Central and Peripheral Nervous System Medications
Objectives
1. Explain the physiologic processes of the central and peripheral nervous systems.
2. Identify the major classes of drugs that affect the central nervous system (CNS).
3. List different actions of antimigraine products.
4. Explain the major actions of drugs used to treat disorders of the CNS.
5. Identify the role of psychotropic drugs in psychotherapeutic intervention.
6. Compare and contrast different categories of medications used to treat mood disorders.
Key Terms
acetylcholine (ăs-ě-tĭl-KŌ-lēn, p. 252)
adrenergic blocking agents (ăd-rěn-ĚRJ-ĭk, p. 253)
adrenergic fibers (ăd-rěn-ĚRJ-ĭk, p. 252)
anticholinergics (ăn-tĭ-kō-lĭn-ĚRJ-ĭks, p. 253)
autonomic (ŏ-tō-NŎM-ĭk, p. 252)
barbiturates (bär-BĬ-chŭ-rets, p. 259)
catecholamines (kăt-ě-KŌ-lă-mēnz, p. 253)
central nervous system (CNS) (SĔN-trŭl NŬR-vŭs SĬS-tĕm, p. 251)
cholinergic drugs (kō-lĭn-ĚRJ-ĭk, p. 253)
cholinergic fibers (kō-lĭn-ĚRJ-ĭk, p. 252)
hypnotic agent (hĭp-NŎT-ĭk, p. 293)
idiopathic (ĭd-ē-ō-PĂTH-ĭk, p. 257)
initial insomnia (ĭn-ĬSH-ăl ĭn-SŎM-nē-ă, p. 293)
intermittent insomnia (ĭn-těr-MĬT-ěntĭn-SŎM-nē-ă, p. 293)
neurotransmitters (nŭr-ō-TRĂNS-mĭt-ěrz, p. 252)
norepinephrine (NŎR-ěp-ĭn-ĚF-rěn, p. 252)
Parkinson disease (PĂR-kĭn-sĕnz dĭ-ZĒZ, p. 267)
parasympathetic (p. 252)
peripheral nervous system (PNS) (pě-RĬF-ěr-ă l, p. 252)
receptor (rē-SĚP-tŏr, p. 253)
sedative agent (SĚD-ă -tĭv, p. 293)
seizures (SĒ-zhŭ rz, p. 257)
somatic (sō-MĂT-ĭc, p. 252)
status epilepticus (STĂT-ŭsě p-ĭ-LĚP-tĭ-kŭ s, p. 260)
sympathetic (p. 252)
terminal insomnia (TŬR-mĭn-ăl ĭn-SŎM-nē-ă, p. 293)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
This chapter has six sections discussing drugs that act on various parts of the central nervous system (CNS) and the peripheral nervous system (PNS). Although many drugs are used in treating CNS diseases, the principles of drug usage, actions of the medications, and adverse reactions are very similar. The nurse will benefit from learning how these drugs are the same and how they are different for the various categories of drugs. Although narcotic and nonnarcotic analgesics are also CNS drugs, they will be discussed in Chapter 17.
The first section of this chapter explores antimigraine agents. The second section covers the medications used to treat various types of seizures. The third section discusses drugs for vertigo (feeling of dizziness or spinning), and the fourth section presents drugs used to treat Parkinson disease. The fifth section introduces all the psychotropic drugs and includes subsections dealing specifically with medications used to treat anxiety, depression, and psychosis. Lithium, a unique antimanic medication, is covered in this section. The sixth section discusses sedative-hypnotics and their use in anxiety and sleep disorders.
Nervous System
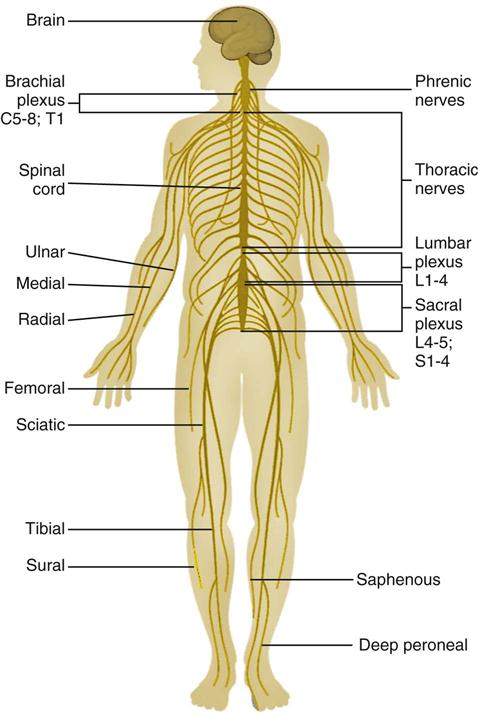
The major structures of the nervous system include the brain, spinal cord, nerves, and sensory receptors (Figure 16-1). The nervous system regulates and coordinates the body’s activities (including the senses), controls movement, and coordinates physiologic and intellectual functions.
The nervous system has two divisions, the central and the peripheral. The central nervous system (CNS), made up of the brain and the spinal cord, is located within the cranial cavity of the skull and the vertebral canal of the spinal column. The peripheral nervous system (PNS) includes all nervous structures (ganglia and nerves) that lie outside the cranial cavity and the vertebral canal. These include the cranial and spinal nerves and the sympathetic division of the autonomic nervous system.
Pathologic conditions in the brain may produce either local or general symptoms; abnormalities in the peripheral system usually cause only local symptoms. Because the nerve and muscle systems are mixed together so closely, it is often difficult to tell if disease lies within the nerves or the structures activated by the nerves.
Although the drugs covered in this chapter focus on the actions of the CNS, or those actions controlled by the brain and spinal cord, many of these agents act through the PNS. The PNS produces changes or activity in the body through the nerves and chemicals of the motor nervous system and the autonomic nervous system as they carry out directions from the CNS.
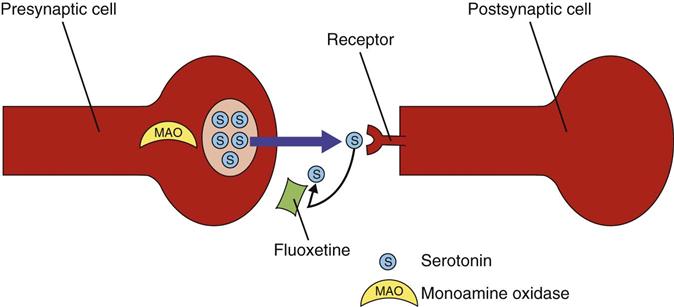
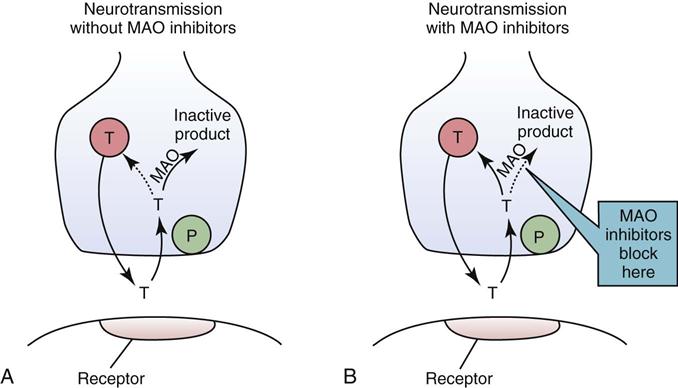
Drugs act on the CNS and peripheral nerves by sending or transmitting information from the brain through chemical messengers or neurotransmitters. The neurotransmitter chemical is released at the end of one neuron and passes across a small gap (the synapse) to activate the next neuron in the chain. At the end of the nerve chain, it stimulates an organ, smooth muscle, or gland to produce a physiologic response.
In the PNS, nerves of the somatic nervous system have voluntary control over skeletal muscle. Nerves of the autonomic nervous system provide involuntary control over organs and tissues of the heart muscles, and over smooth muscles and glands affecting the salivary glands and digestive tract, eyes, respiratory tract, and reproductive tracts. The action of the autonomic nervous system is very important to understanding the action of key drugs that act on this system.
The autonomic system works through two subdivisions—the sympathetic nervous system and the parasympathetic nervous system. These two systems work together in directing how most organs and glands work. The sympathetic system helps the body prepare for stressful situations by producing chemicals that will induce the “fight or flight” response. The parasympathetic nervous system provides the basic, routine maintenance of the body actions and has been called the “rest-and-digest response”.
The nervous system is made up of small cells called neurons. The cells might be thought of as people standing in line passing a message to each other to do something. Instead of one person telling the next person the message, in the nervous system, a neurotransmitter chemical is released by the neuron which crosses the space or synapse between the two messengers (neurons) and is received by the receptor neuron on the other side. Then that neuron messenger turns to the next neuron cell to send the message forward until the final message is received, perhaps to affect skeletal muscle that will move the hand.
There are a variety of neuron transmitters that carry these messages. The two major neurotransmitters in the body are norepinephrine, which acts on the sympathetic nerves, and acetylcholine, which acts on the parasympathetic nerves. There are several other important neurotransmitters, especially in the brain. Nerve fibers that release norepinephrine are called adrenergic fibers. Nerve fibers that release acetylcholine are called cholinergic fibers. Most organs in the body are influenced by both types of fibers, which have opposite effects. For example, adrenergic activity speeds up the heart rate, and cholinergic activity slows it down. It is possible to compare this system to a car that is influenced by an accelerator and a brake. It is very important to understand these concepts because many drugs look or act like neurotransmitters and they act to help or block the action of neurotransmitters.
There are several names for the types of drugs that act on the nervous system. Because autonomic drugs either block or stimulate either the sympathetic or parasympathetic nervous systems, these autonomic drugs are classified based on their actions. These drugs have been called by several different names as, over time, research reveals more information about them.
These basic terms are used throughout this chapter. Remembering these terms and definitions will help in understanding drug actions.
When neurotransmitters release their chemicals, the chemicals are targeted to act at certain parts of the body. Each neurotransmitter has a certain chemical shape (like a key), which produces an action only when it “fits into” a specific receptor (lock) for that chemical.
Acetylcholine (cholinergic) receptors are classified as either muscarinic (which stimulate smooth muscle and gland secretions and decrease the heart rate and force of heart contraction) or nicotinic (which stimulate smooth muscle and gland secretions). Norepinephrine (adrenergic) receptors are identified as alpha 1 (provides for constriction of blood vessels and dilation of pupils); alpha 2 (blocks norepinephrine release); beta 1 (increases heart rate and force of contraction and release of renin); and beta 2 (blocks smooth muscle action). Note that when stimulated, alpha receptors often have the opposite effect of beta receptors on the heart, blood vessels, GI tract, or eye muscles. The text often refers to a medication as having alpha or beta properties. For example, some medications are called beta blockers because of their selective action in blocking only the beta-adrenergic effects in the body.
Many of the drugs discussed in the following sections act on more than one type of receptor. Each agent acts differently, making it possible for certain drugs to be given for specific actions without many adverse reactions. It should be clear that if dosages are exceeded, many receptors may be overly stimulated, causing widespread and serious effects. Thus accuracy in giving the right amount of drug and at the proper time is very important in giving these drugs safely.
