Procedure 17 Surgical Treatment of Neuromas in the Hand
Indications
 Neuroma with the following characteristics:
Neuroma with the following characteristics:
Examination/Imaging
Clinical Examination
 Patients may present with pain associated with scar and altered sensation (hypoesthesia, hyperalgesia, or anesthesia). The pain may be spontaneous or result from pressure over the neuroma, movement of adjacent joints, or light touch in the vicinity of the neuroma.
Patients may present with pain associated with scar and altered sensation (hypoesthesia, hyperalgesia, or anesthesia). The pain may be spontaneous or result from pressure over the neuroma, movement of adjacent joints, or light touch in the vicinity of the neuroma.
 A painful neuroma by itself is not an indication for surgery. Information regarding the cause of injury, contributing factors (e.g., bowling, method of holding equipment), workers’ compensation and litigation issues, and functional status of the patient must be obtained. Patients must also be evaluated for the presence of complex regional pain syndrome.
A painful neuroma by itself is not an indication for surgery. Information regarding the cause of injury, contributing factors (e.g., bowling, method of holding equipment), workers’ compensation and litigation issues, and functional status of the patient must be obtained. Patients must also be evaluated for the presence of complex regional pain syndrome.
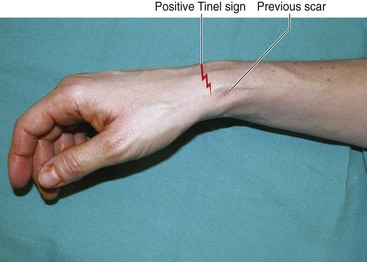
 The location of the neuroma in relation to any overlying scar and the presence of a Tinel sign must be noted (Fig. 17-1).
The location of the neuroma in relation to any overlying scar and the presence of a Tinel sign must be noted (Fig. 17-1).
Surgical Anatomy
 A neuroma of the hand can be an end neuroma or an in-continuity neuroma. End neuromas are frequently associated with digital amputation and involve the proper digital nerves. In-continuity neuromas most often result from poor surgical repair and involve the median and ulnar nerves at the wrist. Both end neuromas and in-continuity neuromas can also result from unrecognized iatrogenic injury (e.g., superficial radial nerve, palmar cutaneous branch of median nerve) or delayed presentation of a partially or completely divided nerve.
A neuroma of the hand can be an end neuroma or an in-continuity neuroma. End neuromas are frequently associated with digital amputation and involve the proper digital nerves. In-continuity neuromas most often result from poor surgical repair and involve the median and ulnar nerves at the wrist. Both end neuromas and in-continuity neuromas can also result from unrecognized iatrogenic injury (e.g., superficial radial nerve, palmar cutaneous branch of median nerve) or delayed presentation of a partially or completely divided nerve.
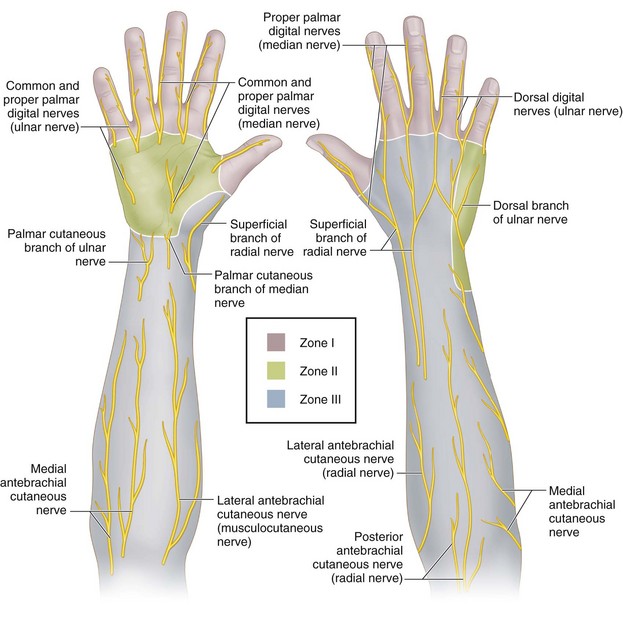
 The hand and wrist have been classified into three zones based on the location of the neuroma (Fig. 17-2). Zone I represents the digits and includes neuromas arising from the digital nerves, their dorsal branches, and the terminal branches of the nerves innervating the dorsum of the hand. Zone II represents the body of the hand and includes the common digital nerves, the palmar cutaneous branches of the median nerve, and the palmar and dorsal cutaneous branches of the ulnar nerve. Zone III represents the radial border of the wrist and forearm and includes the superficial radial nerve, the lateral antebrachial cutaneous nerve, the medial antebrachial cutaneous nerve, and the posterior cutaneous nerve of the forearm.
