CASE 160
History: A 54-year-old woman presents with intermittent nausea, vomiting, and diarrhea.
1. What should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
2. In patients with Crohn’s disease, what area of the stomach is most commonly involved?
3. When Crohn’s disease is long-standing, the antrum and duodenum become a featureless rigid tube. What is the name given to this sign?
4. Crohn’s disease is one of many granulomatous diseases that may involve the stomach. Which is the most common in a Western hemisphere population?
ANSWERS
CASE 160
Crohn’s Disease of the Stomach
1. A, C, D, and E
2. B
3. B
4. C
References
Horsthuis K, Bipat S, Bennink RJ, et al: Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008;247(1):64–79.
Wills JS, Lobis IF, Denstman FJ. Crohn disease: state of the art. Radiology. 1997;202(3):597–610.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 69.
Comment
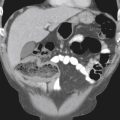
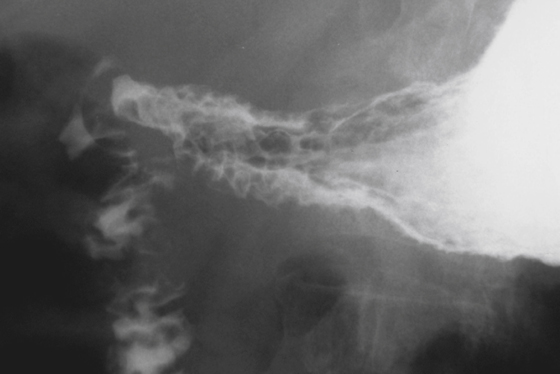
Crohn’s disease of the stomach is usually found in the distal aspect of the stomach but rarely may involve the entire organ. The antrum is first to become involved, and the disease may spread more proximally. Fundal involvement is unusual. Many patients also have associated involvement of the duodenum (see the figure). The stomach is rarely the only part of the gut that is involved by Crohn’s disease; most often, there is ileal or colonic Crohn’s disease as well, and it should be assumed that there is disease in other portions of the GI tract, too. The incidence of Crohn’s disease involving the stomach ranges from 5% to 40% of cases. A much higher incidence is reported in Japan than in North America.
The most common manifestation of Crohn’s disease in the stomach is gastric erosions. These erosions are identical to other types of erosions in the stomach, and there is no way to distinguish them radiologically. As the disease progresses, the severity of the inflammation may increase, and ulcers may become confluent and linear or stellate in configuration. As with other portions of the GI tract, the inflammation is transmural, resulting in fibrosis and scarring. Typically (according to some reports, in more than half of the cases of gastric Crohn’s disease), there may be involvement of the adjacent duodenum.
When Crohn’s disease is long-standing, the antrum and duodenum become a featureless rigid tube; this presentation is called the “ram’s horn” sign because of the conical antrum and widening funnel of the body and fundus. This configuration may be so severe that it resembles a scirrhous carcinoma or any condition that might give a linitis plastica appearance to the stomach. Fistulas are a rare complication of gastric Crohn’s disease but can develop into the transverse colon. Postinflammatory polyps may develop as a sequela of Crohn’s disease of the stomach as they do elsewhere in the gut, especially in the colon.