Sympathomimetic Drugs
Adrenergic agonists or sympathomimetic drugs produce chemicals involved in the fight-or-flight syndrome and have many of the same effects as the anticholinergics. Some of the drugs have been developed so that they act specifically on either the alpha or beta subreceptors. This makes their actions more focused and predictable.
The effects of these drugs depend on which adrenergic subreceptors are stimulated. Some act very selectively, for example, on drying secretions in the nose. Other drugs act primarily on the heart or to help bronchodilation in the lungs. Thus these drugs may have specific uses prior to surgery, with specific heart problems, or asthma. Other drugs may stimulate more than one type of adrenergic receptor and so are considered nonselective. Thus product information may say that drugs act on both beta 1 and beta 2 receptors or both alpha 1 and beta 2 receptors. This should help the nurse anticipate what these drug actions might be.
Because of the variability in drug actions, many of these drugs are discussed in other relevant chapters in the book. Only a few of the most common sympathomimetics are listed in Table 16-1, along with their receptors.
![]() Table 16-1
Table 16-1
Selected Sympathomimetics and Adrenergic Drugs
| DRUG | TRADE NAME | RECEPTOR SUBTYPES | USE |
| Sympathomimetics | |||
| Albuterol | Proventil, Ventolin | Beta 2 | Asthma treatment |
| dobutamine | Dobutrex | Beta 1 | Heart stimulant |
| dopamine | Intropin | Alpha 1 and beta 1 | Treatment of shock |
| epinephrine |
Adrenalin, Primatene | Alpha and beta | Comes in variety of forms to treat asthma, shock, cardiac arrest |
| isoproterenol | Isuprel | Beta 1 and beta 2 | Comes in variety of forms to treat heart failure, asthma, dysrhythmias |
| metaproterenol | Alupent | Beta 2 | Used to treat asthma attacks and maintenance |
| metaraminol | Aramine | Alpha 1 and beta 1 | Used to treat shock |
| norepinephrine | Levarterenol, Levophed | Alpha 1 and beta 1 | Used to treat shock |
| oxymetazoline | Afrin | Alpha | Topical OTC product to treat nasal congestion |
| phenylephrine | Neo-Synephrine | Alpha | Topical OTC product to treat nasal congestion |
| pseudoephedrine | Sudafed | Alpha and beta | Topical OTC product to treat nasal congestion |
| ritodrine | Yutopar | Beta 2 | Slow uterine contractions and reduce risk of abortion |
| salmeterol | Serevent | Beta 2 | Used to treat nasal congestion and asthma |
| terbutaline | Brethine | Beta 2 | Used to treat asthma |
| Adrenergic Blockers | |||
| acebutolol | Sectral | Beta 1 | Used for treating dysrhythmias, angina, hypertension |
| atenolol | Tenormin | Beta 1 | Used for treating hypertension and angina |
| carteolol | Cartrol | Beta 1 and beta 2 | Used in treatment of glaucoma and hypertension |
| carvedilol | Coreg | Alpha 1, beta 1, and beta 2 | Used in treating hypertension |
| doxazosin | Cardura | Apha 1 | Used in treating hypertension |
| esmolol | Brevibloc | Beta 1 | Used in treating hypertension |
| metoprolol | Lopressor | Beta 1 | Hypertension, heart failure, MI |
| nadolol | Corgard | Beta 1 and beta 2 | Used in treating hypertension |
| phentolamine | Regitine | Alpha | Used in severe hypertension |
| prazosin | Minipress | Alpha 1 | Used in treating hypertension |
| propranolol |
Inderal | Beta 1 and beta2 | Used in dysrhythmias, angina, hypertension, treatment of migraines |
| sotalol | Betapace | Beta 1 and beta 2 | Used in dysrhythmias |
| terazosin | Hytrin | Alpha 1 | Used in treating hypertension |
| timolol | Blocadren, Timoptic | Beta 1 and beta 2 | Used in treating angina, hypertension, glaucoma |
MI, Myocardial infarction; OTC, over the counter.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Adrenergic Agonists or Blockers
The actions of the sympathetic nervous system are blocked by adrenergic blocker medications. These agents are common and are used in the treatment of hypertension. The actions of adrenergic blockers are quite specific and this makes them very useful. They are used primarily in blocking the effect on beta 1 receptors only present in the heart, or blocking receptors in vascular smooth muscle in small arteries, causing vasodilation and reducing blood pressure. Other beta blockers are nonselective so they block both beta 1 and beta 2 receptors. These drugs usually have more side effects. A list of these drugs and their primary receptor subtype is in Table 16-1. A more complete discussion of these drugs and their uses in hypertension is found in Chapter 15.
Parasympathetic Drugs
Parasympathomimetic drugs that produce the rest-and-digest responses act like the parasympathetic chemicals in the body. The action of these drugs is difficult to limit to a small part of the body and they have many adverse effects. Thus there are only a small number of these drugs and they are used carefully for specific neurologic problems. For example, bethanechol (Urecholine) is a direct-acting agonist and neostigmine (Prostigmin) is a reversible cholinesterase inhibitor. Both are used to help contract the muscles in the ureters or bladder when treating for urinary retention. Physostigmine (Antilirium) and pilocarpine (Isopto Carpine) are commonly used to treat glaucoma by reducing intraocular pressure. Pyridostigmine (Mestinon) is a drug used only for the treatment of myasthenia gravis, a relatively uncommon neurologic problem.
Anticholinergic Drugs
Anticholinergic drugs mimic the fight-or-flight response. These drugs are commonly used for their autonomic function in the treatment of many respiratory and GI disorders. The drugs increase heart rate, dilate pupils, dry secretions, and dilate the bronchi of the respiratory tract. The usefulness of these drugs is limited because of their adverse effects—primarily producing a rapid heart rate and causing urine release to be blocked in older men who have enlarged prostate glands. Some of the newer medications have fewer side effects than older drugs in this category.
Examples of common anticholinergics are atropine and glycopyrrolate (Robinul) that are used prior to anesthesia to dry up secretions, to increase heart rate in some arrhythmias, and dilate the pupils in assessment of some eye problems. Glycopyrrolate also has been used in the treatment of peptic ulcers and irritable bowel syndrome, along with Propantheline (Pro-Banthine) and dicyclomine (Bentyl). Cyclopentolate (Cyclogyl) is also used to dilate pupils. Ipratropium (Atrovent) is used in treating asthma, oxybutynin (Ditropan) is used in treating urinary bladder urgency and incontinence, and scopolamine (Hyoscine, Transderm-Scop) is used not only for treating irritable bowel syndrome, but also has a central effect in controlling motion sickness and alcohol withdrawal symptoms. Many of these drugs have significant interactions when given with other medications. The more important of these medications will be discussed as relevant drugs in other chapters.
Antimigraine Agents
Overview
Headaches are a common problem seen in primary care patients. Tension headaches that occurs when stress causes the muscles of the head and neck to tighten are successfully treated with over-the-counter (OTC) drugs such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), or aspirin.
Migraine headaches are more serious and complex headaches in which the patient feels throbbing or pulsating pain, often made worse by noise or bright light. These headaches are often triggered by specific products (like monosodium glutamate in some foods), food additives, chocolate, red wine, and caffeine. A warning sign or aura that a migraine headache is developing might occur when the patient has changes in vision, hearing, taste, or smell. These headaches might also produce nausea, vomiting, and severe fatigue. These migraine headaches are treated with a variety of different drugs and may also be prevented by some types of medicines (prophylactic medicine).
Antimigraine agents block nerve impulses in the receptors of the sympathetic nervous system and so may be used for either prevention or treatment. The ergot alkaloids used in the treatment of vascular headaches are adrenergic-blocking agents. Treatment medications should be given as soon as the pain begins. Other medications can be taken to prevent migraines from occurring (prophylactically).
Action
There are two commonly used classes of drugs used in migraine treatment: (1) ergot alkaloids; and (2) triptans. Both of these drug classes stimulate serotonin (5-hydroxytryptamine [5-HT]) and affect the many serotonin receptor subtypes found throughout the CNS. There are a variety of other anticonvulsant, antidepressant, beta-adrenergic blockers, or calcium channel blockers that may be used to treat severe migraines. Riboflavin (Vitamin B2) and feverfew are alternative therapies some have found to be effective.
The process that produces migraine headaches is thought to be local dilation of the blood vessels in the cranium or the release of sensory neuropeptides through nerve endings in the trigeminal system. The vascular 5-HT receptor is present on the human basilar artery and in the vessels of human dura mater. Use of the 5-HT, or serotonin, receptor antagonists results in cranial vessel constriction (narrowing) and blocking of neuropeptides that cause inflammation, which happens at the same time the patient feels the relief from migraine headache. Some of these products also cross the blood-brain barrier, produce central activity on the trigeminovascular system, and stop nerve depolarization at peripheral sites in the cranium.
Additionally, adrenergic-blocking agents dilate the veins in smooth muscle tissue in the peripheral vascular system, reducing cerebral blood flow and arterial pulsing, which reduces headache pain. Other actions include dilation of veins in the uterus, an increase in uterine contractions (oxytocic effect), and a decrease in blood pressure.
Uses
Antimigraine agents are used in both the prevention and treatment of vascular headaches. They relieve the pain of vascular headaches by narrowing dilated cerebral arteries. OTC drugs such as ibuprofen or aspirin are usually started first. If these drugs are not helpful, triptans such as sumatriptan (Imitrex) are used. The triptans come in a variety of forms, including injection and inhalation, so that if the patient has nausea or vomiting, he or she may still take the drug. The action of 5-HT agonists is not affected by whether or not the person with the migraine has an aura or by the length of the attack, sex or age of the patient, relationship to menstrual periods, or the use of other common migraine prevention drugs. Ergot alkaloids like ergotamine (Ergonal) are used if triptans are not effective, although less commonly. Ergot alkaloids are also used for pregnant women for oxytocic (labor-inducing) and other smooth-muscle spasmogenic effects. They are not used in early pregnancy as they are pregnancy category X drugs.
Adverse Reactions
Adverse reactions to antimigraine agents in general include heart murmurs, brief tachycardia (rapid heartbeat), confusion, depression, dizziness, drowsiness, fixed miosis (constriction) of the pupil of the eye, paresthesias (numbness and tingling) in the toes, weakness (especially in legs), nausea and vomiting, leg cramps, localized pruritus (itching) and edema (fluid buildup in the body tissues), and neutropenia of the blood. Symptoms of overdosage include numb, cold, pale extremities; constant muscle pain, even at rest; decreased or absent arterial pulses; drowsiness; confusion; depression; convulsions; hemiplegia; and fixed miosis. Because of the potential for 5-HT agonists to cause coronary vasospasm, patients with ischemic heart disease or other major cardiovascular disease, or uncontrolled hypertension (high blood pressure) should not use these products.