The hand and wrist have been classified into three zones based on the location of the neuroma (Fig. 17-2). Zone I represents the digits and includes neuromas arising from the digital nerves, their dorsal branches, and the terminal branches of the nerves innervating the dorsum of the hand. Zone II represents the body of the hand and includes the common digital nerves, the palmar cutaneous branches of the median nerve, and the palmar and dorsal cutaneous branches of the ulnar nerve. Zone III represents the radial border of the wrist and forearm and includes the superficial radial nerve, the lateral antebrachial cutaneous nerve, the medial antebrachial cutaneous nerve, and the posterior cutaneous nerve of the forearm.
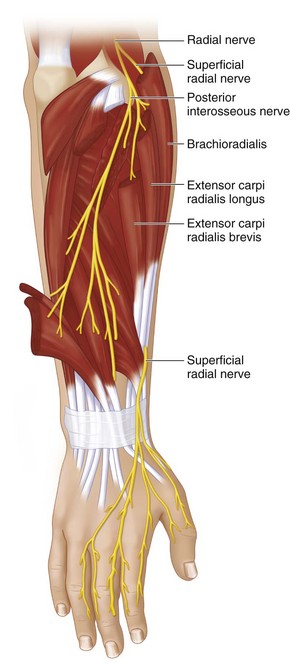
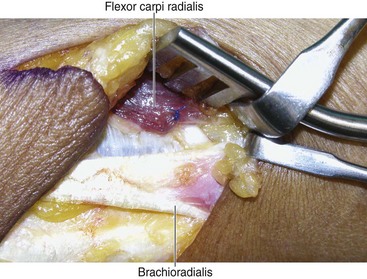
 Although a neuroma can involve any sensory nerve in the hand, the superficial radial nerve is particularly prone to developing a neuroma, and these neuromas are difficult to manage. The nerve becomes subcutaneous about 7 cm proximal to the radial styloid by piercing the fascia between the brachioradialis (BR) and the extensor carpi radialis longus (ECRL) (Fig. 17-3). It is believed that the nerve may be compressed between the tendons of the ECRL and BR. In 3% to 10% of the population, it passes through the tendon of the brachioradialis, tethering it proximally. These factors, combined with its superficial location, may explain the predisposition to iatrogenic injury and neuroma formation.
Although a neuroma can involve any sensory nerve in the hand, the superficial radial nerve is particularly prone to developing a neuroma, and these neuromas are difficult to manage. The nerve becomes subcutaneous about 7 cm proximal to the radial styloid by piercing the fascia between the brachioradialis (BR) and the extensor carpi radialis longus (ECRL) (Fig. 17-3). It is believed that the nerve may be compressed between the tendons of the ECRL and BR. In 3% to 10% of the population, it passes through the tendon of the brachioradialis, tethering it proximally. These factors, combined with its superficial location, may explain the predisposition to iatrogenic injury and neuroma formation.
Treatment Options
• Our surgical treatment of neuromas is based on the availability of an appropriate distal nerve, the local tissue environment, and the anatomic zone of the neuroma.
