many other drug interactions.
Methotrexate
Action and Uses
Methotrexate (Rheumatrex, Trexall) is an antineoplastic medication that has been used for years to treat various cancerous and psoriatic conditions. The mechanism of action in rheumatoid arthritis is unknown. It may affect immune function. It reduces joint swelling and tenderness in 3 to 6 weeks, but there is no evidence that it causes remission of the disease or limits bone erosions.
Methotrexate is used in cases of severe rheumatoid arthritis that are unresponsive to other treatment. This product has a high possibility of severe adverse reactions, including death. It is most toxic to the bone marrow, liver, kidney, and lungs. It has many contraindications to use, drug interactions, and dosage precautions. Consult the package insert for specific information.
Adverse Effects
In general, the incidence and severity of acute adverse reactions are related to the dose and frequency of administration. The most common adverse reactions are stomatitis, esophagitis, oral ulceration, nausea/vomiting, and abdominal distress. Drug-induced bone marrow suppression occurs rapidly and may cause numerous blood dyscrasias, acute and chronic hepatotoxicity, severe opportunistic infections, a transient acute neurologic syndrome with a stroke-like encephalopathy, and renal toxicity. Methotrexate is a category X drug.
Drug Interactions
Methotrexate interacts with a wide variety of drugs and only a few of the most important are listed here. Concurrent NSAID use reduces the clearance of methotrexate, resulting in elevated and prolonged serum methotrexate levels. Caution should be used in giving salicylates with methotrexate. The drug is partially bound to plasma proteins and drugs that can displace methotrexate from these proteins, such as oral sulfonylureas, phenylbutazone, hydantin anticonvulsants, or sulfonamides could cause methotrexate-induced toxicity. Oral antibiotics may decrease intestinal absorption of methotrexate or interfere with liver circulation.
 Immunomodulators
Immunomodulators
Three different subclasses of immunomodulators are in current use. They are the cytokine blockers TNF-α inhibitors, the cytokine blocker IL-1 antagonists, and the T-cell modulators.
Cytokine Blockers TNF-α INHIBITORS
Action and Uses
These drugs are monoclonal antibodies specific for tumor necrosis factor-alpha and are approved as sole therapy in the treatment of rheumatoid arthritis (RA), and are administered subcutaneously. In addition to reducing the signs and symptoms of RA and ankylosing spondylitis, and several other arthritic-type diseases. The drugs reduce disease progression, and significantly improve pain and inflammation.
The cytokine blockers TNF-α inhibitors such as adalimumab (Humira), and etanercept (Enbrel) act to neutralize the biological activity of tumor necrosis factor-alpha by binding to it and blocking its interactions with TNF receptors.
Adverse Effects
Adalimumab may cause myositis. The most common adverse events are rash, headache, and pruritus. Cutaneous vasculitis and erythema multiforme have also been reported. Rare cases of blood dyscrasias are also reported.
One of the most common adverse reactions reported with etanercept is an injection site reaction lasting 3-5 days. The drug may worsen psoriasis. Infections including active tuberculosis, invasive fungal infections, and other opportunistic bacterial and viral infections have been reported. Pancytopenia and other blood dyscrasias are common. Diarrhea and inflammatory bowel disease have been noted. It may also increase the risk of secondary malignancy.
Drug Interaction
These drugs should not be used with other TNF-alpha blockers. The immune response to vaccines or toxoids may be decreased. Safety for use immunocompromised patients is unknown. Do not give abatacept with adalimumab.
Concurrent use of etanercept and cyclophosphamide or sulfasalazine is not recommended. There is only limited data examining the safety and efficacy of vaccine or toxoids given with this drug. Serious infections may develop if given with anakinra.
Cytokine Blockers, IL-1 Receptor Antagonists
Action and Uses
These cytokine blockers IL-1 receptor antagonist drugs, such as infliximab (Remicade) and anakinra (KIineret), are used in combination with methotrexate to reduce the signs and symptoms of rheumatoid arthritis and limit the worsening of damage to joints. This leads to improved physical function in patients with moderate to severe active rheumatoid arthritis who have had an inadequate response to methotrexate alone. It is also used in Crohn disease (inflammatory bowel disease) and some orthopedic inflammatory or destructive processes.
