Procedure 16 Treatment of a Nerve Gap in the Hand
Indications
 A segmental defect in a nerve can result from the following:
A segmental defect in a nerve can result from the following:
 Nerve grafting should be considered in the following cases:
Nerve grafting should be considered in the following cases:
Examination/Imaging
Clinical Examination
 The possibility of nerve grafting should be discussed for all patients in whom a digital nerve injury is suspected. Potential nerve graft sources and their morbidity should also be discussed (detailed later). It is better to avoid harvesting a nerve graft from the same limb in patients who have preexisting nerve-related pain/paresthesia because it adds another nociceptive focus.
The possibility of nerve grafting should be discussed for all patients in whom a digital nerve injury is suspected. Potential nerve graft sources and their morbidity should also be discussed (detailed later). It is better to avoid harvesting a nerve graft from the same limb in patients who have preexisting nerve-related pain/paresthesia because it adds another nociceptive focus.
 It may be difficult to establish sensory loss in children. The absence of wrinkling following immersion of the child’s hand in warm water for 5 to 7 minutes indicates loss of sympathetic innervation and can help with diagnosis.
It may be difficult to establish sensory loss in children. The absence of wrinkling following immersion of the child’s hand in warm water for 5 to 7 minutes indicates loss of sympathetic innervation and can help with diagnosis.
Surgical Anatomy
 A variety of substitutes have been described for reconstituting nerve defects. They include nerve (autograft/allograft), biological conduits (e.g., vein, muscle), and artificial conduits (e.g., polyglycolic acid, nanofiber).
A variety of substitutes have been described for reconstituting nerve defects. They include nerve (autograft/allograft), biological conduits (e.g., vein, muscle), and artificial conduits (e.g., polyglycolic acid, nanofiber).
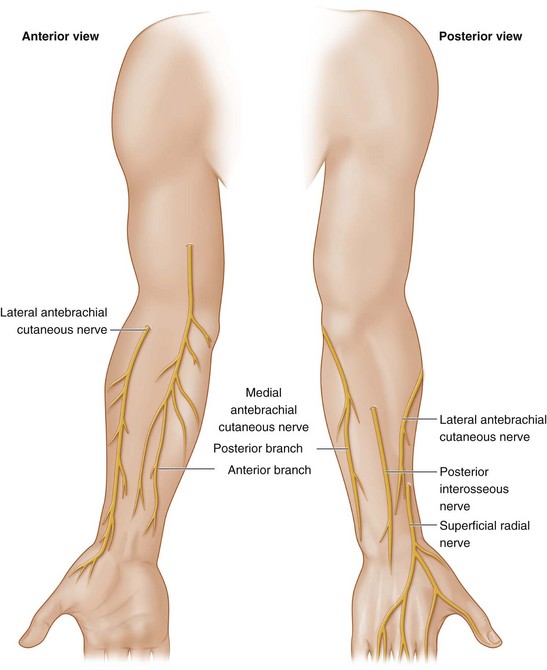
 The available nerve autografts include the posterior interosseous nerve (PIN), superficial radial nerve, medial and lateral antebrachial cutaneous nerves, and sural nerve (Fig. 16-4). We do not use the superficial radial nerve or the lateral antebrachial cutaneous nerves because they provide innervation to potentially valuable areas of skin.
The available nerve autografts include the posterior interosseous nerve (PIN), superficial radial nerve, medial and lateral antebrachial cutaneous nerves, and sural nerve (Fig. 16-4). We do not use the superficial radial nerve or the lateral antebrachial cutaneous nerves because they provide innervation to potentially valuable areas of skin.
 PIN: The distal portion of the PIN is a purely sensory nerve that innervates the wrist joint. It is identified in the radial aspect of the floor of the fourth extensor compartment deep to the tendons of the extensor digitorum communis (EDC) and the extensor indicis proprius (EIP). It can then be followed proximally for a distance of 5 to 7 cm adjacent to the posterior interosseous artery on the dorsal aspect of the interosseous membrane. It has a cross-sectional area of approximately 0.5 to 0.8 mm2 and contains one to two fascicles.
