Pharmacists will no longer be able to keep the difference between the price paid by the government for generic drugs and the lower price charged by the manufacturer. But they will receive $1.1 billion (over 4 years) to compensate for this loss of income.
Although the proposed changes to pharmacy arrangements received positive media coverage, it was also suggested that these changes to the PBS would ‘dismantle’ the reference pricing system (Metherell 2006). As part of these measures, the subsidised prices of medicines that are patented and offer the same health benefit as those that are off-patent (generic) will no longer be linked. This concept, known as ‘reference pricing’, has operated since 1992 and has been a fundamental tenet of the PBS for many years. Basically, the government pays the lowest price for all drugs that offer the same health outcome. For example, drugs which lower blood pressure are all reimbursed at the lowest price, irrespective of whether the product is patented or not. That is why it has been said that the Australian government buys health outcomes, not drugs (Commonwealth of Australia 2005).
This chapter explores the policy measures put forward by Minister Abbott and the claims that they will ensure continued access to prescription drugs for the Australian people, while also controlling PBS expenditure. Consideration will also be given to whether these measures signal a shift in Australian pharmaceutical policy from reference pricing towards purchasing drugs, as against health outcomes.
A ‘WICKED’ PROBLEM
So these were the two problems – overpricing to government and therefore to taxpayers of generics, and the difficulties of reference pricing in the new system of mandatory price cuts. These were the two problems that these changes are designed to address.
The cost of the PBS has long been of concern to government. Although PBS growth in expenditure has slowed to a rate of about 2.7% per annum, and a cost of 6 billion to government (2005–06), it was previously the fastest growing area of Commonwealth health expenditure, with nominal growth of 12% per annum between 1995 and 2004 (Abbott 2006, Commonwealth of Australia 2007). The federal Treasurer, Peter Costello, has repeatedly identified the PBS as a ‘core challenge’ for government spending (Stafford & Allen 2005). Reflecting this challenge, Minister Abbott has also advocated savings on the PBS so that ‘headroom’ can be created to pay for newer, more expensive pharmaceuticals (Abbott 2006). The fact that both ministers agree that action was required to address PBS expenditure draws attention to the problem that exists between delivering PBS outcomes that satisfy both the main stakeholders on the one hand and PBS ‘sustainability’ on the other.
The PBS has been in operation for almost 60 years. It was designed to provide timely and affordable access to prescription drugs for all Australians (Commonwealth of Australia 2005). It operates as a reimbursement scheme: consumers pay a fixed co-payment for their drug(s) and the government reimburses community pharmacists the difference. For example, a drug which costs $56.00 to government will cost general patients $30.70 and concession card holders, $4.90.
For a drug to be listed on the PBS it must satisfy quality, safety and efficacy criteria. This is primarily assessed by the Therapeutic Goods Administration (TGA). In addition, the cost effectiveness and comparative effectiveness to existing therapies must be assessed by the Pharmaceutical Benefits Advisory Committee (PBAC). Under the National Health Act 1953 a drug that is substantially more costly than alternatives may not be added to the PBS formulary unless, for some patients at least, it confers an additional benefit.
Consistent with this legislative mandate is the concept of reference pricing. As noted above, reference pricing pays a set amount for a therapeutic outcome. Economic evaluation, including cost-effective analysis, provides the tools to determine the value (expressed as a price) of this outcome. It also means that if there are any price changes to the drugs in a therapeutic group (i.e. through a new drug being listed on the PBS that is considerably cheaper than that already listed) these are extended to other drugs in the groups, irrespective of patent status. Usually this is seen when a generic pharmaceutical enters the market at a lower price than the originator brand, either through the government’s policy of a mandatory 12.5% reduction for new drugs being listed, or through the manufacturer offering a lower price to government.
These provisions have caused the pharmaceutical industry considerable angst, both domestically and internationally. The industry has argued that this policy does not adequately reward innovation and undermines the value of pharmaceutical patents (Pharmaceutical Research and Manufacturers of America [PhRMA] 2007).