Drug Interactions
When antimigraine agents are used with other vasoconstrictors, vasoconstriction may be increased. The 5-HT agonists may not be used within 24 hours of taking an ergotamine-containing preparation and may not be used at the same time with monoamine oxidase (MAO) inhibitor therapy, selective serotonin reuptake inhibitors (SSRIs) serotonin/norepinephrine reuptake inhibitors (SNRIs), lithium (given for depression), and many other drugs. Some of the different triptans cannot be used within 24 hours of each other because of drug interactions.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the overall health history of the patient, as well as the history of headaches (whether tension, migraine, or cluster). Find out whether there are factors that might affect the patient’s use of antimigraine drugs (e.g., coronary artery disease or conditions in which a sudden change in blood pressure may be dangerous).
The patient may have a history of migraine headaches, vascular headaches, or headache pain of a periodic, throbbing, severe nature. The pain may be one-sided (unilateral) and commonly felt over one eye. Photophobia (sensitivity to light) and sensitivity to sound may be present, as well as nausea and vomiting. A family history of vascular headaches or history of motion sickness as a child, series of headaches in clusters, history of hypertension, a food allergy, or use of birth control pills may be present. The headache may have been relieved or eased by sleeping, vomiting, or drinking a caffeinated drink.
Ask whether the patient uses any herbal products or vitamins to control headache or migraines, because some of these products may interact adversely with other drugs, including nonsteroidal antiinflammatory drugs (NSAIDs). The Complementary and Alternative Therapies box summarizes herbal preparations the patient may be using and their drug interactions. The nurse may observe signs of sweaty hands and feet, scalp tenderness, autonomic dysfunction (such as miotic pupil), red eye, and unilateral nasal congestion.
n Diagnosis
In addition to the medical diagnosis, what other symptoms does this patient have that require nursing action? Are there needs for patient education, nutrition information, and quiet time away from people? Sometimes identifying the migraine triggers leads to the diagnosis of other emotional or physical problems.
n Planning
Ergot alkaloids increase uterine contraction and may be harmful to the pregnant patient. These migraine medications are slowly and incompletely absorbed from the GI tract. Traces of ergotamine remain in various tissues; this accounts for its long-lasting and toxic actions.
n Implementation
Patients who have had migraines often have a regimen they follow that helps bring relief. These behaviors often include isolating themselves in a dark, quiet room, use of icepacks on head, and avoiding food. If migraine agents are used at the onset of an attack, the ability of the drugs to relieve migraine pain and symptoms is increased. If the patient’s pain is relieved after an intramuscular (IM) injection of 1 mL (0.5 mg) of ergotamine, the diagnosis of vascular headaches is confirmed.
Antimigraine products are available in oral, sublingual, parenteral, and rectal forms, and as a solution for inhalation. Many factors, including whether the purpose of the agent is to prevent or to treat migraine, influence which form will be best tolerated and most effective.
Oral and rectal preparations are absorbed slowly and incompletely from the GI tract. To speed up this absorption, caffeine is included with oral and rectal preparations of ergot alkaloids. Persons who are vomiting and cannot tolerate oral preparations are given rectal forms of the agent. Inhalant methods are preferred by some patients. Sublingual tablets are more quickly absorbed than either rectal or oral preparations. IM and subcutaneous preparations are commonly used, but absorption is often incomplete and slow.
A list of important dosage information about antimigraine products is presented in Table 16-2.
![]() Table 16-2
Table 16-2
| GENERIC NAME | TRADE NAME | COMMENTS |
| Serotonin (5-HT) Receptor Agonists | ||
| almotriptan | Axert | For acute treatment of migraine and prevention. |
| eletriptan | Relpax | Used for acute treatment, as well as prophylaxis. Older adults may be particularly sensitive and have hypotension. May cause angina or MI. |
| frovatriptan | Frova | Used for acute treatment, as well as prophylaxis. Produces tachycardia. |
| naratriptan | Amerge | Single doses taken with fluid are typically effective in relieving acute pain. If headache returns or patient has only partial response, dose may be repeated in 4 hr. Higher doses do not produce better results. |
| rizatriptan benzoate | Maxalt | Comes as a tablet or an orally disintegrating tablet that does not require liquid but must not be opened until just before dosing. |
| sumatriptan succinate |
Imitrex | Comes PO, SC injection, or intranasal spray. |
| zolmitriptan | Zomig | Break tablet in half for initial dose. Repeat in 2 hr if headache returns. Use care in patients with liver dysfunction. Also comes as nasal spray. |
| Ergotamine Derivatives | ||
| dihydroergotamine |
DHE 45 | An alpha-adrenergic blocking agent with pharmacologic and toxic properties similar to ergotamine used to treat migraine headaches. The drug causes cerebral vasculature to constrict, but it does not have an oxytocic effect and can be used during pregnancy. |
| Migranal | ||
| ergotamine | Ergomar | An alpha-adrenergic blocking agent that exerts direct vasoconstriction on cranial blood vessels, relieving pulsations thought to be responsible for vasoconstriction. Dependence on ergotamine may develop, necessitating gradual withdrawal from this product. |
| Combination products | Cafergot | Cafergot is a combination of ergotamine, caffeine, and other products used to treat migraine and vascular headaches. Caffeine is included in these products to increase absorption of ergot alkaloids. Small amounts of belladonna alkaloids and barbiturates may also be included to control nausea and produce sedation. Comes PO or suppository. |
| Other Migraine Prophylaxis Products | ||
| Beta-Adrenergic Blockers | ||
| atenolol | Tenormin | Also used in treatment angina and hypertension. |
| metoprolol | Lopressor | Also used in treatment angina and hypertension. Comes in sustained-release and IV forms. |
| propranolol HCl | Inderal | Also used in treating cardiac dysrhythmias. |
| timolol | Blocadren | Also used for treatment glaucoma, angina, and hypertension. |
| Calcium Channel Blockers | ||
| nifedipine | Procardia | Also used for treatment of angina and hypertension. Available in sustained-action product. |
| nimodipine | Nimotop | Used following strokes to improve neurologic statue; unlabeled use in preventing migraines. |
| verapamil HCl | Calan | Unlabeled use in preventing migraines. |
| Tricyclic Antidepressants | ||
| amitriptyline | Elavil | Unlabeled use in preventing migraines. |
| imipramine | Tofranil | Also used to control bedwetting in children and alcohol or cocaine dependence. Many side effects. |
| Miscellaneous Agents | ||
| valproic acid | Depakote | Also used for absence or mixed generalized seizures and mania. |
| methysergide | Sansert | Similar to ergotamine. |
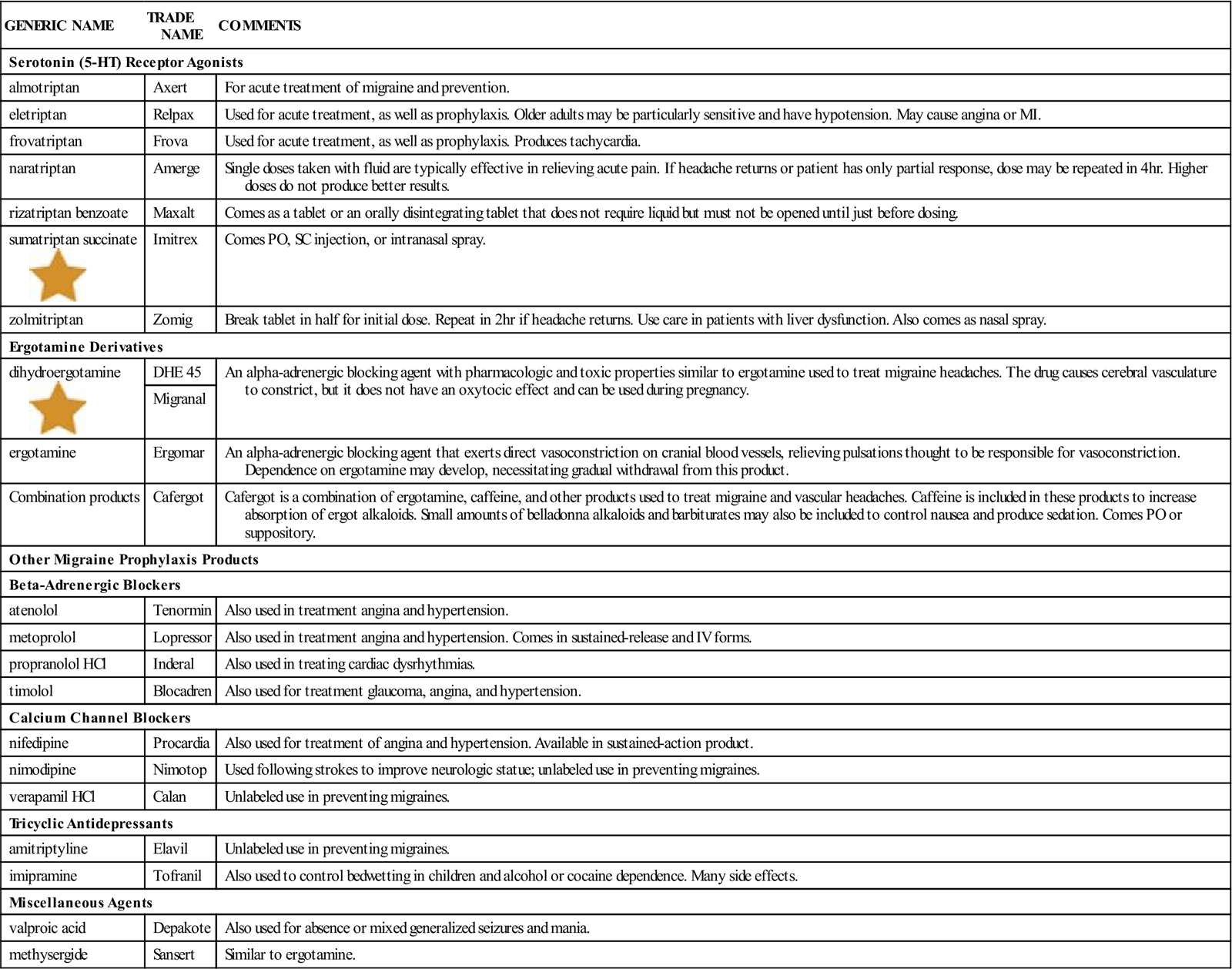
5-HT, 5-Hydroxytriptamine; IV, intravenous; MI, myocardial infarction; PO, by mouth; SC, subcutaneous.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
When evaluating the patient with recurrent migraines, determine if the drug is helping. There should be a decrease in number and severity of migraine headaches. To determine if overdosage, toxicity, or adverse reactions are developing, monitor the patient’s blood pressure in standing, sitting, and lying positions and check for peripheral pulses.
Long-term use of migraine agents can lead to acute overdosage or chronic toxicity because of the wide variability in their absorption, metabolism, and excretion. Because patients often treat themselves, they may not realize that they are overdosing.
