CASE 173
History: A 63-year-old woman presents with sudden onset of dysphagia; she cannot tolerate pills, fluids, or her own saliva.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the most common predisposing factor for esophageal foreign body obstruction?
3. What therapeutic option should a radiologist perform first on discovery of an impacted food bolus in the distal esophagus?
D. Proteolytic enzyme via nasogastric tube
4. What is the treatment?
A. Nothing; peristalsis eventually breaks up the bolus
ANSWERS
CASE 173
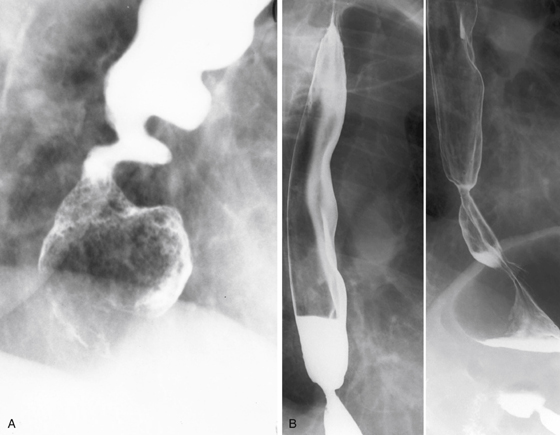
Food Impaction in Esophagus Secondary to Stricture
1. A and B
2. C
3. C
4. C
References
Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41(1):33-38.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 37.
Comment
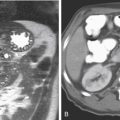
Esophageal food impaction is common. In virtually in every case, there is some underlying disease; this is usually in the form of a mild area of narrowing or stricture that is located in the distal esophagus, associated with chronic reflux disease (see figures). It can often turn out to be the symptomatic form of the esophageal “B” ring, referred to as Schatzki ring. This condition is sometimes referred to as the “steakhouse syndrome,” suggesting that the patient has swallowed a large, inadequately chewed solid bolus of food. The reasons for this can vary depending on the patient. Mild intoxication has often been implicated, such as in the “café coronary,” in which the bolus becomes stuck in the cervical esophagus or the esophagopharyngeal junction, occluding or compressing the airway. In such cases, the more dramatic Heimlich maneuver is called for to prevent asphyxiation.
The capacity for the human gastroesophageal junction to stretch to accommodate a large bolus of food is high. The esophagus may be anatomically divided into the tubular and vestibular esophagus. The vestibule is a short segment of natural widening of the esophagus just above the gastroesophageal junction and should not be confused with a small hiatal hernia. No gastric folds are present in this natural widening, and it is more prominent in some patients than in others. Because of this vestibule, even a large bolus can usually pass the gastroesophageal junction safely.
When a solid bolus becomes impacted near the gastroesophageal junction, the radiologist should appreciate the extremely high probability that some underlying narrowing is present. If the narrowing is mild, it can easily be missed at endoscopy. In follow-up studies, a barium tablet (12.5 mm) should be used; the tablet is often hung up in the narrowed area and subsequently washed down with warm water. The radiologist should explain to the patient that the barium tablet is not a medication.