• If an appropriate distal target is available, we use a nerve graft to bridge the defect caused by resection of the neuroma. If the local tissue environment is not suitable for a nerve graft, we wrap the nerve graft in a vein, an artificial nerve conduit, or a locally transposed fat flap.
• If an appropriate target is not available, we resect the neuroma and relocate the proximal end. The relocation of the proximal end depends on the anatomic zone.
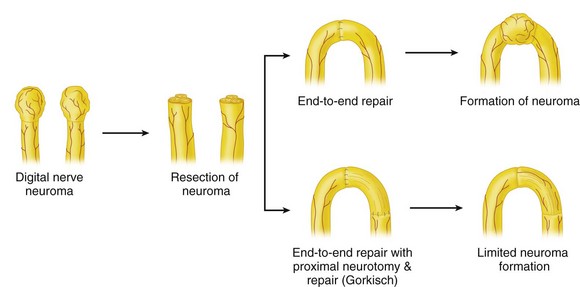
• We have occasionally used the technique of centro-centralization for a digital nerve neuroma. This involves resection of the neuroma and suturing of the digital nerves to each other. Gorkisch and colleagues (1984) suggested dividing one of the digital nerves 5 to 10 mm proximal to the repair site and performing an additional repair. This creates a nerve graft segment and prevents the development of a neuroma at the original nerve repair site (Fig. 17-4).
Positioning
 The procedure is performed under tourniquet control using a 3.0× to 3.5× loupe magnification.
The procedure is performed under tourniquet control using a 3.0× to 3.5× loupe magnification.
 The patient is positioned supine with the affected extremity on a hand table.
The patient is positioned supine with the affected extremity on a hand table.
 If a cable nerve graft is anticipated, the leg should be prepped for harvest of a sural nerve graft. It is better to avoid harvesting a nerve graft from the same limb in patients with complex regional pain syndrome, who have preexisting nerve-related pain/paresthesia, because it adds another nociceptive focus.
If a cable nerve graft is anticipated, the leg should be prepped for harvest of a sural nerve graft. It is better to avoid harvesting a nerve graft from the same limb in patients with complex regional pain syndrome, who have preexisting nerve-related pain/paresthesia, because it adds another nociceptive focus.
Procedure
Available Distal Nerve
Step 1
 A 38-year-old woman presented with tenderness over the superficial radial nerve after release of the first dorsal compartment for de Quervain tendovaginitis. The sensory function of the nerve was intact. She had a Tinel sign in the distribution of the superficial radial nerve on percussion of the scar (see Fig. 17-1).
A 38-year-old woman presented with tenderness over the superficial radial nerve after release of the first dorsal compartment for de Quervain tendovaginitis. The sensory function of the nerve was intact. She had a Tinel sign in the distribution of the superficial radial nerve on percussion of the scar (see Fig. 17-1).
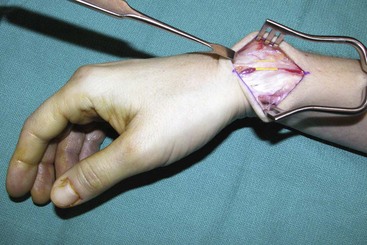
 An incision in line with the previous scar was made and extended proximally and distally (Fig. 17-5).
An incision in line with the previous scar was made and extended proximally and distally (Fig. 17-5).
Step 2
 The nerve was dissected free from all surrounding scar tissue (Fig. 17-6). A decision was made to maintain the nerve in continuity because the patient had intact sensory function. It was decided to cover the nerve with a vein graft to improve the local tissue environment and prevent further scarring around the nerve.
The nerve was dissected free from all surrounding scar tissue (Fig. 17-6). A decision was made to maintain the nerve in continuity because the patient had intact sensory function. It was decided to cover the nerve with a vein graft to improve the local tissue environment and prevent further scarring around the nerve.
