CASE 175
History: A 57-year-old man presents with dyspepsia.
1. What should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
2. If on a barium examination the stomach does not change shape, what might you call this condition?
3. What is the most common metastatic malignancy that could cause a linitis plastica appearance?
4. What is the most common benign etiology for the linitis plastica appearance?
D. Helicobacter pylori infection
ANSWERS
CASE 175
Uremic Gastritis
1. A and B
2. B
3. B
4. A
References
Ba-Ssalamah A, Prokop M, Uffmann M, et al: Dedicated multidetector CT of the stomach: spectrum of diseases. Radiographics. 2003;23(3):625-644.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 70.
Comment
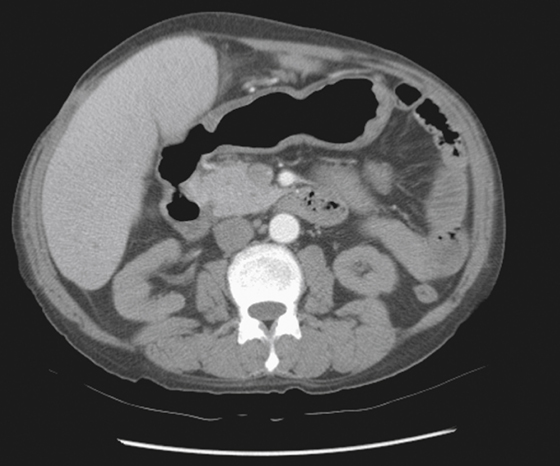
The usual cause of an atrophic, rigid nonpliant stomach is generally primary or metastatic malignancy. It cannot be totally excluded here, but the lack of a mass makes it much less likely (see figure). Other conditions that diffusely involve the stomach and result in a ridged “linitis-like” picture must be considered. In this case, the patient was a sickle cell patient with chronic renal failure. In such patients, chronic severe gastritis is common. Many also have chronic duodenitis, such as this patient. Uremic gastritis is mostly seen in patients on long-term dialysis. There is also thought to be a higher incidence of peptic ulcer disease in such patients.
A correlation between elevated serum creatinine levels and serum gastrin levels seems to exist, although it is unclear that this is an instigating factor involved with uremic gastritis. Increased urea in the blood may affect the gastric mucosa directly. Endoscopically, uremic gastritis has been described as atrophy and hemorrhagic erosive gastritis. Involvement of H. pylori as a causative effect in uremic gastritis has also been considered and found to occur with about the same frequency as in other patients with peptic ulcer disease. Whatever the cause, there seems to be little doubt that patients on long-term dialysis have a higher level of chronic gastritis, duodenitis, and peptic ulceration and erosions and are more predisposed to gastrointestinal bleeding than the normal population.