A consequence of this policy is that the price of generic drugs has remained high in comparison to those that are protected by patents. In an attempt to achieve greater price reductions when the new brands (generics) enter the market, the government introduced the 12.5% reduction policy in 2005. When the first new brand of a medicine is listed on the PBS, a mandatory 12.5% price reduction for all medicines is applied to all medicines in the reference pricing group (Commonwealth of Australia 2005). Usually, this occurs around the time of patent expiry. Once a group received a 12.5% cut, further reductions would not be made when other brands were listed. This proposal was expected to generate savings of about $800 million (Commonwealth of Australia 2005).
Concern over the prices of generic drugs was heightened by the knowledge of imminent patent expiries on a number of ‘blockbuster’ drugs. Over the next 10 years, the patent for over 100 drugs will be expiring (Commonwealth of Australia 2007). When a pharmaceutical patent expires, it is possible for a generic manufacturer to enter the market with an identical product at a considerably lower cost. In Australia, these discounts are typically offered by generic manufacturers to pharmacists and the government was keen to capture these savings.
THE POLICY RESPONSE
On 16 November 2006, Minister Abbott announced a package of PBS-related reforms. Further detail was provided on 2 February 2007. The initial response from stakeholders to the November 2006 announcement was positive, with its promise of considerable savings for consumers. The fine print released in February 2007 failed to attract widespread attention.
The government put forward a ‘range of inter-connected measures’, which included:
- changes to the pricing of PBS-listed medicines
- the introduction of compensation arrangements for pharmacy and pharmaceutical wholesalers
- streamlined authority approvals for some medicines
- the establishment of an access medicines working group made up of government and industry representatives (Commonwealth of Australia 2007).
- the introduction of compensation arrangements for pharmacy and pharmaceutical wholesalers
Each of these measures will be considered in turn.
Changes to the pricing of PBS-listed medicines
This is perhaps one of the most significant policy revisions in the history of the PBS. Rather than being listed on a single formulary, from 1 August 2007, the PBS schedule will comprise two separate formularies. There will be no price linkages between the formularies and the system of reference pricing will no longer apply across the entire PBS. Instead, it will be applied with limitations. In addition, pharmaceutical manufacturers will be forced to disclose to the government the price at which a drug is sold for new drugs listed on the PBS. A summary of these changes appears in Box 17.1.
BOX 17.1 SUMMARY OF PRICING REFORMS
- Creation of two PBS formularies; Formulary 1 (F1) and Formulary 2 (F2).
- Different pricing strategies for each formulary.
- No price linkages between the two formularies.
- Drugs will be able to move between formularies.
- Different pricing strategies for each formulary.
- Single brands (only one medicine of its type listed on the PBS).
- Typically will include on-patent drugs and often first drug of its type to be listed on the PBS.
- No price cuts.
- For medicines in the same reference pricing group, standard reference pricing arrangements apply; that is, the government pays the same price for the same health outcome.
- Typically will include on-patent drugs and often first drug of its type to be listed on the PBS.
- Multiple brands and the creation of two groups with different pricing arrangements.
- Typically will include medicines that are interchangeable at the patient level and where generic drugs are available.
- Staged price cuts (2% per year for 3 years, from 1 August 2008).
- Price disclosure arrangements apply from 1 August 2007.
- Will not impact price until 1 August 2009 and will only be applied if the weighted average disclosed price is 10% more than what is currently being paid.
- Price disclosure arrangements apply from 1 August 2007.
- 25% one-off cut (but for some products this will be phased over life of the patent).
- 12.5% price reduction policy still applies for new brands entering the market.
- Price disclosure arrangements apply from 1 Jan 2011.
- Will not impact price until 1 August 2012 and will only be applied if the weighted average disclosed price is 10% more than that is currently being paid.
- 12.5% price reduction policy still applies for new brands entering the market.
The trigger for price disclosure is the listing of a new product on the PBS. All other suppliers of that product will be invited to disclose the price at which they sell their medicine.
Medicines will only be listed on one formulary. For medicines that have multiple strengths and brands, the entire molecule will be listed on F2.