Abruptly stopping any of the agents used to treat migraines after long-term use can result in rebound (or new-onset) migraine headaches; therefore, they should be stopped very slowly.
n Patient and Family Teaching
Anticonvulsants or Antiepileptic Drugs
Overview
Seizures are sudden muscle contractions that happen without conscious control. They are a symptom of abnormal and excessive electrical discharge in the brain. A variety of diseases and disorders can produce seizures. High temperatures in infants and children may provoke seizures. One of the most common causes of chronic and recurring seizures is epilepsy, which is frequently of an unknown cause (idiopathic). Head injury, brain tumor, stroke, meningitis, temperature elevation, and poisoning, especially from excessive alcohol intake or drugs, are also common causes of seizure activity. The most frequent cause of a seizure is the failure to take medication to control previously diagnosed seizure activity. It is estimated that as many as 10% of all people will have a seizure during their lifetime, although this percentage may rise as more people abuse drugs. The diagnosis of epilepsy often has legal consequences, which vary among states, including restriction of driver’s licenses and restriction from operation of heavy machinery or doing other activities that require alertness. It is obvious how it might be a problem if someone were driving a car or big truck and suddenly had a seizure.
The terms epilepsy, convulsions, and seizures are commonly used to mean the same thing, although they each have a slightly different medical meaning. A variety of terms have been used over the years to describe types of seizures, including grand mal (tonic-clonic), petit mal (absence), psychomotor, myoclonic, atonic, and jacksonian. More recently, there has been agreement to group seizures into two broad categories, generalized or focal, based on their clinical presentation and electroencephalographic (EEG) patterns. This chapter uses both terms.
Sometimes surgery or dietary treatment may be used to control symptoms in a patient with a seizure disorder. More commonly, epileptic seizures are treated with medication. The goal of this type of therapy is to suppress or reduce the number of patient seizures.
Action
A number of drugs control seizures through depression or slowing of abnormal electrical discharges in the CNS. These products work in a variety of ways. There is usually one drug that is more effective than another for a patient, depending on the type of seizure activity. Patients with newly diagnosed and acute seizure disorders are often started on parenteral injection therapy; when seizure activity has come under control, oral therapy is started.
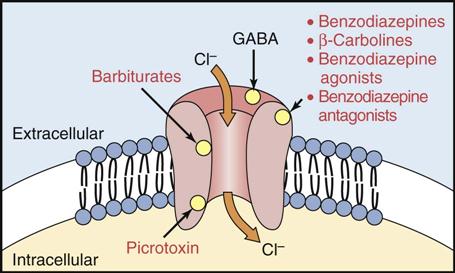
There are five major anticonvulsant or antiepileptic drug (AED) groups: barbiturates, benzodiazepines, hydantoins, succinimides, and γ-aminobutyric acid (GABA) analogues (Figure 16-2). A list of anticonvulsants and their uses is presented in Table 16-3. In addition to prescription medications, patients and families sometimes try a variety of supplements and herbal products to treat seizure disorders. The Complementary and Alternative Therapies box provides a list of common herbal products and drug interactions important for patients to know.
![]() Table 16-3
Table 16-3
Antiepileptics and their Primary Uses
| GENERIC NAME | TRADE NAME | COMMENTS |
| Barbiturates | ||
| amobarbital | Amytal | Status epilepticus, acute convulsive episodes; also used for preoperative sedation and insomnia, preoperative anxiety and sedation |
| pentobarbital | Nembutal | General seizure, reduce ICP in head trauma; preoperative sedation, insomnia |
| phenobarbital |
Phenobarbital | All forms of epilepsy, status epilepticus, severe recurrent seizures, eclampsia |
| secobarbital | Seconal | Preoperative sedation; insomnia |
| Benzodiazepines | ||
| clonazepam | Klonopin | Petit mal, myoclonic seizures |
| clorazepate | Tranxene | Focal seizures |
| diazepam |
Valium | All forms of epilepsy, status epilepticus, severe recurrent seizures, tetanus |
| lorazepam | Ativan | Used for all seizures except febrile seizures |
| Hydantoins | ||
| fosphenytoin | Cerebyx | Status epilepticus |
| phenytoin | Dilantin | Used for partial seizures, status epilepticus |
| Phenytek | ||
| Succinimides | ||
| ethosuximide | Zarontin | Absence atonic seizures and myoclonic seizures |
| methsuximide | Celontin | Absence seizures; adjunct therapy in mixed seizures |
| phensuximide | Milontin | Absence seizures |
| GABA Analogs | ||
| tiagabine | Gabatril | Inhibits uptake of GABA into presynaptic neurons, prolonging GABA action; used for adjunctive therapy in adult partial seizures |
| Other Drugs | ||
| acetazolamide | Diamox | Absence seizures, metabolic alkalosis in mechanically ventilated patients, altitude sickness |
| carbamazepine | Tegretol | Status epilepticus, partial seizures |
| gabapentin | Neurontin | Partial seizures in adults, children |
| lamotrigine | Lamictal | Partial seizures in adults, children |
| levetiracetam | Keppra | Partial seizures in adults, children |
| oxcarbazepine | Trileptal | Partial seizures in adults, children |
| primidone | Mysoline | Grand mal, psychomotor, focal seizures in adults and children |
| topiramate | Topamax | Adjunctive therapy for partial-onset seizures in adults, children |
| valproic acid | Depakene | Used for all types of seizures |
| Depakote | ||
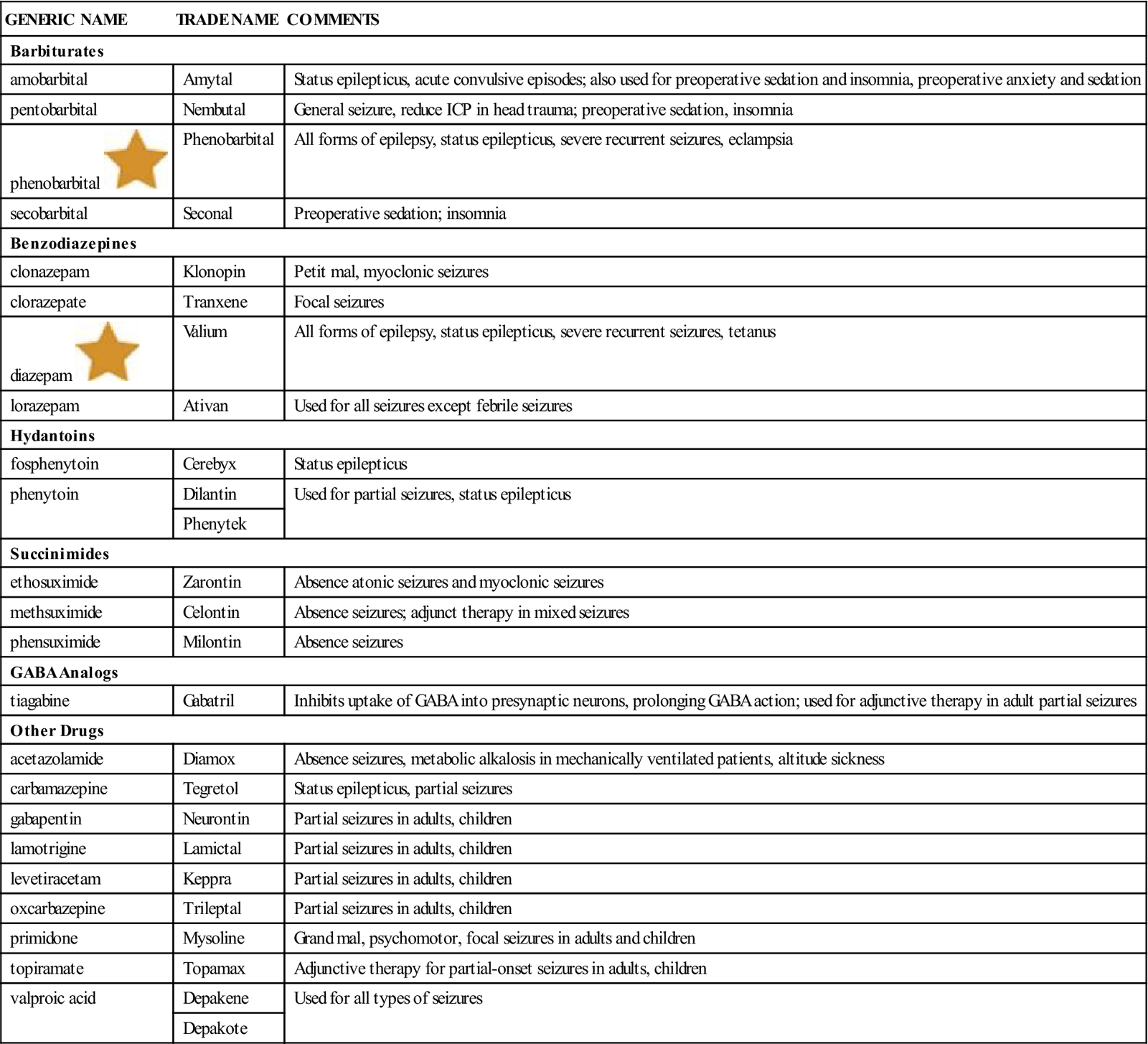
GABA, γ-Aminobutyric acid.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Uses
Barbiturates, which have a long duration of action, are an important category of prescription anticonvulsants and are used for their sedative effect on the brain. They may be used in combination with medications from the other three groups. Benzodiazepines are useful with some problems but also have a lot of serious adverse effects. Hydantoins have a wide range of uses, and phenytoin (Dilantin) is by far the most commonly used anticonvulsant. Succinimides are used to control petit mal seizures. GABA analogs have wide use for many types of seizures. Each of these five groups, along with a variety of other newer miscellaneous anticonvulsants, are discussed in this section.
Because of the variety of drugs and the many possible side effects, the choice of an anticonvulsant tends to be a trial or experiment for each patient. When seizures are not stopped with one drug, another may be added, or the first drug may be stopped and another product used instead.
Barbiturates
Action
Barbiturates are CNS depressants. They act primarily on the brainstem reticular formation, reducing nerve impulses that go to the cerebral cortex. Barbiturates depress the respiratory system and slow the activity of nerves and muscles (smooth, skeletal, and cardiac). Barbiturates also raise the seizure threshold, or the level of electrical activity that must be produced before a seizure will occur. Barbiturates may be short-acting, intermediate-acting, or long-acting.
Uses
Long-acting barbiturates are used as anticonvulsants to control and prevent grand mal seizures. They are sometimes used if other drugs do not help to treat status epilepticus, a condition in which a series of severe grand mal seizures occur one after another without stopping. They may also be used to treat seizures caused by tetanus, fever, or drugs.
Adverse Reactions
Adverse reactions to barbiturates include worsening of symptoms of certain organic brain disorders in older adult patients, dizziness, drowsiness, hangover, headache, lethargy (sleepiness), paradoxical restlessness or excitement, unsteadiness, photosensitivity (abnormal response to exposure to sunlight), rash, diarrhea, nausea, hepatitis with jaundice, vomiting, anemia, decreased platelet counts, unusual bleeding or bruising, urticaria (hives), joint and muscle pains, tolerance (increased resistance to the drug caused by repeated use), and withdrawal symptoms due to physical dependence when discontinued.
In cases of acute overdose, the patient may show exaggerated CNS depression, slow, shallow respirations, miosis, tachycardia, areflexia (absence of reflexes), shock, or coma. Death may occur as a result of cardiorespiratory failure.