Adverse Reactions
This drug may activate tuberculosis, invasive fungal infections, and other opportunistic infections. (A test for tuberculosis should be given and any latent tuberculosis treated prior to beginning the patient on this therapy.) There is a high mortality rate in patients who have preexisting congestive heart failure. Watch for hypersensitivity and infusion-related reactions (for example, dyspnea, flushing, headache, and rash that may occur within 1 to 2 hours of the infusion).
Drug Interactions
Infliximab shuld not be given with abatacept, anakinra, rilonacept, and tocilizumab as the incidence of serious infections increases. Anakinra should not be given with rilanacept or any TNF modifiers because of the increased risk of serious infections.
For both drugs, the immune response to vaccines or toxoids may be decreased. Safety for use immunocompromised patients is unknown.
T-Cell Modulators
Action and Uses
T-cell modulators such as abatacept (Orencia) and leflunomide (Arava) are pyrimidine synthesis inhibitors that have an antiinflammatory effect. They are used in treatment of active rheumatoid arthritis in adults to reduce signs and symptoms and to slow structural damage in joints.
Adverse Reactions
The Federal Drug Administration requires a warning label that pregnancy must be ruled out and avoided in all women who are of childbearing age while they are taking this drug. This is a category X drug that is contraindicated during pregnancy.
Leflunomide may produce hepatotoxicity, and there is some evidence of increased risk of cancer of the lymph system. In patients taking abatacept, common reactions were headache, dizziness, hypertension, and dyspepsia and these may start within 1 hour of taking the medicine. Hypersensitive reactions may also develop. As T cells mediate cellular responses, these drugs may affect host defenses against infections and malignancies.
Drug Interactions
Use of abatacept and anakinra together is not recommended. Do not give with TNF modifiers. Abatacept may increase the onset of respiratory infections and should not obe used with drugs that decrease mucus production and clearance such as general anesthetics or atropine and scopolamine. Live viruses should not be given concurrently with abatacept or within 3 months of its discontinuation.
Leflunomide should not be given with other hepatotoxic drugs as it increases the risk of hepatotoxicity. It inhibits the cytochrome P45 2C9 system. Increased International Normalized Ratio when this drug and warfarin are coadministered is possible. It also appears to interact with rifampin.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
After reading specific information from the package insert about the medication, learn as much as possible about the patient’s health history, including the treatment history of the patient’s arthritis; presence of drug sensitivities; underlying diseases such as renal, liver, cardiovascular, or hematopoietic diseases that contraindicate any of these products; the possibility of pregnancy; and other drugs taken at the same time that might cause drug interactions.
n Diagnosis
What is the patient’s general level of mobility? Do pain and joint deformity interfere with the ability to perform activities of daily living or required tasks on the job? Is the patient able to comply with the treatment regimen? Does the patient experience side effects from antiarthritis medication? What effect has chronic rheumatoid disease had on emotions and the ability to cope? Does the patient have other kidney disease?
n Planning
These drugs are not without significant adverse reactions. The benefits of the medication must be weighed against the risks and serious adverse reactions.
n Implementation
These drugs will be given by rheumatologists. Nurses do not often administer these drugs. A summary of dosage information concerning antiarthritis medications is provided in Table 18-3.
n Evaluation
The nurse should observe for the therapeutic effect and monitor closely for the numerous and serious adverse effects that may develop.
n Patient and Family Teaching
Antigout Medications
Overview
Uric acid comes from the metabolism of protein and is present in the blood within a very specific range. Several pathologic processes, metabolic changes, or drug interactions may be responsible for increasing the uric acid level of the blood above an acceptable amount. High uric acid levels cause the excess uric acid to form crystals, usually in the kidneys and in joint spaces. These crystals have very long, sharp, and jagged edges. These crystals tear and bruise the tissues with which they come in contact. The result is swelling or increased tissue edema, heat, inflammation, and severe pain—the syndrome called gout. Gout is a form of arthritis caused when the body makes too much (overproduction) or does not get rid of (underexcretion) uric acid, and may manifest in any joint.
The drugs used to treat gout vary in their method of action. Those used to treat acute attacks act to relieve pain and inflammation. Other drugs called uricosurics alter the body’s response to, production of, or distribution of uric acid to prevent gout attacks.
Action
The management of gout involves three different steps: reducing the inflammatory response (colchicine, glucocorticoids and ACTH, and NSAIDS), decreasing uric acid production allopuruinol (Zyloprim), and increasing uric acid clearance (probenecid and sulfinpyrazone). The glucocorticoids and ACTH are reserved for acute attacks when the patient is resistant to therapy or if there is a contraindication to use of colchicine or NSAIDS. Chronic gout is usually treated with uricosuric agents, allopurinol, or daily colchicine given in low doses.