PIN: The distal portion of the PIN is a purely sensory nerve that innervates the wrist joint. It is identified in the radial aspect of the floor of the fourth extensor compartment deep to the tendons of the extensor digitorum communis (EDC) and the extensor indicis proprius (EIP). It can then be followed proximally for a distance of 5 to 7 cm adjacent to the posterior interosseous artery on the dorsal aspect of the interosseous membrane. It has a cross-sectional area of approximately 0.5 to 0.8 mm2 and contains one to two fascicles.
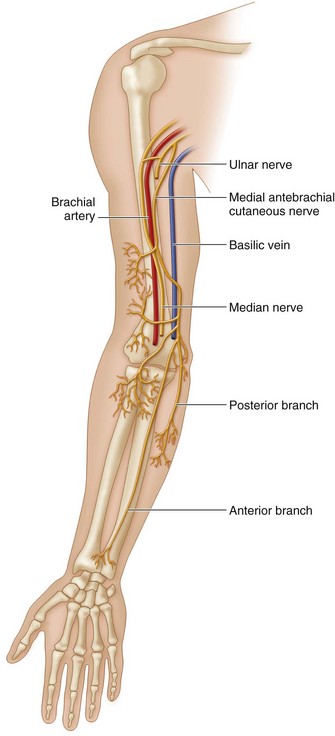
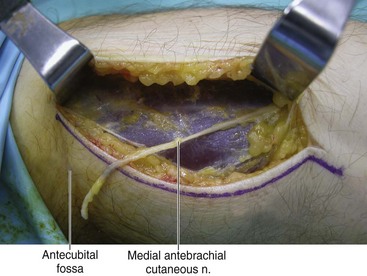
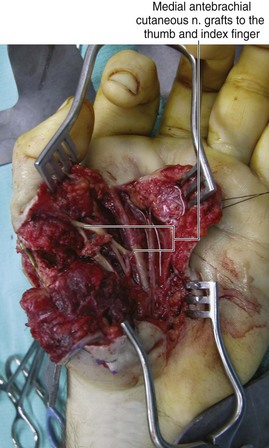
 Medial antebrachial cutaneous nerve (MABCN): This is a purely sensory nerve that arises directly from the medial cord of the brachial plexus (C8, T1) and runs along the axillary vein. It then accompanies the basilic vein in the proximal half of the arm and pierces the deep fascia in the midarm. It splits into anterior and posterior branches in the distal third of the arm. The anterior branch innervates the anteromedial surface of the forearm, whereas the posterior branch innervates the posterior and ulnar aspect of the elbow and forearm (Fig. 16-5). The anterior branch of MABCN is used for nerve graft harvest to avoid sensory loss over the elbow. The anterior branch crosses the elbow between the medial epicondyle and the biceps tendon, usually in front of the antecubital vein, and courses superficial to the flexor carpi ulnaris muscle, ending 10 cm from the wrist. A 20-cm long graft can be harvested based on the anterior branch. It has a cross-sectional area of approximately 0.6 to 1 mm2 and contains three to four fascicles.
Medial antebrachial cutaneous nerve (MABCN): This is a purely sensory nerve that arises directly from the medial cord of the brachial plexus (C8, T1) and runs along the axillary vein. It then accompanies the basilic vein in the proximal half of the arm and pierces the deep fascia in the midarm. It splits into anterior and posterior branches in the distal third of the arm. The anterior branch innervates the anteromedial surface of the forearm, whereas the posterior branch innervates the posterior and ulnar aspect of the elbow and forearm (Fig. 16-5). The anterior branch of MABCN is used for nerve graft harvest to avoid sensory loss over the elbow. The anterior branch crosses the elbow between the medial epicondyle and the biceps tendon, usually in front of the antecubital vein, and courses superficial to the flexor carpi ulnaris muscle, ending 10 cm from the wrist. A 20-cm long graft can be harvested based on the anterior branch. It has a cross-sectional area of approximately 0.6 to 1 mm2 and contains three to four fascicles.
