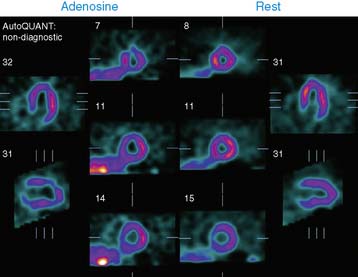
Case 18
What should the nuclear cardiology laboratory do about this patient?
1. Coiera E. Communication systems in healthcare. Clin Biochem Rev. 2006;27:89-98.
2. Lippi G., Fostini R., Guidi G.C. Quality improvement in laboratory medicine: Extra-analytical issues. Clin Lab Med. 2008;28:285-294.
3. Magni V., Chieffo A., Colombo A. Evaluation of intermediate coronary stenosis with intravascular ultrasound and fractional flow reserve: Its use and abuse. Catheter Cardiovasc Interv. 2008;73:441-448.