Uricosuric agents increase the excretion of urate salts in the urine by blocking tubular reabsorption of these salts in the kidney. They also decrease the amount of circulating urate and the deposition of urate and promote reabsorption of urate deposits. Sulfinpyrazone also has platelet inhibitory and antithrombotic effects. Uricosuric agents do not have significant antiinflammatory or analgesic properties and therefore are of little help during an acute episode of gout.
Colchicine is a special drug used to treat acute gouty attacks. It is not an antiinflammatory, analgesic, or uricosuric agent. The mechanism of action of colchicine in relieving gouty attacks is not completely known. It is believed to be involved in the inhibition of leukocyte migration and phagocytosis that causes the inflammatory response in gout. It also decreases uric acid deposits in the tissues. In addition to use in the acute stage, it may also be used with allopurinol or other uricosuric agents to prevent an acute attack.
Probenecid inhibits tubular reabsorption of urate, increasing uric acid excretion.
Allopurinol inhibits the production of uric acid by decreasing the production of xanthine oxidase, an enzyme that metabolizes purine hypoxanthine to xanthine and xanthine to uric acid. This drug has no analgesic or antiinflammatory properties and therefore is not beneficial in the treatment of acute gout. Instead, it is used in prophylactic (preventive) therapy for repeated or chronic gout. It is also used in patients with renal failure severe enough to increase their uric acid levels to a point at which they may develop gouty attacks.
Corticosteroids and ACTH decrease inflammation in gout. They do this by inhibiting the release of leukocyte adhesion to the capillary wall, inhibiting histamine release, and interfering with the formation of scar tissue, as well as other processes.
Uses
Usually the patient comes in with an acute attack and the diagnosis of gout is made. The joint with acute gout is very painful, red, and swollen. Even a sheet on a toe might not be tolerated. Oral colchicine and/or NSAIDS are first-line agents for systemic treatment of acute attacks. Colchicine is used to treat gouty attacks when the diagnosis of gout is either confirmed or suspected by the patient’s history and physical examination and when examination of joint fluid is not possible. Colchicine relieves the pain of acute attacks but it does not decrease the levels of uric acid. Intraarticular aspiration and injection of a long-acting steroid is safe and effective for acute gout attacks.
For those patients with recurrent acute attacks, arthropathy, tophi, or x-ray changes, urate-lowering therapy, usually with allopurinol, is used long term to maintain the serum uric acid level below 6.8 mg/dL and to dissolve urate crystals. Uricosuric agents such as probenecid are an alternative to allopurinol. Colchicine may also used along with allopurinol or uricosuric agents to prevent a gouty attack until the serum uric acid level is reduced to normal and stabilized. It has no effect on uric acid levels itself. It may be used prophylactically along with NSAIDs (such as indomethacin, naproxen, and sulindac) to prevent recurrent attacks, but only in combination with a uricosuric agent.
Uricosuric agents are primarily used to reduce uric acid levels in patients who do not excrete enough uric acid. The diagnosis of gout is confirmed by serum uric acid levels greater than 7 mg/100 mL and a 24-hour urine test for uric acid of less than 800 mg/day. The patient has usually had more than one acute episode before being started on these agents.
Sulfinpyrazone (Anturane) is used only in patients who do not respond to all other drugs. It is the preferred drug for patients with gout secondary to hypertensive diuretic therapy and may have other risk factors for coronary artery disease.
Allopurinol (Zyloprim) generally is used when objective findings show any of the following conditions:
• Uric acid nephropathy with impaired renal function (creatinine clearance less than 80 mL/min)
• Tophi, or small masses of crystals, on bony prominences (often the elbow or ankle)
• When kidney stones are seen by flat plate x-ray study of the abdomen
• Primary or secondary hyperuricemia associated with blood dyscrasias and their treatment
Probenecid is also often used with penicillin preparations to treat venereal diseases because of its ability to increase the plasma level of penicillin. Levels may increase two to four times normal, regardless of the route of penicillin administration.
Corticosteroids (such as methylprednisolone) are often injected into the joints if 1 or 2 accessible joints are involved. Where systemic steroids are required, doses of oral prednisone are given for several days and then gradually the dose tapered over 10-14 days.