Procedure
No Distal Nerve Available
Step 1
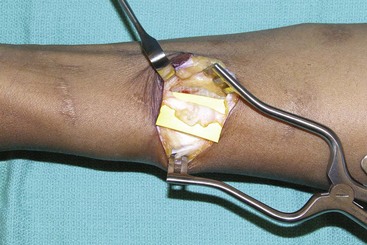
 A 46-year-old woman presented late with severe burning pain over the superficial radial nerve 3 months after a forearm laceration. The laceration was sutured in the emergency department. On examination, the patient had diminished sensation in the first web, and a Tinel sign was localized to the scar.
A 46-year-old woman presented late with severe burning pain over the superficial radial nerve 3 months after a forearm laceration. The laceration was sutured in the emergency department. On examination, the patient had diminished sensation in the first web, and a Tinel sign was localized to the scar.
 An incision was made over the area of tenderness, and the neuroma of the superficial radial nerve was identified and mobilized (Figs. 17-8 and 17-9).
An incision was made over the area of tenderness, and the neuroma of the superficial radial nerve was identified and mobilized (Figs. 17-8 and 17-9).
Step 3
 The fascicles of the superficial radial nerve were gently separated and sutured to the undersurface of the FCR with a few interrupted 8-0 nylon sutures (Fig. 17-10).
The fascicles of the superficial radial nerve were gently separated and sutured to the undersurface of the FCR with a few interrupted 8-0 nylon sutures (Fig. 17-10).
 A single 5-0 Prolene suture was used to suture the nerve to the muscle sheath proximally to reduce the tension on the distal nerve fascicle-muscle suture (Fig. 17-11).
A single 5-0 Prolene suture was used to suture the nerve to the muscle sheath proximally to reduce the tension on the distal nerve fascicle-muscle suture (Fig. 17-11).
Procedure
Centro-Centralization of a Digital Nerve
Step 1
 A 43-year-old woman presented with pain at the tip of an index finger amputation stump. She had undergone an amputation of the index finger through the middle phalanx following a table saw injury 6 months previously, and her symptoms had not resolved with conservative measures.
A 43-year-old woman presented with pain at the tip of an index finger amputation stump. She had undergone an amputation of the index finger through the middle phalanx following a table saw injury 6 months previously, and her symptoms had not resolved with conservative measures.
 Bilateral midaxial incisions were made and a palmar skin flap elevated (Fig. 17-12).
Bilateral midaxial incisions were made and a palmar skin flap elevated (Fig. 17-12).
 The digital nerves were identified in the proximal part of the incision and followed distally to a large neuroma of the radial digital nerve and a smaller neuroma of the ulnar digital nerve (Fig. 17-13).
The digital nerves were identified in the proximal part of the incision and followed distally to a large neuroma of the radial digital nerve and a smaller neuroma of the ulnar digital nerve (Fig. 17-13).
Postoperative Care and Expected Outcomes
 A splint is not applied, and patients are started on early mobilization to allow the nerve to glide within the tissue planes and decrease adhesions. Prevention is the best treatment of neuromas. One should be especially careful when operating in the vicinity of the superficial radial nerve.
A splint is not applied, and patients are started on early mobilization to allow the nerve to glide within the tissue planes and decrease adhesions. Prevention is the best treatment of neuromas. One should be especially careful when operating in the vicinity of the superficial radial nerve.
 The relocation of neuromas into muscle has given better results compared with burial in bone. Greater than 90% of patients have an improvement in their symptoms.
The relocation of neuromas into muscle has given better results compared with burial in bone. Greater than 90% of patients have an improvement in their symptoms.
Dellon AL, Mackinnon SE. Treatment of the painful neuroma by neuroma resection and muscle implantation. Plast Reconstr Surg. 1986;77:427-438.
Gorkisch K, Boese-Landgraf J, Vaubel E. Treatment and prevention of amputation neuromas in hand surgery. Plast Reconstr Surg. 1984;73:293-299.
Sood MK, Elliot D. Treatment of painful neuromas of the hand and wrist by relocation into the pronator quadratus. J Hand Surg [Br]. 1998;23:214-219.