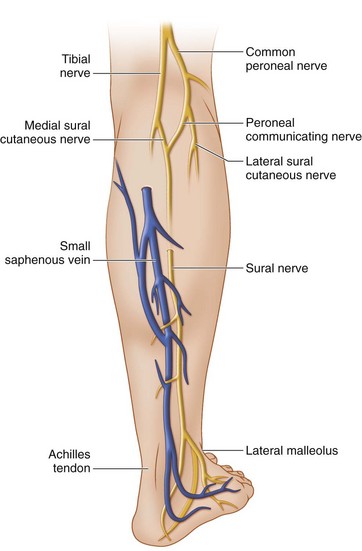
 Sural nerve: The sural nerve is a purely sensory nerve formed by the union of the medial and lateral sural cutaneous nerves (sural communicating nerve). The medial sural cutaneous nerve arises from the tibial nerve and pierces the deep fascia of the leg between the heads of the gastrocnemius in the upper third of the leg. It is then joined by the lateral sural cutaneous nerve branch of the peroneal nerve to form the sural nerve. The sural nerve descends along the lateral margin of the Achilles tendon with the small saphenous vein between the lateral malleolus and the calcaneus (Fig. 16-6). It innervates the lateral aspect of the lower third of the leg and the lateral aspect of the ankle, heel, and foot. A 40-cm–long graft can be harvested based on the sural nerve and medial sural cutaneous nerves. The sural nerve has a cross-sectional area of approximately 2.5 to 3.0 mm2 and contains six to eight fascicles.
Sural nerve: The sural nerve is a purely sensory nerve formed by the union of the medial and lateral sural cutaneous nerves (sural communicating nerve). The medial sural cutaneous nerve arises from the tibial nerve and pierces the deep fascia of the leg between the heads of the gastrocnemius in the upper third of the leg. It is then joined by the lateral sural cutaneous nerve branch of the peroneal nerve to form the sural nerve. The sural nerve descends along the lateral margin of the Achilles tendon with the small saphenous vein between the lateral malleolus and the calcaneus (Fig. 16-6). It innervates the lateral aspect of the lower third of the leg and the lateral aspect of the ankle, heel, and foot. A 40-cm–long graft can be harvested based on the sural nerve and medial sural cutaneous nerves. The sural nerve has a cross-sectional area of approximately 2.5 to 3.0 mm2 and contains six to eight fascicles.
Positioning
 The procedure is performed under tourniquet control using 3.0× to 3.5× loupe magnification for the initial dissection and an operating microscope for the nerve repairs.
The procedure is performed under tourniquet control using 3.0× to 3.5× loupe magnification for the initial dissection and an operating microscope for the nerve repairs.
 The patient is positioned supine with the affected extremity on a hand table.
The patient is positioned supine with the affected extremity on a hand table.
 The leg must be prepared and a thigh tourniquet applied, if a sural nerve graft is anticipated.
The leg must be prepared and a thigh tourniquet applied, if a sural nerve graft is anticipated.
Exposures
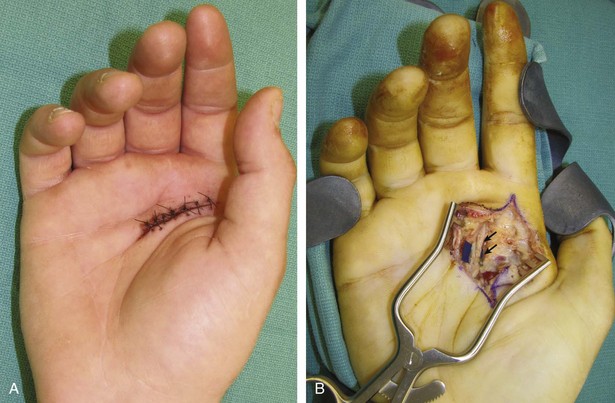
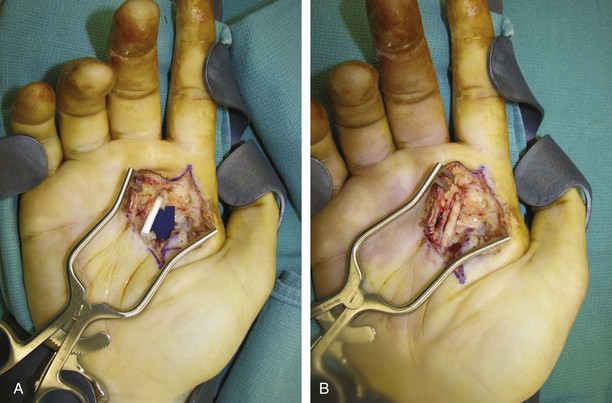
 A Bruner zigzag incision that incorporates any previous lacerations is made. Thick skin flaps are raised in a plane superficial to the tendon sheath (Fig. 16-7B).