Adverse Reactions
Uricosuric agents may produce drug fever, dizziness, pruritus, rashes, anorexia, constipation, diarrhea, nausea, vomiting, and exacerbation of acute attacks of gout. Rarely, anaphylaxis, nephrotic syndrome, hepatic necrosis, and aplastic anemia are seen.
Colchicine may cause abdominal pain, hemorrhagic gastroenteritis, severe diarrhea, nausea, and vomiting. Chronic use may cause bone marrow depression, agranylocytosis, aplastic anemia, alopecia (hair loss), peripheral neuritis, purpura (bruising), and myopathy. There is usually a delay between overdosage and onset of symptoms. Deaths have been reported with as little as 7 mg. Risk of colchicine-related deaths increases when it is given with cyclosporine, erythromycin, calcium channel antagonists (verapamil and diltiazem), tellithromycin, ketoconazole, HIV protease inhibitors, or nefazodone.
The most common adverse effect with use of a allopurinol (Zyloprim) is skin rash that may develop up to 2 years after the beginning of treatment. It may also produce drowsiness, alopecia, purpura, diarrhea, abdominal pain, nausea, vomiting, and blood dyscrasias. It may produce idiosyncratic potential fatal toxicity syndrome shown by fever, chills, arthralgias (joint pain), skin rash, pruritus, nausea, vomiting, interstitial nephritis, occasional development of cataracts, and vasculitis that may lead to hepatotoxicity and death.
Febuxostat (Uloric) has a higher rate of risk of cardiovascular thromboembolic events compared to allopurinol.
All of the NSAIDs produce similar adverse effects, the most common being nausea, anorexia, abdominal pain, and ulceration. (See Chapter 17 for a discussion of these drugs.)
All glucocorticoids, by stimulating negative feedback, can suppress the HPA axis. These drugs are also discussed in greater detail in Chapter 21.
Drug Interactions
Salicylates antagonize (interfere with) the uricosuric action of these drugs. Uricosurics increase the effects of the following drugs by decreasing renal tubular excretion: sulfonamides, sulfonylureas, naproxen, indomethacin, rifampin, dapsone, pantothenic acid, aminosalicylic acid, and methotrexate. Additionally, sulfinpyrazone affects anticoagulants by increasing their platelet aggregation effects.
The effects of colchicine are blocked by acidifying agents and increased by alkalinizing agents. Patients taking this drug may have an increased sensitivity to CNS depressants. Colchicine also decreases gut absorption of vitamin B12. The effects of sympathomimetics are increased by colchicine.
Hypersensitivity may occur in patients with renal compromise who are taking thiazides and allopurinol at the same time. Use at the same time as ampicillin may increase the chance for skin rashes. Allopurinol increases the half-life of anticoagulants and many other drugs.
Febuxostat (Uloric) is contraindicated in patients treated with azathioprine, mercaptopurine, or theophylline.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the patient’s health history, including the presence of hypersensitivity, other drugs being taken that could cause drug interactions, history of other disease, or the possibility of pregnancy. These conditions are precautions or contraindications to the use of antigout medications. The frequency and severity of the attacks should be recorded to help determine whether therapy with colchicine is indicated.
The patient may complain of an initial or recurrent attack of inflammation, erythema, swelling, extreme tenderness, and pain, usually in a single joint. At least 50% of initial attacks occur in the great toe at the metatarsal-phalangeal joint (podagra). This disease usually develops in the lower extremities. Joints affected may be in the instep, ankles, heels, or knees, although some patients are also bothered in wrists, fingers, and elbows. In patients with a severe or worsening form of the disease, additional joints may be involved. These symptoms are sudden in onset, and the patient may complain of being unable to tolerate clothing, shoes, or even bed coverings touching the site of inflammation. In some cases, there is a history of minor trauma to the involved joint, obesity, alcohol intake, use of a new drug such as hydrochlorothiazide, or low-dose aspirin consumption.
n Diagnosis
In addition to the medical diagnosis, what other problems exist for the patient? Are there general concerns about weight, diet, stress, or conditions that would limit the use of medication? How can the nurse help the patient prevent future attacks? What does the patient need to learn about gout and its treatment?
n Planning
The nurse can assist in collecting a 24-hour urine test for uric acid level and creatinine clearance and baseline laboratory tests as ordered by the health care provider.
Uricosuric agents are to be started only after the acute attack has resolved. Prophylactic therapy is recommended in patients having more than one acute attack per year. If affected less often, the patient should try to control attacks by having colchicine on hand and beginning treatment as soon as symptoms develop.