Importantly, there will be no price links between the medicines listed on F1 and F2. This is a significant deviation from what has been considered a fundamental principle of the PBS. It is conceivable that there will be drugs on F1 that offer the same health benefit as those listed on F2. For example, selective serotonin reuptake inhibitors (SSRIs) will be split between F1 and F2 as they are not interchangeable at the patient level. It remains to be seen whether there will be significant price differences between those listed on F1 to F2.
Price reductions
All products on F2 will be subject to mandatory price reductions and there will be a requirement that the price at which they are being sold by the pharmaceutical manufacturer to the pharmacist be disclosed. Price disclosure will not be retrospective and will apply to new listings on the PBS. This was introduced so that the government could further benefit from the introduction of generic drugs, which are priced at significantly lower levels than their (identical) branded counterparts.
The intent of these changes is to ensure that the price that the government pays is closer to the price at which it is being sold. To stimulate this, the government has proposed that mandatory price reductions be applied to F2:
- F2A – drugs that are being discounted by less than 25% to pharmacists as at 1 October 2006
- F2T – drugs that are being discounted by more than 25% to pharmacists as at 1 October 2006.
All medicines listed on F2A will be subject to staged price reductions of 2% per year for 3 years, commencing on 1 August 2008. The 12.5% price reduction policy will continue to apply, where relevant.
For drugs listed on F2T, a one-off mandatory price reduction will be applied on 1 August 2008. The 12.5% price reduction policy will apply when new drugs are listed, and the principles of reference pricing will apply in F2T as price reductions will ‘flow-on’ to all brands, forms and strengths of that drug, and to drugs that are interchangeable with that medicine. It should be noted that, for a ‘defined list of patented medicines’ on F2T, the 25% price reduction will be phased over the remaining patent life (approximately 5–10 years), which will delay the savings achievable by this measure.
Price disclosure
Both F2 formularies will be subject to price disclosure arrangements but implementation will be phased over 4 years.
From 1 August 2007, any new listings on F2A must disclose the ‘actual market price’ as a condition of listing. The staged price reduction of 2% per annum will apply until the price of that pharmaceutical reaches the disclosed price. Further reductions will be applied from 2009 on the basis of information provided as part of the listing process and will continue on an annual basis.
Drugs on F2T will be required to disclose the ‘actual market price’ as a condition of listing from 1 January 2011. The price reduction that results from price disclosure will take effect from 1 August 2012. These reductions will reflect the weighted average disclosed price, and prices will then be adjusted annually to reflect this average.
Pharmaceutical products will be able to move between the formularies, with F1 medicines likely to move to F2A once generic brands enter the market. The pricing rules for F2A would then be applied but delayed by 1 year before taking effect (1 August 2009). This could also potentially delay or reduce the savings achieved by government.
The government has sought to define how these arrangements might work. In short, price disclosure will be triggered when a new brand of a drug already on the PBS is listed. For pharmaceuticals listed on F2A this begins on 1 August 2007 and for those on F2T on 1 January 2011. Importantly, unless the 12.5% or the 2% price reduction applies, the initial listing price of the new brand will be the same as those already listed on the PBS (not dissimilar to current arrangements) but the supplier will be required to disclose to the Department of Health and Ageing (DOHA) the actual price at which this drug is sold to wholesalers and/or pharmacies.
Once this has been disclosed, DOHA will then invite other suppliers of the same medicines to disclose their price. This will then form the basis for the calculation of the weighted average price and possibly trigger further price reductions. If the price reduction is less than 10% of the PBS ex-supplier price, the price reduction will not apply. If the reduction is greater than 10%, the weighted average disclosed price will be the subsidised price, rather than the disclosed price.
Compensation arrangements for pharmacists and wholesalers
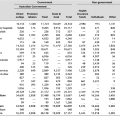
Around 30% of PBS expenditure is directed towards pharmacists and wholesalers. This is in addition to the payments that pharmacists receive for dispensing PBS medicines under the 4th Community Pharmacy Agreement (CPA).