Drug Interactions
Because barbiturates act through the P450 enzyme system to speed up the metabolism of some drugs in the liver, they reduce the activity of anticoagulants, corticosteroids, and digitalis preparations. MAO inhibitors may increase the depressant effects of the barbiturates. There may be significant additive effects if barbiturates are used along with alcohol, antihistamines, benzodiazepines, methotrimeprazine, narcotics, and tranquilizers.
Benzodiazepines
Action
Benzodiazepines are CNS depressants. Their exact mechanism of action is not known, but they are thought to act on the hypothalamus and limbic system of the brain, decreasing the vasopressor response and increasing the arousal threshold. Benzodiazepines suppress the electrical spike-and-wave brain discharge in seizures and decrease the frequency, amplitude, duration, and spread of the discharge in minor motor seizures.
Uses
Benzodiazepines are used to treat partial seizures and also to treat Lennox-Gastaut syndrome (petit mal variance) and for patients who have failed to respond to succinimide drugs such as ethosuccinimide (Zarontin). Three benzodiazepines are approved for use as anticonvulsants. Diazepam (Valium) is used intravenously to control seizures and is the drug of choice for treatment of status epilepticus. Clonazepam (Klonopin) is used for oral treatment of petit mal seizures in children, and clorazepate (Tranxene) is used with other antiepileptic agents to control partial seizures.
Adverse Reactions
Adverse reactions to benzodiazepines include hypotension (low blood pressure), shortness of breath, difficulty focusing or blurred vision, confusion, drowsiness, flushing (red color in the face and neck), headaches, light-headedness, paradoxical reactions (excitement, stimulation, hyperactivity), slurred speech, sweating, anorexia (lack of appetite), bitter taste, dry mouth, diarrhea, heartburn, nausea, vomiting, pruritus, rash, joint pains, and burning eyes.
Overdosage may produce marked drowsiness, weakness, impairment of stance and gait, confusion, and coma.
Drug Interactions
Alcohol, other sedatives and hypnotics, antidepressants, anticonvulsants, and narcotics may produce additive sedative effects if used with benzodiazepines. Some combinations of anticonvulsants may result in an antidepressant effect or provoke additional seizures.
Hydantoins
Action
Hydantoins act primarily on the motor cortex, where they stop the spread of seizure activity by blocking neuronal sodium and calcium channels. This stabilizes the nerve cell against hyperexcitability and reduces the maximal activity of brainstem centers responsible for the tonic phase of grand mal seizures. It also has an antiarrhythmic property.
Uses
Hydantoins are used to treat tonic-clonic and psychomotor seizures. Sometimes they are used to treat status epilepticus, migraine, and trigeminal neuralgia. They are also used in some nonepileptic psychotic patients.
Adverse Reactions
Adverse reactions to hydantoins include ataxia (poor coordination), dizziness, drowsiness, hallucinations, inattentiveness, nystagmus (rhythmic movement of the eyes), ocular disturbances, poor memory, slurred speech, constipation, nausea, vomiting, blood cell disturbances, purpura (bruising), acnelike eruptions, gingival hyperplasia (overgrowth of gums), lupus erythematosus, hepatitis with jaundice, and lymph node hyperplasia. Hydantoins are also teratogenic-category D (producing changes in the fetus). Overdosage may produce ataxia, coma, dysarthria, hypotension, nystagmus, and unresponsive pupils.
Drug Interactions
Hydantoin drug interactions are frequent and often substantial. Even when given alone, the drug requires careful monitoring of the patient. It is very important to see the patient regularly when it is used with any other medication or vitamins because the dose that prevents seizure is very close to the toxic dose. It may also alter the results of various laboratory tests.
Succinimides
Action
Succinimide-type anticonvulsants raise the seizure threshold in the cortex and basal ganglia, making seizures less likely and reduce response at the nerve synapse to some specific types of nerve stimulation.
Uses
Succinimides are used to control absence seizures.
Adverse Reactions
Adverse reactions to succinimides include dizziness, headaches, hiccups, hyperactivity, lethargy, mood or mental changes, rashes, blurred vision, photophobia (intolerance to light), anorexia, abdominal pain, diarrhea, nausea, vomiting, urinary frequency, vaginal bleeding, blood cell changes, alopecia (hair loss), muscular weakness, systemic lupus erythematosus, disturbances of sleep, inability to concentrate, mental slowness, and night terrors.
Drug Interactions
If these drugs are used with other anticonvulsants, they can result in increased sex drive (libido) or increased frequency of tonic-clonic seizures. Bone marrow–depressing drugs used with succinimides can result in significant and fatal blood dyscrasias or conditions.
γ-Aminobutyric Acid Analogs (GABA)
Action
The mechanism of action for GABA analogs is not clearly understood. All of these drugs are chemically unrelated but they all increase the actions of GABA, which is an inhibitory neurotransmitter. It is thought that they might slow the sodium channel, helping to stabilize the neuronal membranes. Some of the newer GABA analogs also increase the action of GABA, block voltage of sodium channels, antagonize glutamate, and modulate calcium channels.
Uses
Although relatively new drugs, GABA analogs are used in the treatment, along with other antiepileptic drugs, for simple partial, complex partial, secondarily generalized, generalized tonic-clonic, and absence seizures. These medications are also used in treating peripheral neuropathy, post-herpatic neuralgia, and fibromyalgia.
Adverse Reactions
Adverse reactions include GI disturbances; weight gain; irregular menses; alopecia; pruritus; rashes, including erythema multiforme; photosensitivity; hair loss; anxiety; mood problems; tremor; and nervousness. Drowsiness and ataxia that are dose-dependent may also be seen. Inattention, anorexia, paresthesias, and renal stones may also be produced by some drugs.
Drug Interactions
Increased CNS depression may occur when valproic acid is administered with other CNS depressants, including other anticonvulsants and alcohol. These drugs interact with many other CNS drugs and may increase or decrease their blood levels. This is particularly true of phenytoin. It is advisable to monitor serum concentrations of any other anticonvulsants being used with these drugs to prevent overdosage.
Other Drugs
A variety of other products that are chemically unrelated have been in use for years in the treatment of seizures. New products continue to be developed in efforts to obtain better seizure control with reduced side effects. These products and their uses are listed in Table 16-3. All of these products have widespread usage for many different neurologic problems. Some also have other indications. For example, Valproic Acid (Depakote) is widely used in patients with bipolar symptoms and for migraine headaches.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about other drugs currently being taken that may produce drug interactions. Ask about other anticonvulsants, response to anticonvulsants taken in the past, hypersensitivity (allergy), and the possibility of pregnancy. Cardiac, respiratory, hepatic, or renal diseases are contraindications or precautions to the use of anticonvulsants.
n Diagnosis
For patients who are just starting on an antiseizure medication, find out what particular fears or concerns they have, as well as specific learning deficits. The diagnosis of these problems will help the nurse develop an appropriate nursing care plan to meet those needs. If the patient has alcohol and drug abuse problems, there may be problems with drug withdrawal, legal issues, or difficulties with compliance that will need to be part of the care plan.
n Planning
Older adult or weakened patients may be more sensitive to barbiturates and should be started on lower dosages. These patients are more likely to have hangover, confusion, and delirium.
Several of the anticonvulsant medications may produce blood dyscrasias or systemic lupus erythematosus. Benzodiazepines are changed by the liver into long-acting forms that may remain in the body for 24 hours or more and produce increased sedation; liver function may be affected with long-term use. In addition, there is a risk of congenital malformations and neonatal depression with most anticonvulsants, if used during pregnancy.
n Implementation
Barbiturates are legally controlled substances. They should not be given to patients with a history of abuse or addiction. Barbiturates should not be given to patients in pain, because these drugs may worsen the pain. When barbiturates are given parenterally, use great caution to avoid accidentally allowing the medicine to infiltrate tissues, because serious ischemia or gangrene could result. One of the major problems with this whole class of drugs is that they cause respiratory depression. This side effect has caused clinicians to turn to other drugs as they have become available.
When benzodiazepines are used in patients who have a mixed type of seizure activity, the drugs may increase or cause the onset of generalized tonic-clonic seizures. These drugs should also be used with caution in patients with poor or reduced renal function. Stopping the drugs quickly can produce status epilepticus.
The dosage of benzodiazepines is individualized for each patient, depending on the patient’s response. The onset of action is about for oral medicine is 30 to 60 minutes, and the effects last 7 to 8 hours. The drug should be given 15 to 30 minutes before bedtime. Older adult or weakened patients should receive reduced dosages of all anticonvulsants. It is important to very slowly increase or decrease dosages.
Oral phenytoin (Dilantin) suspension is often difficult to give accurately. The oral suspension should be shaken well before being given, and the liquid should not be frozen. Chewable tablets should not be used for once-a-day treatment.
Subcutaneous or perivascular (around the veins) injection of hydantoins should be avoided because of the highly alkaline nature of the solution. Hydantoins should be administered very slowly when given intravenously.
Talk to the patient and family about the chance of brief but short-term personality changes with phensuximide therapy. These should be reported to the nurse, physician, or other health care provider if they occur.
Once the patient is seizure-free with a particular drug, changing to phenytoin (Dilantin) products should be avoided. All dosages must be determined for the individual. The dosage for children is usually larger by weight than for adults. The patient is usually given a single dose within the therapeutic range, and then the amount is gradually increased until the seizures are controlled and the serum levels are stable, or until symptoms of overdosage or toxicity indicate that no further increases can be made.
Table 16-4 provides a list of important information about anticonvulsants, including dosages. A variety of miscellaneous anticonvulsants are also available. See Tables 16-2 and 16-3 for brief information about those products. Felbamate (Felbatol) has been used for partial seizures and Lennox-Gastaut syndrome. Enough cases of aplastic anemia and hepatic failure have developed from use of this drug that it carries a warning regarding its use.