Initiation of therapy with uricosuric agents may cause an acute attack of gout, so colchicine is often given to prevent such an attack.
The use of salicylates in small or large doses is contraindicated in patients taking probenecid, because salicylates antagonize the uricosuric action of this drug. Patients needing mild pain relief for other conditions should be told to use only acetaminophen products.
Allopurinol (Zyloprim) may also cause a gouty attack during the initial treatment phase. This is easily prevented by prophylactic use of colchicine 0.5 mg twice daily PO for 2 weeks to 1 month. Good fluid intake and neutral or alkaline pH of the urine are important to prevent the possibility of xanthine stone or calculi forming. Patients with poor renal function require smaller doses, and renal function should be carefully watched.
When patients switch from uricosuric agents to allopurinol, a gradual increase of allopurinol with a gradual decrease of the other agent should be made over a period of several weeks. The patient should be watched for complications, and blood work will likely be ordered to monitor serum uric acid levels.
n Implementation
The patient’s urine should be alkalinized to prevent hematuria or formation of urate stones, especially during the initial stages of therapy. Injectable doses of colchicine are not to be given intramuscularly or subcutaneously, but must be given only intravenously.
With an acute attack, colchicine should be given immediately, and then a dose should be given every hour until either symptoms go away or the patient develops signs of toxicity.
Table 18-4 provides a summary of dosage information concerning some common antigout medications.
![]() Table 18-4
Table 18-4
| GENERIC NAME | TRADE NAME | COMMENTS |
| Antigout Analgesic Preparations for Acute Gouty Attacks—First Line Drugs to Reduce Inflammation | ||
| colchicine | Colchicine | Acute attack of gout: Therapy should be started at first warning of an acute attack. Delay of even a few hours greatly reduces therapeutic effectiveness. PO: Follow directions closely. Give medication every hour or two until pain is relieved or nausea, vomiting, or diarrhea develops. Pain usually relieved in 12 hr and gone in 24-48 hr. IV: Give until pain is relieved. Prophylactic therapy: Give daily in single or divided doses, usually in combination with a uricosuric agent. |
| NSAIDS | ||
| naproxyn | Aleve | Used in reducing inflammation and swelling in acute gouty attacks. |
| indomethacin | Indocin | Used in reducing inflammation and swelling in acute gouty attacks. |
| sulindac | Clinoril | Used in reducing inflammation and swelling in acute gouty attacks. |
| Corticosteroids | ||
| Methylprednisolone | For injection into painful joints. | |