A Bruner zigzag incision that incorporates any previous lacerations is made. Thick skin flaps are raised in a plane superficial to the tendon sheath (Fig. 16-7B).
 Nerve grafts should not be harvested until the divided nerve ends have been exposed, the ends have been débrided, and the required length of nerve graft has been calculated.
Nerve grafts should not be harvested until the divided nerve ends have been exposed, the ends have been débrided, and the required length of nerve graft has been calculated.
 The PIN is exposed by a longitudinal incision ulnar to the Lister tubercle. The extensor retinaculum over the fourth compartment is incised, and the tendons of the EDC and EIP are retracted. The PIN is found on the radial aspect of the floor of fourth compartment. Depending on the length of the nerve required, the skin incision can be extended proximally. There is often a bulbous dilation at the distal termination of the PIN. This should be excised. The average length of a PIN graft is usually 4 to 5 cm.
The PIN is exposed by a longitudinal incision ulnar to the Lister tubercle. The extensor retinaculum over the fourth compartment is incised, and the tendons of the EDC and EIP are retracted. The PIN is found on the radial aspect of the floor of fourth compartment. Depending on the length of the nerve required, the skin incision can be extended proximally. There is often a bulbous dilation at the distal termination of the PIN. This should be excised. The average length of a PIN graft is usually 4 to 5 cm.
 The MABCN is exposed by a longitudinal incision on the anteromedial aspect of the forearm at the junction of the proximal and middle third of the forearm. This incision begins 2 cm anterior and 2 to 3 cm distal to the medial epicondyle. The anterior branch of the MABCN can be found within the subcutaneous tissue (Fig. 16-8). If more than one branch is found, the branch that better matches the recipient nerve diameter is selected. Depending on the length of nerve required, the skin incision can be extended proximally.
The MABCN is exposed by a longitudinal incision on the anteromedial aspect of the forearm at the junction of the proximal and middle third of the forearm. This incision begins 2 cm anterior and 2 to 3 cm distal to the medial epicondyle. The anterior branch of the MABCN can be found within the subcutaneous tissue (Fig. 16-8). If more than one branch is found, the branch that better matches the recipient nerve diameter is selected. Depending on the length of nerve required, the skin incision can be extended proximally.
 The sural nerve is exposed by a 2-cm longitudinal incision midway between the lateral malleolus and the calcaneus. It is close to the lateral margin of the Achilles tendon and lies lateral to the small saphenous vein. The required length of the nerve is then dissected proximally. The use of multiple transverse 1-cm stepladder incisions gives a more aesthetic result compared with a single longitudinal incision.
The sural nerve is exposed by a 2-cm longitudinal incision midway between the lateral malleolus and the calcaneus. It is close to the lateral margin of the Achilles tendon and lies lateral to the small saphenous vein. The required length of the nerve is then dissected proximally. The use of multiple transverse 1-cm stepladder incisions gives a more aesthetic result compared with a single longitudinal incision.
Pearls
It is preferable not to cross the web space by the Bruner incision to prevent the development of a contracture band. If an incision needs to extend from the palm to the digit, it is better to leave a small bridge of intact skin at the web and tunnel the nerve graft.
It is important to identify the nerve in normal (uninjured) tissue planes proximal and distal to any existing laceration. These nerves are then followed to find the divided ends that may be encased in scar tissue.
Procedure
Step 1: Preparation of Nerve Ends
 The divided nerve ends are mobilized for 1 to 2 cm depending on the location of injury.
The divided nerve ends are mobilized for 1 to 2 cm depending on the location of injury.
 The nerve ends are then trimmed until healthy fascicles are visualized (Fig. 16-9).
The nerve ends are then trimmed until healthy fascicles are visualized (Fig. 16-9).
Step 1 Pearls
Trimming of the nerve ends should be done conservatively in a graduated fashion to avoid cutting off too much nerve.