![]() Table 16-4
Table 16-4
| GENERIC NAME | TRADE NAME | COMMENTS |
| Barbiturates | ||
| Long Acting | ||
| phenobarbital |
Luminal | Give IM in large muscle mass, because injection is very painful. Give slowly IV. |
| Phenobarbital | Some forms come in sustained-release capsules. Onset in 1 hr, effective for 16 hr. | |
| Benzodiazepines | ||
| clonazepam | Klonopin | Give initial doses. After 4-9 days, dosage may be increased by 0.5-1.5 mg/day every 3 days until seizures stop or until side effects prevent any further increase. |
| Whenever possible, give in 3 equally divided doses; if this is not possible, give the largest dose before bedtime. | ||
| clorazepate | Tranxene | |
| diazepam |
Valium | Comes PO, sustained-release capsules, and IV. |
| Parenteral therapy: Inject IV medication slowly only into large veins, 1 min for each 5 mg. May cause respiratory arrest if this is exceeded. | ||
| Hydantoins | ||
| fosphenytoin | Cerebyx | Continuously monitor ECG and vital signs. |
| phenytoin |
Dilantin | Monitor blood levels carefully. Watch for adverse neurologic effects. |
| Succinimides | ||
| phensuximide | Shake suspension well before pouring. Take drug with meals to decrease gastric discomfort. Efficacy of the drug decreases with long-term use. | |
| Miscellaneous Anticonvulsants | ||
| acetazolamide | Diamox | |
| carbamazepine | Tegretol | |
| gabapentin | Neurontin | Add-on therapy for patients older than 12 yr. Effective. |
| lamotrigine | Lamictal | Consult package insert for complex dosing instructions. |
| topiramate | Topamax | |
| valproic acid | Depakene | |
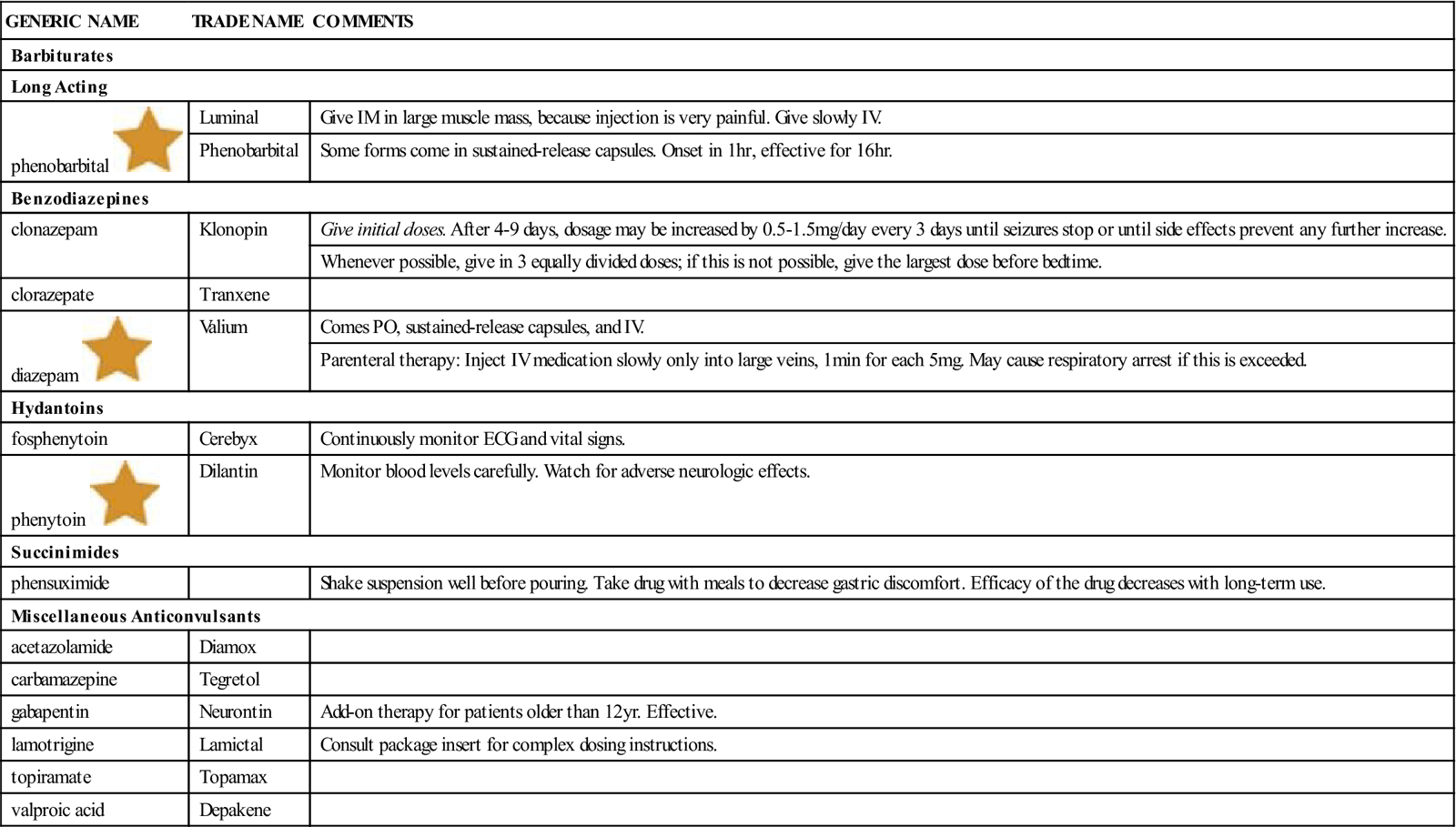
ECG, Electrocardiogram; IM, intramuscular; IV, intravenous; PO, by mouth.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
It takes several weeks before the success of an anticonvulsant dosage plan can be seen. The therapeutic effects should be monitored. Note seizure pattern and change. Note whether or not the sedation is a problem. Blood levels may be needed to see if the drug dosage is in the therapeutic range.
The patient’s compliance should be followed in regard to the amount of and times the drug is taken, any pattern of abuse, and drinking of alcohol. In addition, the patient should be asked about any paradoxical reactions and evaluated for tolerance, dependence, withdrawal, and toxicity. Liver toxicity is indicated by jaundice (yellow color of skin, eyes, and mucous membranes), rash, and sore throat.
The patient should keep a record of any seizures, with information about the time, length, characteristics, and reaction.
Complete blood cell counts and liver function tests should be followed as a baseline and repeated on a set schedule for patients on long-term barbiturate therapy.
Tolerance is usually related to the total amount of drug received. Dependence and withdrawal symptoms may occur if these drugs are used for very long periods. If the patient has been taking the drug for a long time, the drug should not be discontinued quickly.
Hydantoins are metabolized at various rates by patients; therefore, be alert to symptoms of toxicity. The patient should avoid alcohol while taking most anticonvulsants.
Adverse effects are common in long-term therapy. Gum overgrowth around the teeth (hyperplasia) is a typical finding with phenytoin (Dilantin) and may cause distress to the patient and family. The patient and family must be educated about how to prevent and treat this problem.
n Patient and Family Teaching
Tell the patient and family the following:
• Tablets and capsules should be kept in a dry, tightly closed container.
• Elixirs should be kept in a tightly closed, brown, glass bottle.
• Smoking may decrease the length of time benzodiazepines are effective.
• The liquid form of ethosuximide (Zarontin) should be shaken well before the dose is measured.
• Succinimide agents may make the urine appear pink, red, or reddish brown.
• Chewable tablets must be chewed or crushed before they are swallowed.
Antiemetic-Antivertigo Agents
Overview
Antiemetic or antivertigo agents are used to prevent and treat motion sickness and the nausea and vomiting that occur with anesthesia and surgery or cancer treatment. They are also used to treat severe, intractable (cannot be stopped by the usual treatment methods) vomiting and hiccups.
Action
The vomiting center of the brain may be stimulated by many factors: drugs, metabolic disorders, radiation, motion, gastric irritation, and vestibular neuritis. Vomiting is produced by direct action on the vomiting center of the brain, by indirect action through stimulation of the chemoreceptor trigger zone, and through increased activity of chemical neurotransmitters. Nausea and vomiting resulting from motion are probably caused by impulses to the vestibular network of the labyrinth system of the ear, which is located near the vomiting center. The impulses are conducted to the vomiting center by cholinergic nerves. Thus drugs that inhibit cholinergic nerve impulses should be effective in treating motion sickness.
Uses
Antidopaminergic agents such as chlorpromazine (Thorazine) and prochlorpromazine (Compazine) are used almost exclusively to control nausea and vomiting. Selected first generation H1 blocker antihistamine/anticholinergic medications are used to control motion sickness. Meclizine (Antivert) and dimenhydrinate (Dramamine) are the only products used to control acute vertigo. 5-HT3 antagonists such as ondansetron (Zofran) are routinely used prophylactically in patients expected to have nausea (e.g., patients undergoing chemotherapy).
Adverse Reactions
Drowsiness or sedation is the most common side effect of the anticholinergics, but tolerance to this reaction usually develops with long-term therapy. Patients may also feel dry mouth, stuffy nose, blurred vision, constipation, urinary retention, and other anticholinergic reactions.
Drug Interactions
The sedative effect of some antiemetic medications is increased (or potentiated) by other CNS depressants. Anticholinergic antiemetics can increase the anticholinergic side effects of many other drugs. The drug interactions may vary, depending on the type of antiemetic-antivertigo drug, but would be similar to other anticholinergic or antidopaminergic products. (See the earlier discussions about anticholinergic and antidopaminergic actions at the beginning of this chapter.)
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including episodes of motion sickness, extrapyramidal reactions caused by antipsychotic therapy, labyrinthitis, vertigo, Meniere disease, radiation therapy, or diabetes. Nausea and vomiting are common adverse reactions to drug therapy and may occur after taking almost any medication.
Find out whether the patient has a history of allergy, is currently using drugs that would cause drug interactions (especially MAO inhibitors), or is pregnant. In all cases, the underlying cause of vomiting, nausea, or vertigo should be found. In women of childbearing years, the possibility of pregnancy should always be considered. These drugs should not be used for treating morning sickness, because many drugs are not safe for the fetus.
Peppermint and ginger have been used in the treatment of motion sickness and nausea. Ask patients about the use of these herbs, because ginger has the potential to interact with anticoagulants, aspirin, NSAIDs, antiplatelet agents, and cardiac glycosides (digoxin).
n Diagnosis
For patients who have been vomiting for a long time or who have vertigo, other problems may develop. Is the patient dehydrated? Getting enough good food? Are there problems related to work or family because of the patient’s vomiting? Explore these areas to determine if there are problems that require action.
n Planning
Antiemetic and antivertigo agents should be used with extreme caution in patients doing tasks that require them to be mentally alert, because some of these products produce drowsiness. These agents are not recommended for use in children, because they may contribute to the development, the misdiagnosis, or the severity of symptoms in Reye syndrome, a brain encephalopathy that is often fatal in children.
Vomiting is often an important diagnostic clue and may point to a serious underlying problem. The cause of the vomiting or nausea should be found so that the best treatment can be given to get rid of the problem. Antiemetic drugs should not be the only form of therapy in cases of nausea or vomiting. Attempts to maintain hydration, restore electrolyte balance, and reduce other symptoms should be made.
n Implementation
All phenothiazine derivatives (chlorpromazine [Thorazine], prochlorperazine [Compazine] and promethazine [Phenergan]), turn the urine pink or reddish brown. They also may produce photosensitivity, so the patient should avoid exposure to sunlight. Antiemetic and antivertigo agents generally come in tablets, sustained-release capsules, and concentrates for oral use. For patients who are vomiting or so nauseated they are unable to take oral medications, injection or suppository forms are usually given.
The dose should be as low as possible, and therapy should be stopped as soon as possible. IV preparations should be reserved for severe cases in patients in the hospital. Medications given IM should be switched when the patient can tolerate oral agents.
Table 16-5 summarizes important information about antiemetic-antivertigo agents.