| prednisone |
For systemic steroid use | |
| Uricosuric Agents—Decrease Uric Acid Production | ||
| allopurinol | Zyloprim | Effective in reducing uric acid levels in blood |
| febuxostat | Ulonic | New product used primarily when patient unable to tolerate allopurinol. |
| Uricosuric Agents—Increase Uric Acid Clearance | ||
| probenecid | Increases urate excretion. Often used with penicillin to treat venereal disease. Cross-sensitivity to phenylbutazone and other pyrazoles. | |
| sulfinpyrazone | Anturane | Drug reserved for patients refractory to all other modalities of therapy. Initial dose: Should be taken with meals. Maintenance dose: Therapy should be continued even during acute episodes. Patient may be switched from other uricosuric agents to this drug at full maintenance dose. |
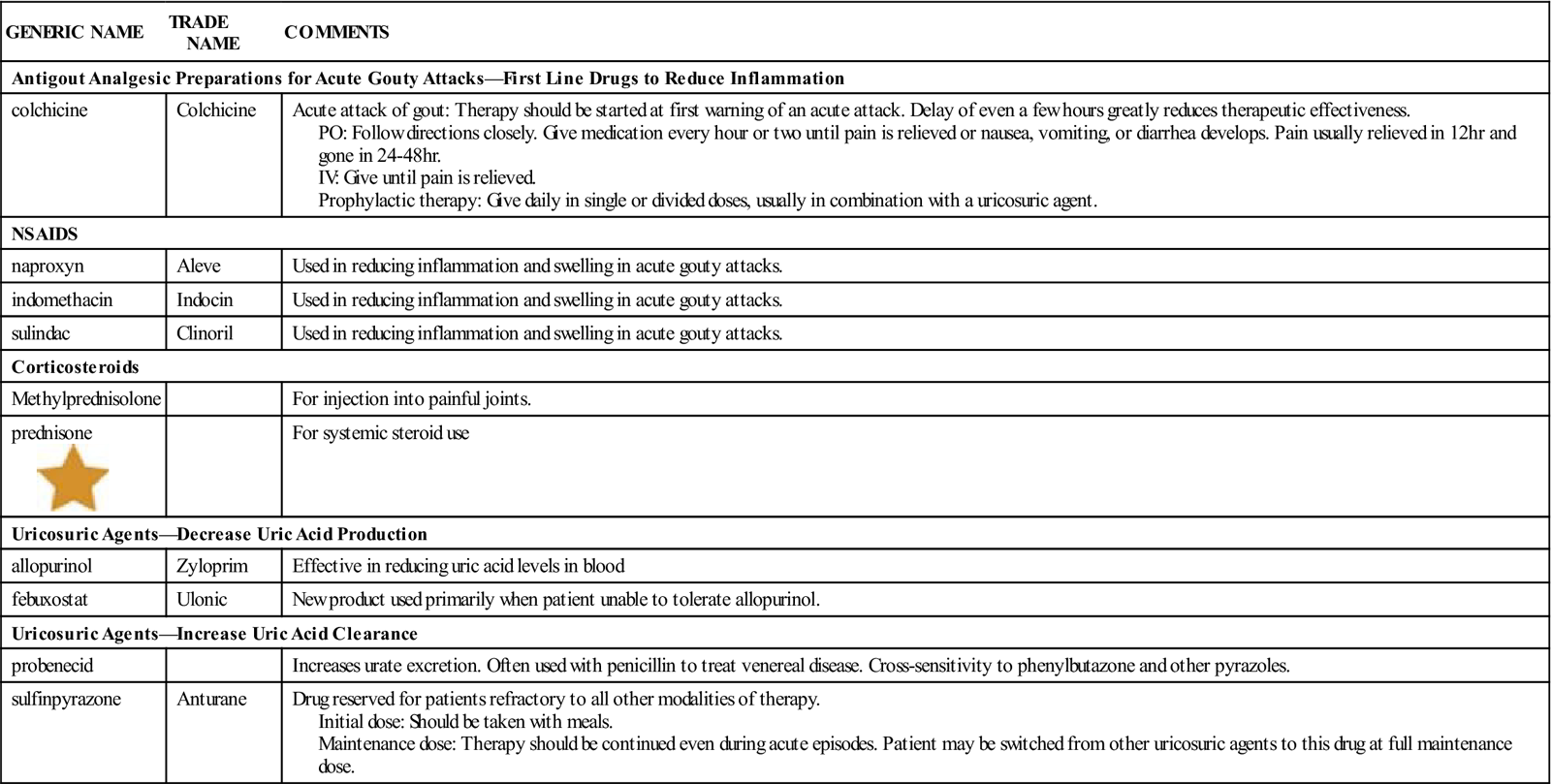
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use. IV, intravenous; PO, by mouth.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use. IV, intravenous; PO, by mouth.
n Evaluation
Colchicine must be started as soon as the patient has gout pain. Observe for therapeutic effects and adverse reactions. The patient being treated for acute attacks with a loading dose can usually reach a maximum dose level before the onset of GI side effects. The patient should be checked frequently for weakness, anorexia, nausea, vomiting, or diarrhea, because these are the first indications of toxicity. If these symptoms appear, the dosage should be reduced. If the patient has taken colchicine for a long time, vitamin B12 deficiency may develop.
If the nurse is seeing the patient over several months, watch for the therapeutic effects (decrease in frequency and severity of gouty attacks) of these drugs and watch for symptoms of the arthritis process (joint deformity, destruction, or formation of tophi).
The effect of allopurinol is seen 5 to 10 days after therapy is started. The dosage should be adjusted to maintain a serum uric acid level of less than 7 mg/100 mL. Uric acid levels as low as 2 to 3 mg/100 mL are not harmful. Adverse reactions such as rash, appearance of tophi, and change in joint deformities should be monitored.
If a maculopapular rash develops in the patient taking allopurinol at any time during therapy, the drug should be stopped immediately and it should not be restarted.
n Patient and Family Teaching
Tell the patient and family the following:
• Things the patient may do to help prevent or control gouty attacks include:
• Control weight with daily exercise
• Limit the amount of red meat eaten
• Replace eating fish with omega-3 fatty acids supplements
• Stop eating foods and drinks containing high fructose
• Eat 1-2 servings of dairy or calcium supplements daily