To encourage pharmacists to dispense generic drugs or ‘substitutable, premium-free medicine’ an incentive of $1.50 will be paid, in addition to the dispensing fee (Commonwealth of Australia 2007). This payment does not apply to pharmaceuticals that are priced ‘under the co-payment’ or for private scripts. In addition, for scripts processed as part of PBS Online (a program developed by the government designed to reduce the administrative burden of the PBS and being implemented in all pharmacies) an incentive of 40c will be paid. Pharmacy mark-ups and dispensing fees will also increase. These measures will cost the government $1.1 billion.
As part of the remuneration arrangements, pharmaceutical wholesalers receive a proportion of the value of each product sold. Once the mandatory price reductions and price disclosure arrangement are fully implemented, the margins for pharmaceutical wholesalers will be reduced. To compensate for this, pharmaceutical wholesalers that supply predominantly rural and remote areas will be eligible for additional funding.
Streamlining authority approvals for some medicines
For some pharmaceuticals listed on the PBS prior approval to prescribe must be obtained from Medicare Australia. Usually, this means that patients must meet certain criteria and additional work by prescribers is required. These arrangements have often been described as draconian and excessively bureaucratic by the Australian Medical Association (AMA 2006).
As part of these reforms, the number of drugs requiring the approval of Medicare Australia will be reduced and the process for obtaining approval has been simplified. This will apply to drugs used in the treatment of certain chronic conditions. Approval for repeat prescriptions will no longer be required under these arrangements, once initial approval has been granted.
Access to medicines working group and stakeholder engagement
Since the adoption of the National Medicines Policy in 2000, a ‘partnership approach’ has been applied to developing and implementing pharmaceutical policy in Australia. The health of this partnership has waxed and waned, but more recently the government has actively sought to work collaboratively with the pharmaceutical industry and its peak body, Medicines Australia (MA).
In light of this, a MA–DOHA Access to Medicines working group will be established to consider ‘timely and appropriate access to new medicines for the PBS’ (Commonwealth of Australia 2007). This is a variation on what has been described as the objective of the PBS. It may signal a shift away from the currently stated objective of affordable access (although it could be argued appropriate access could entail affordable access). It also creates a structure that further links the pharmaceutical industry and the government.
In addition to the Access to Medicines working group, DOHA will establish a stakeholder reference group to provide a forum for discussing implementation of these reforms. This stakeholder reference group reflects the major stakeholders in pharmaceutical policy in Australia with the notable omission of PBAC. It should be noted that PBAC is an important player in these reforms as it is the only body from which the minister can accept recommendations when making decisions about listing drugs on the PBS.
SOLUTIONS OR LONG-TERM PROBLEM?
Healthcare is a high cost area of public expenditure where it has proved difficult for governments to make significant savings – unless services are no longer provided. It is rare for a federal budget not to include a PBS cost-saving initiative. Numerous cost-containing attempts have been implemented over recent years, including increasing co-payments, changing safety net arrangements or de-listing drugs. These measures have had a minimal impact on the cost of the PBS, although the measures introduced in the 2005–06 budget did play a substantive role in slowing the growth of PBS expenditure (Abbott 2006).
There were two main objectives for the measures put forward: the first was to ensure that Australians had continuing access to prescription drugs, and the second was to reduce overall PBS expenditure, so that newer drugs could be listed. Although these objectives may appear to be contradictory, the focus of these measures was on reducing the price of generic drugs by mandatory price cuts and price disclosure arrangements as well as de-linking these products from patented drugs.
At first glance it appears likely that these reforms will generate some savings to the PBS. Mandatory 25% cuts to some products and staged reductions to others, while at the same time maintaining the current 12.5% reduction policy and elements of the reference pricing system, will all reduce PBS expenditure in the short term. Whether the long-term savings will be realised, or offset by the pharmacy compensation package, will not be known for some time.
Arrangements for pharmacists
These savings are predicated on price disclosure arrangements and that the disclosed price reflects the ‘true’ price. They also rely on ‘non-cash’ arrangements, such as two-for-one deals and ‘product bundling’, to be disclosed and appropriately factored in to the calculations.