![]() Table 16-5
Table 16-5
Antiemetic and Antivertigo Agents
| GENERIC NAME | TRADE NAME | COMMENTS |
| Antidopaminergics | ||
| Phenothiazines | ||
| chlorpromazine | Thorazine | A phenothiazine derivative used to control nausea and vomiting and to treat intractable hiccups. |
| prochlorperazine |
Compazine | A phenothiazine derivative used to treat vomiting. |
| Available PO, sustained-release tablets, and IM. | ||
| promethazine | Phenergan | A phenothiazine derivative used to treat motion sickness and prevent and control nausea and vomiting associated with surgery and anesthesia. Caution: subcutaneous injection may cause tissue necrosis; intraarterial injection may produce gangrene of the extremity. |
| Motion sickness: Adults: 25 mg 30-60 min before travel, repeat 8-12 hr later PRN. On succeeding days, take 25 mg on arising and again before the evening meal. | ||
| Nausea and vomiting: Available PO, IM, IV, or suppository and topical cream. IV medication should be given to hospitalized patients only. | ||
| Preoperatively, may give equal doses of promethazine and a barbiturate or narcotic and an atropine-like drug. | ||
| Other | ||
| metoclopramide | Octamide | Give before meals and at bedtime. |
| Reglan | ||
| Anticholinergics | ||
| Antihistamines | ||
| dimenhydrinate | Dramamine | Antiemetic and antivertigo agent used in motion sickness, in radiation sickness, or following anesthesia. Appears to depress motion-induced stimulation of the labyrinthine structures; may alter blood counts. |
| diphenhydramine |
Benadryl | Antihistamine that blocks histamine receptors on peripheral effector cells. Has anticholinergic, antitussive, antiemetic, and sedative properties. With IV use, blood pressure should be carefully monitored. |
| Genahist | ||
| meclizine | Antivert | Antiemetic, anti-motion-sickness, and antivertigo agent with anticholinergic properties. Motion sickness: 50 mg 1 hr before departure; repeat q24h PRN. |
| Other | ||
| dronabinol | Marinol | Antiemetic primarily used for nausea and vomiting from chemotherapy. Give 5 mg/m2 1-3 hr before the administration of chemotherapy, then every 2-4 hr after chemotherapy is given, for a total of 4-6 doses/day. May be increased by 2.5 mg/m2 if dose is ineffective and no side effects have occurred. Use cautiously, because disturbing psychiatric symptoms develop with higher dosages. Also used as an appetite stimulant. |
| phosphorated carbohydrate solution | Emetrol (OTC) | Hyperosmolar carbohydrate solution that relieves nausea and vomiting by direct local action on the wall of the GI tract, reducing small muscle contraction. Used as antiemetic or for motion sickness. |
| Morning sickness: 15-30 mL on arising, and repeat every 3 hrs or when nausea threatens. | ||
| scopolamine | Transderm-Scōp | Comes as a transdermal patch, which is placed behind the ear and releases medication at a constant rate over a 3-day interval. The transdermal mechanism allows for lower dosage and produces fewer adverse anticholinergic effects than the oral forms. Scopolamine is used to control motion sickness in adults. Many contraindications. |
| Motion sickness: 0.24-0.8 mg PO 1 hr before anticipated travel. Long-term therapy: Apply 1 patch behind ear at least 4 hours before the antiemetic effect is desired; replace every 3 days for continued therapy. |
||
| trimethobenzamide | Tigan | Antiemetic that inhibits the chemoreceptor trigger zone in the medulla; used to control nausea and vomiting. Drug has been linked to the development of Reye syndrome in children. Give deep IM; solution is highly irritating to tissues. |
| 5-HT Receptor Antagonists | ||
| dolasetron | Anzemet | Controlling nausea and vomiting associated with chemotherapy: Give within 1 hr before chemotherapy. Lower dosages may be given to control postoperative vomiting. |
| granisetron | Kytril | Used for prevention of nausea and vomiting associated with initial and repeat courses of chemotherapy. |
| ondansetron | Zofran | Used in controlling nausea and vomiting associated with chemotherapy. See package insert for complex dosing instructions. May be given IV, suppository, solution, or tablet. |
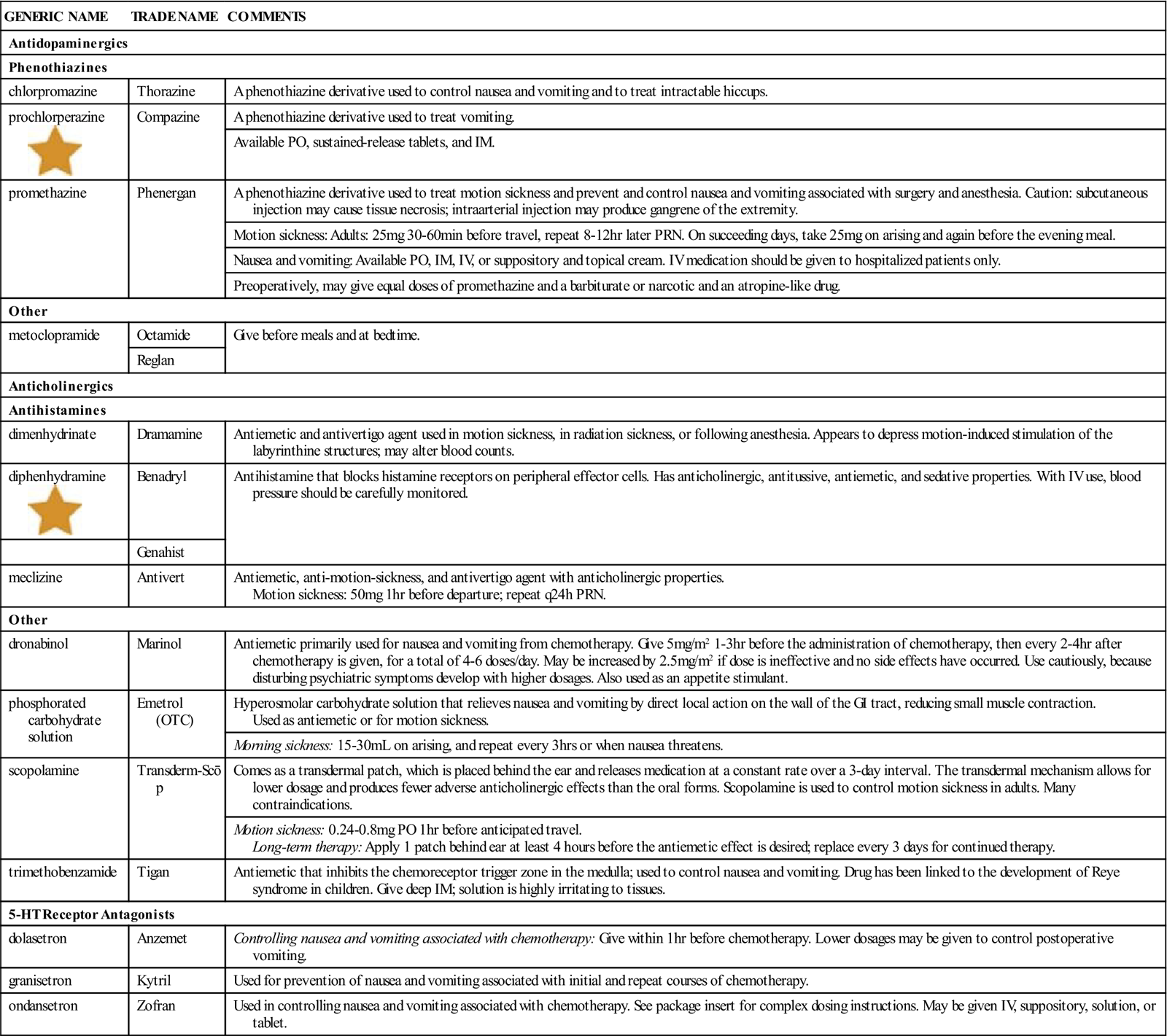
5-HT, 5-Hydroxytriptamine; GI, gastrointestinal; IM, intramuscular; IV, intravenous; OTC, over the counter; PO, by mouth; PRN, as needed.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
The nurse should monitor for therapeutic effectiveness and side effects.
n Patient and Family Teaching
Tell the patient and family the following:
Antiparkinsonian Agents
Overview
Parkinson disease is a chronic disorder of the CNS. The cause is unknown, but it is thought to involve an imbalance in chemical neurotransmitters within the brain. Problems seem to stem from too much acetylcholine and not enough dopamine in the basal ganglia. Medicine for Parkinson disease is designed to replace dopamaine, as well as to control symptoms. Common symptoms are fine muscle tremors while they are at rest, slowness of movement, rigidity, muscle weakness, a characteristic shuffling, forward-pitched gait, and resulting changes in posture and balance. Patients often develop dementia as time progresses.There is no known cure for Parkinson disease. Treatment goals are designed to relieve symptoms and maintain movement and activity of the patient.
Action
The two main actions of the antiparkinsonian agents are to: (1) block the uptake of acetylcholine at postsynaptic muscarinic cholinergic receptor sites; and (2) elevate the functional levels of dopamine in motor regulatory centers. These drugs exert a wide range of effects on all the tissue affected by the autonomic nervous system, including the eyes, respiratory tract, heart, GI tract, urinary bladder, nonvascular smooth muscle, exocrine glands, and CNS. Antiparkinsonian agents reduce muscle tremors and rigidity and improve mobility, muscular coordination, and performance.
Uses
Antiparkinsonian agents are anticholinergic and dopaminergic drugs used to control the symptoms of Parkinson disease. Amantadine (Symmetrel) was originally introduced as an antiviral agent for the prophylaxis of Influenza A but was unexpectedly found to cause improvement in symptoms. The patient may achieve good control of symptoms for a while with these drugs but patients develop tolerance to the drugs, requiring frequent readjustment of doses and medications.
Adverse Reactions
Dopaminergic agents may produce dysrhythmias (irregular heartbeats), muscle twitching, psychotic reactions, rigidity, diarrhea, epigastric distress, GI bleeding, nausea, vomiting, blurred vision, alopecia, bitter taste, hot flashes, rash, and urinary retention.
Anticholinergic agents may cause postural hypotension (low blood pressure when a person suddenly stands up), tachycardia, agitation, confusion, depression, headache, memory loss, muscle cramping, constipation, vomiting, diplopia (double vision), increased intraocular pressure, decreased sweating, flushing, dry mouth, and skin rash.
Early signs of toxicity in the patient taking dopaminergic agents include muscle twitching and blepharospasm (eyelid spasms). Overdosage is a common phenomenon, particularly with long-term drug therapy. It is recognizable because the patient experiences a sudden onset of progressively worsening parkinsonian symptoms. These drugs should be tapered gradually.
Drug Interactions
Common drug interactions differ, according to whether the preparation is an anticholinergic or a dopaminergic agent. These drugs commonly interact with many types of medications; product information must be closely studied. These patients often take antipsychotics, which have the potential to interact with these antiparkinson drugs. Two herbal products, ginkgo and grape seed, are commonly used to treat symptoms of Parkinson disease. The Complementary and Alternative Therapies box summarizes these products and their drug interactions.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including hypersensitivity; drugs currently being taken that may produce drug interactions; asthma, renal, liver, and cardiovascular disease and epilepsy; other contraindications for the drug; and the possibility of pregnancy.