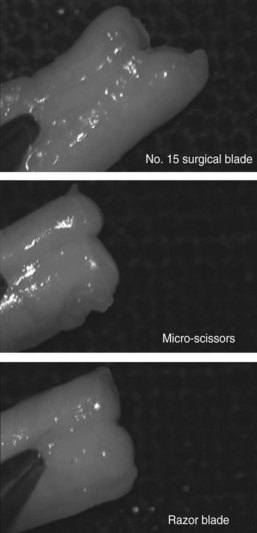
It is important to use a sharp micro-scissors reserved for this purpose. The use of a blunt scissors can lead to a crushed cut with unevenly cut fascicles. A fresh no. 15 blade can also be used for this purpose, provided that the nerve can be placed on a firm, nonslippery surface. We have found that a sterile razor blade and a gauze-wrapped wooden spatula are ideal in preparing the ends of the divided nerve as well as the nerve graft (Fig. 16-10).
Step 2: Assessment of Nerve Gap and Possibility of Primary Repair
 The gap between the nerve ends is measured with the IP joint and metacarpophalangeal (MCP) joint in full extension.
The gap between the nerve ends is measured with the IP joint and metacarpophalangeal (MCP) joint in full extension.
 One should proceed with nerve grafting if the gap is greater than 10 mm. Additional mobilization and slight flexion of the IP joint will allow tension-free repair of gaps smaller than 5 mm. For gaps that are 5- to 10-mm wide, a single 8-0 nylon suture can be used to assess tension of the repair with the joint in 30-degree flexion. If the suture can hold the nerve ends together, a primary repair is attempted.
One should proceed with nerve grafting if the gap is greater than 10 mm. Additional mobilization and slight flexion of the IP joint will allow tension-free repair of gaps smaller than 5 mm. For gaps that are 5- to 10-mm wide, a single 8-0 nylon suture can be used to assess tension of the repair with the joint in 30-degree flexion. If the suture can hold the nerve ends together, a primary repair is attempted.
Step 2 Pearls
In a patient with an associated tendon injury, it is preferable to graft a nerve defect rather than suture it, even under slight tension, because the nerve repair is likely to rupture during early mobilization for the tendon injury.
In a traumatic situation with skin loss associated with segmental loss of a digital artery and nerve (up to 10 mm), it may be possible to use a homodigital neurovascular island flap based on the proximal end of divided artery and nerve. This flap can be advanced 10 mm, allowing closure of the skin as well as primary repairs of the digital nerve and artery.
Step 3: Selection of Nerve Graft
 A nerve graft should be 10% to 15% longer than the measured gap to account for shrinking of the graft as a result of elastic recoil.
A nerve graft should be 10% to 15% longer than the measured gap to account for shrinking of the graft as a result of elastic recoil.
 The selection of nerve autografts for digital nerve defects depends on the number, length, and location of the nerve gap.
The selection of nerve autografts for digital nerve defects depends on the number, length, and location of the nerve gap.
Step 3 Pearls
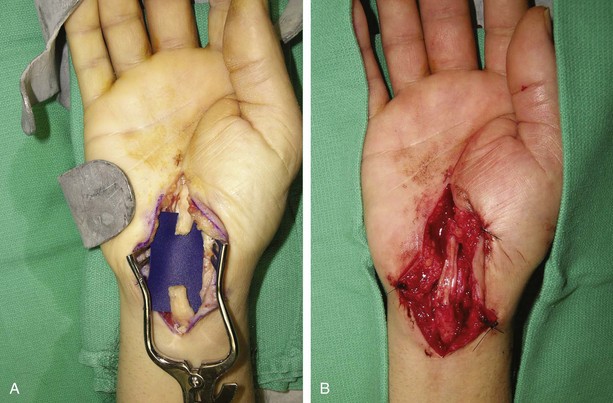
We prefer to use a conduit (vein conduit/PGA conduit) for a digital nerve gap that is less than 3 cm (Fig. 16-11).
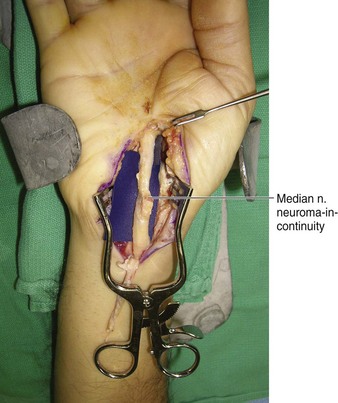
For digital nerve gaps that are 3 cm or larger, we use a nerve autograft (Figs. 16-12 and 16-13).