It is noteworthy that these reforms have long lead times for implementation. The cost of healthcare is dynamic and it remains to be seen whether the price paid 12 months ago reflects what is being paid at the time when the first price cut is introduced. It is not unreasonable to expect that the manufacturers/pharmaceutical suppliers would change their pricing structure in that time. It is unclear whether suppliers will be subject to regular price disclosure arrangements or whether the disclosure will only apply at the time of listing.
Another purpose of the price disclosure arrangements is to reveal the arrangements between pharmaceutical suppliers and pharmacists. This information would ensure that the price paid by government more closely reflects the price at which it is sold. A similar concept was introduced in Korea in 1999 when the government introduced a ‘no margin’ policy and slashed the reimbursement level for drugs. This led to price collusion and consumers having to pay more for drugs as the price cut was passed on to consumers (Kwon 2003). Although Australian consumers are protected by a fixed co-payment, taxpayers are not, and the prospect of price collusion cannot be dismissed.
When the reform package was announced, the president of the Pharmacy Guild, Kos Sclavos, stated that the profession accepted the disclosure arrangements to protect its ‘good name’ (Metherell 2006). Although these reforms will have an impact on the revenue for pharmacists, a $1.1 billion compensation package will be paid until 2011. This compensation package will be paid to pharmacists, irrespective of whether these savings are achieved. In short, if these savings are not made, the government will be spending net additional money on the PBS.
It could also be expected that the compensation arrangements will be an ongoing feature of pharmacy remuneration arrangements. The current CPA is due to expire in 2010 and if the increased dispensing fee (which takes into account the bonus for these reforms) forms part of the negotiations of the next CPA, it will ensure that the government will continue to pay a high price to pharmacists.
Another aspect of price disclosure that deserves greater exploration is the calculation of the weighted average disclosed price. Admittedly little detail has been released and, according to the fact sheet released by government, the arrangements are being further refined. However, it could be assumed that the government will achieve less savings if prices are based on an average weighted price, rather than the disclosed price to government. For high volumes products, the ‘lost’ savings would be significant.
Furthermore, this system could also be ‘gamed’ by the pharmaceutical industry, so that price reductions are minimal. For products that have already received a 12.5% or 2% reduction, there is no incentive for a lower price to be offered to government. It also encourages the practice of pseudo-generics whereby branded products enter into a licensing agreement with a generic manufacturer to artificially inflate price while maintaining market share. These arrangements are a dominant feature of the Australian generic scene (Faunce et al. 2006). Pseudo-generics have created similar market distortions in Canada (Hollis 2003).
In an attempt to gain market share, it is likely that that the generic manufacturer (or wholesaler) would offer non-cash benefits to a pharmacy. Under the new arrangements these practices need to be disclosed and will be incorporated into the calculations for price reduction. If the total of value of these benefits was calculated within a 10% margin of the listed price, a price reduction would not be triggered. This is particularly important if no price reductions are applied and/or offered. Furthermore, it also would be difficult to quantify the value of non-cash benefits, notwithstanding the auditing requirements. Once again, potential for savings is undermined.
Reference pricing
The long-term impact of the changes to reference pricing cannot be underestimated. A shift away from reference pricing would signal the abandonment of a system of paying for health outcomes. These measures were identified by the Pharmaceutical Research and Manufacturers of America (PhRMA) as ‘significant change in course for the Australian system’ (PhRMA 2007). PhRMA has openly lobbied both the Australian and US governments for the reference pricing system to be dismantled, arguing that it undermines the value of a patent and does not adequately reward research and innovation.
The split in formularies effectively shields most patented products from any price cuts and will ensure that the government will continue to pay a high, or higher, prices for products which are deemed not interchangeable at the patient level. This will encourage the pharmaceutical industry to demonstrate that their products are not substitutable rather than introduce new medicines (Stafford 2006).
