History: A 70-year-old woman presents with gastroesophageal reflux symptoms.
1. Which of the following should be included in the differential diagnosis of this case? (Choose all that apply.)
A. Benign lymphoid hyperplasia
B. Brunner’s gland hyperplasia
2. What can occur as a response to increased acidity in the duodenal bulb?
A. Benign lymphoid hyperplasia
B. Brunner’s gland hyperplasia
3. Which of the following polyposis syndromes does not involve the duodenum?
A. Familial adenomatous polyposis
4. What is the most common benign tumor of the duodenum?
ANSWERS
CASE 17
Heterotopic Gastric Mucosa of the Duodenum
1. A, B, C, and E
2. B
3. D
4. D
References
Levine MS, Rubesin SE, Herlinger H, et al: Double-contrast upper gastrointestinal examination: technique and interpretation. Radiology. 1988;168:593–602.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 96.
Comment
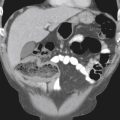
It is not uncommon to encounter nodular filling defects within the duodenal bulb. These may be solitary or multiple and are of variable size. Certain distinguishing features can help differentiate the conditions that are known to produce this radiologic appearance.
Heterotopic gastric mucosa in the duodenal bulb occurs more commonly than most radiologists recognize, occurring in up to 20% of patients in some pathologic series but seen in less than 1% of patients in radiologic series. The radiologic appearance is that of slightly elevated lesions of varying sizes measuring only a few millimeters in diameter and often clustered in a mosaic pattern in the base of the duodenal bulb (see figure). A distinguishing feature is their sometimes angulated or plaque-like margins. These lesions are believed to have no clinical significance.
Benign lymphoid hyperplasia of the bulb and proximal duodenum is characterized by multiple tiny (1- to 2-mm), smooth filling defects, which are usually diffuse throughout the region. Often there is no known reason for their appearance, but they occur more commonly in patients with decreased immune competence, such as those with hypogammaglobulinemia or agammaglobulinemia.
Brunner’s gland hyperplasia has a different radiologic appearance than the two aforementioned entities. The filling defects in this condition are larger, often ranging up to 1 cm. These lesions are smooth and diffuse, often producing a cobblestone appearance. They may be associated with hyperacidity, although this belief is not universally accepted, given the high incidence of hyperacidity disease and the low incidence of Brunner’s gland hypertrophy. However, acidity might be a contributing factor.
The possibility of pancreatic rests, either single or multiple, giving rise to a polypoid filling defect in the duodenal bulb, should also be considered. A tiny barium collection, which can at times be seen in the center of these filling defects, is the orifice of a duct, and such a finding is an extremely important diagnostic finding.
Benign tumors of the duodenum, such as leiomyomas (GIST), adenomas, and neurofibromas, occur more commonly in the proximal duodenum, particularly the duodenal bulb. Also, polyposis syndromes, such as Peutz-Jeghers, Cronkhite-Canada, and familial polyposis syndromes, are known to cause multiple polyps in the duodenum.