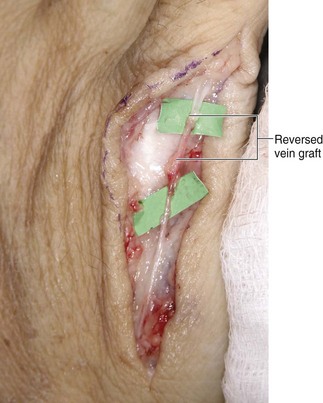
We use a vein graft for nondigital nerve defects (dorsal cutaneous nerves and superficial radial nerve) because the vein grafts are available locally and an additional incision is not usually required (Fig. 16-14).
We also prefer the use of vein conduit in elderly patients (>65 years) because the results of nerve grafting are poor in this population. The use of vein conduit minimizes the risk for neuroma formation and avoids the morbidity associated with harvest of nerve grafts.
Step 4: Harvest of Nerve Graft
 An appropriate length of nerve graft is harvested from the selected site.
An appropriate length of nerve graft is harvested from the selected site.
 The tourniquet is released and hemostasis secured at the nerve graft donor site and the recipient site.
The tourniquet is released and hemostasis secured at the nerve graft donor site and the recipient site.
Step 4 Pearls
The nerve graft should be handled with care using fine-tipped micro-instruments.
The graft should be 10% to 15% longer than the measured defect.
It is important to mark any one end of the nerve graft (proximal or distal). We feel that it is better to reverse the nerve graft when bridging the defect. This may prevent outgrowth of axons from the branches.
If a vein conduit is being used, it should also be reversed so that the valves do not obstruct axonal growth.
Postoperative Care and Expected Outcomes
 The patient is started on early mobilization within the splint. There should be no tension at the repair site in a nerve graft, and patients can be mobilized early, as opposed to after a primary repair, which would require a longer period of immobilization. The splint can be discontinued after 2 to 3 weeks, and patients are advised to avoid hyperextension for another 2 to 3 weeks.
The patient is started on early mobilization within the splint. There should be no tension at the repair site in a nerve graft, and patients can be mobilized early, as opposed to after a primary repair, which would require a longer period of immobilization. The splint can be discontinued after 2 to 3 weeks, and patients are advised to avoid hyperextension for another 2 to 3 weeks.
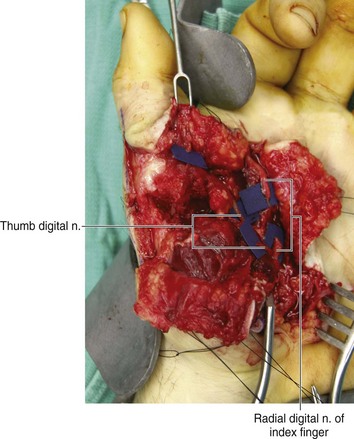
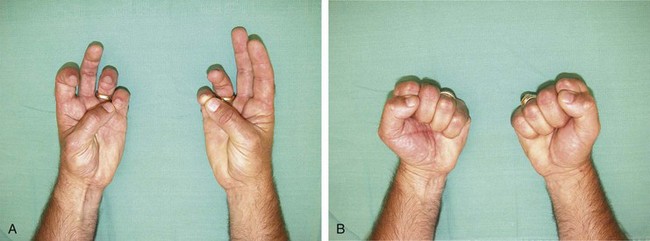
 More than 90% of patients (<65 years) get S3 or greater sensory recovery after a nerve graft (Fig. 16-15—late postoperative result of patient in Figs. 16-1 and 16-12). This equates to recovery of pain and touch sensation, disappearance of hyperesthesia, and ability to localize stimulus. However, there is imperfect recovery of two-point discrimination.
More than 90% of patients (<65 years) get S3 or greater sensory recovery after a nerve graft (Fig. 16-15—late postoperative result of patient in Figs. 16-1 and 16-12). This equates to recovery of pain and touch sensation, disappearance of hyperesthesia, and ability to localize stimulus. However, there is imperfect recovery of two-point discrimination.
Higgins JP, Fisher S, Serletti JM, Orlando GS. Assessment of nerve graft donor sites used for reconstruction of traumatic digital nerve defects. J Hand Surg [Am]. 2002;27:286-292.
Rinker B, Liau JY. A prospective randomized study comparing woven polyglycolic acid and autogenous vein conduits for reconstruction of digital nerve gaps. J Hand Surg [Am]. 2011;36:775-781.