The potential implications of these changes to reference pricing can be demonstrated by the selective serotonin reuptake inhibitors (SSRIs). This group of drugs are not considered to be interchangeable at the patient level but are considered to offer the same health outcome at the population level. While the formulary lists have not yet been released it could be assumed from the information available that, for the SSRIs that have multiple brands, these will be listed on F2 and subject to mandatory price cuts and price disclosure arrangements. Those which are a single brand product will be listed on F1 and be protected by price cuts. When the first price cuts are applied, there will be a price differential between the SSRIs listed on F1 to those listed on F2. What makes the impact of the price differential significant is the volumes associated with SSRIs. These drugs are consistently in the top 10 drugs by volume.
Policy advocates in the United Kingdom were not attracted to the Australian reforms. Less than three months after the Australian government announced the reforms, the Office of Fair Trading in the United Kingdom released a report advocating, inter alia, that there should be a shift from a system of price disclosure to a ‘a value-based approach to pricing, which would ensure the price of drugs reflect the clinical and therapeutic value to patients and the broader NHS’ (Office of Fair Trading 2007). What is being recommended more closely resembles the PBS, prior to these reforms being announced.
FUTURE DIRECTIONS FOR POLICY DEVELOPMENT
Understandably, perhaps, Australian governments of both persuasions have declined to define what it means for the PBS to be ‘sustainable’. Arguably, the sustainability of any government program can be attributed to the political will to maintain it. Nevertheless, in an attempt to ensure the ongoing financial sustainability of the PBS, Minister Abbott has put forward a complex structure which relies on the goodwill of the stakeholders to achieve savings. There are no guarantees that these savings will be realised and the system will be much harder to change when, and if, a future government seeks to ‘reform the reform’.
Australia already pays high prices for many new drugs. Recently Danzon and Furukawa (2006) showed that the prices of biologicals in Australia were similar to those in the US. Further research has demonstrated that the Australian government, on average, pays more than the US government for medicines that represent significant advances in therapy (Roughead et al, forthcoming). This may seem unexpected given the economic evaluation process that underpins PBS listing is generally perceived to have a downward impact on price. More and more, however, it appears that for newer medicines which represent a significant advance in therapy the trend is towards narrower PBS restrictions in which a higher price can be justified, rather than lower prices reflecting cost effectiveness across a broader population.
It remains to be seen whether the measures put forward by the government will further influence this trend. One of the most important remaining questions about these reforms is their potential impact on PBAC’s evaluation process and what effect these changes will have on reference pricing in the longer term. It is particularly concerning that, from the information publicly available, PBAC is notably absent from the stakeholders consulted about these reforms.
The price of the comparator is a key input to the evaluation of cost-effectiveness analysis made by PBAC. A higher priced comparator makes the cost-effectiveness ratio appear more favourable. If, over time, fewer and fewer drugs on the PBS are subject to full reference pricing this has the potential to distort the analysis and could result in higher prices at listing. If the prices of ‘cost-effective’ drugs are higher than would otherwise have been the case the projected savings may evaporate. Australia may find that, in the future, its drug prices are among the highest in the developed world.
The watering down of reference pricing and the de-linking of the prices of patented and non-patent drugs deserves greater consideration. PhRMA has attributed this change in policy to implementation of the principles of the Australia–United States Free Trade Agreement (AUSFTA) (PhRMA 2007). This has not been supported in any of the public statements by Minister Abbott on these reforms. Both the Minister for Health and the Prime Minister maintain that the fundamental architecture of the PBS will not change as a result of AUSFTA. One can therefore reasonably conclude that these reforms have happened not because of, but in spite of, the AUSFTA. Despite assertions to the contrary, the fundamental listing and pricing mechanisms were preserved in this trade agreement.
Australia has been the world leader in the application of economic evaluation to pharmaceutical reimbursement systems and many countries have sought to emulate aspects of the Australian approach as a means of ensuring the affordable access to medicines while balancing the interests of other stakeholders in the system, including taxpayers, pharmacists and the pharmaceutical companies. The proposed reforms appear to be a substantial weakening of both the principle and practice that has kept the PBS both affordable and equitable to date. Clearly, however, it will be some years before the full effects of these reforms will be apparent.
Note: The views expressed in this chapter are the authors and do not necessarily reflect those of the Commonwealth of Australia.
References
Endnote