The patient may have a history of Parkinson disease, drooling, or difficulty with coordination and walking. The patient may be taking an antipsychotic drug; with long-term use, these drugs can cause tardive dyskinesia, with symptoms similar to those of Parkinson disease. The patient may be middle-aged or an older adult and may have tremors at rest that are made worse by emotional stress. The arms may fail to move when walking, with rigidity first occurring in the proximal musculature, and the patient may be unable to perform activities of daily living.
n Diagnosis
These patients frequently have other problems as a result of their medical diagnosis. Ataxia (staggered walking) frequently leads to falls and soft-tissue and bone injuries. They may have breakdown of the skin, poor hygiene, poor nutrition, or other problems related to immobility or difficulty walking, cooking, and so on. Their intelligence and ability to understand may be underestimated when they are unable to communicate well. They are frequently angry, depressed, and lonely. If the nurse is willing to spend the time learning to communicate with the patient, they will gain a clear picture of the multitude of problems relevant to the patient.
n Planning
There is a wide variety of medications given for Parkinson’s disease and medications are frequently changed as patients develop tolerance to them. See Table 16-6 for details about specific agents. Anticholonergic agents are contraindicated for persons with known hypersensitivity, acute narrow-angle glaucoma, asthma, history of epilepsy, peptic ulcer disease, and skin lesions. Persons on CNS stimulants, those exposed to rubella (measles), those with acute psychoses, those with a history of melanoma, or patients receiving MAO inhibitor therapy should not take these medications. These drugs are known to aggravate many other diseases and must be used with caution.
The anticholinergics and some dopaminergics must be withdrawn slowly, because many of these drugs have a long half-life. When withdrawing one preparation and beginning a new preparation, the new drug should be started in small doses and the old drug should be withdrawn gradually. These agents are usually initiated at the lowest dosage possible, and the dosage is increased gradually until the maximum therapeutic effect has been obtained.
n Implementation
These drugs are available in tablets, sustained-release capsules, syrup, and elixir. They are generally well absorbed from the GI tract. Peak blood levels of carbidopa-levodopa (Sinemet), one of the main treatment drugs, are achieved in 1 to 6 hours, depending on the route of administration and the type of drug administered, except for the sustained-release capsules, which reach peak plasma blood levels in 8 to 12 hours. Sustained-release capsules are not recommended for initial therapy, because they do not allow enough flexibility in dosage regulation. IV injection of anticholinergics can cause hypotension and incoordination.
Although dopamine cannot cross the blood-brain barrier, levodopa can move into the brain, where it is converted into dopamine. However, levodopa alone becomes less effective over time, and side effects are related to the dose. Therefore carbidopa and levodopa are often administered together, usually as a fixed-combination product (Sinemet). Carbidopa is added to prevent peripheral breakdown of levodopa and reduce the overall dose of levodopa required.
If this combination drug is administered after levodopa therapy, the levodopa should be discontinued at least 8 hours before initiating therapy with carbidopa-levodopa. The carbidopa-levodopa combination should be substituted at a dosage level that provides 25% of the previous levodopa dose. When the fixed-combination dose is excessive, carbidopa can be given separately with levodopa so that each drug can be titrated individually.
Table 16-6 summarizes the important medications used to treat Parkinson disease.
![]() Table 16-6
Table 16-6
| GENERIC NAME | TRADE NAME | COMMENTS |
| Anticholinergic Drugs | ||
| benztropine | Cogentin | Contains anticholinergic and antihistamine properties. Pharmacologically, drug inhibits excessive cholinergic activity in striatal fibers. Used to treat extrapyramidal symptoms (except tardive dyskinesia) induced by antipsychotic agents. IM injection provides rapid (15 min) relief from acute dystonic reactions. Oral doses of the drug are cumulative; therefore therapy should begin with a low dose and increase gradually at 5- to 6-day intervals as necessary. |
| Used for parkinsonian symptoms and drug-induced extrapyramidal side effects. | ||
| biperiden | Akineton | Blocks central cholinergic receptors, restoring balance between cholinergic and dopaminergic activity in basal ganglia. IV or IM administration may produce incoordination. |
| Used for parkinsonian symptoms and drug-induced extrapyramidal side effects. | ||
| diphenhydramine |
Benadryl | Blocks receptors on peripheral effector cells. |
| Used in idiopathic parkinsonism treatment. | ||
| trihexyphenidyl | Artane | Exerts direct inhibitory effect on the parasympathetic nervous system. Decreases rigidity, but most other symptoms improve to some degree. |
| Dopaminergic Drugs | ||
| amantadine | Symmetrel | This drug enhances release of dopamine from presynaptic nerve endings. Drug has no anticholinergic activity. Used for parkinsonian symptoms and drug-induced extrapyramidal side effects. |
| bromocriptine | Parlodel | Directly stimulates dopamine receptors in corpus striatum; especially helpful in patients who are beginning to deteriorate or develop tolerance to levodopa. |
| carbidopa | Lodosyn | Used with levodopa to slow the breakdown of levodopa; has no therapeutic action itself. Used when treatment requires separate titration of each drug. |
| carbidopa-levodopa | Sinemet–10/100 Sinemet–25/100 Sinemet–25/250 Sinemet–50/200 |
Fixed-combination antiparkinsonian agent used in all types of treatment of Parkinson disease. Composed of both carbidopa and levodopa. Tablet strength indicated by numbering (mg carbidopa/mg levodopa). For patients not receiving levodopa: 1 tablet (10/100 or 25/100) 3 times daily initially; increased by 1 tablet daily until a maximum of 8 tablets is given. For patients receiving levodopa, levodopa must be discontinued at least 8 hr before initiating therapy with this product. Administer 1 tablet (25/250) 3 to 4 times daily to patients previously requiring 1500 mg or more of levodopa each day. |
| entacapone | Comtan | Used as adjunct to carbidopa-levodopa to treat patients with idiopathic Parkinson disease who experience the signs and symptoms of end-of-dose “wearing-off.” Given as 200-mg tablet with each carbidopa-levodopa dosage. |
| levodopa | Dopar | A metabolic precursor of dopamine. Enters CNS by crossing blood-brain barrier and is converted to dopamine. |
| Larodopa | ||
| selegiline | Eldepryl | Irreversible MAO inhibitor. Usual dose 5 mg at breakfast and lunch; allows carbidopa-levodopa dosages to be reduced. |
| Carbex | ||
| tolcapone | Tasmar | May cause hallucinations and tardive dyskinesia. Give without food and always as adjunctive therapy to carbidopa-levodopa therapy. |
| Dopamine Receptor Agonists, Nonergot | ||
| pramipexole | Mirapex | Binds with high affinity to dopamine D3 receptors. May stimulate dopamine receptors in the striatum. Follow precise dosing schedule in package insert. |
| ropinirole | Requip | Follow precise dosing schedule listed in package insert. |
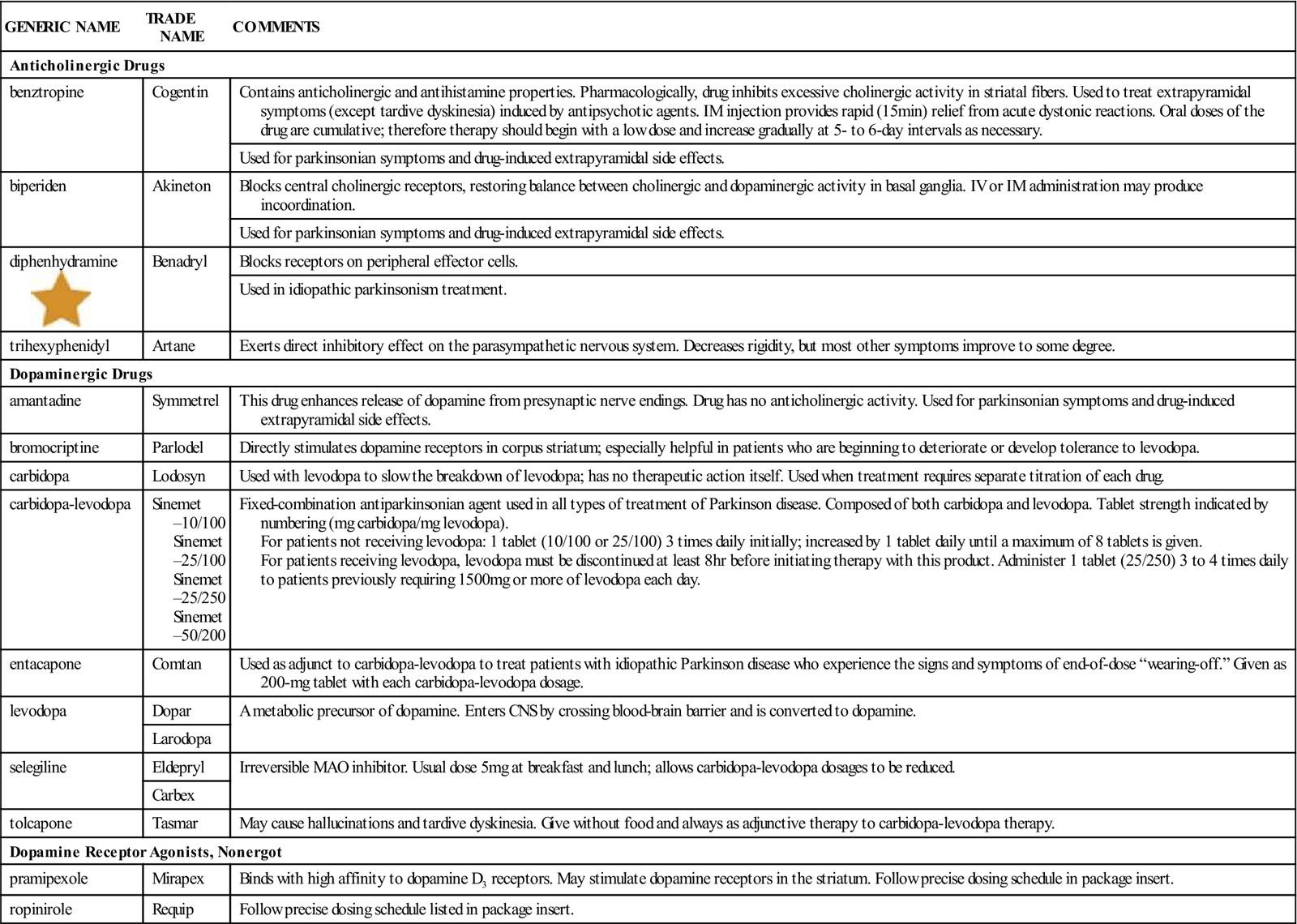
CNS, Central nervous system; IM, intramuscular; IV, intravenous; MAO, monoamine oxidase.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
Long-term use of dopaminergic and anticholinergic agents often leads to akinesia (loss of movement), tardive dyskinesia (abnormal and involuntary movements especially of the lower face), and dystonia (impairment of muscle tone). To reverse these effects, the dosage is likely to be reduced to the minimum effective level and very slow and careful changes in dosages made as necessary to avoid overmedication.
Numerous laboratory tests may be altered by these medications; this should be taken into account when monitoring patient status.
n Patient and Family Teaching
Psychotherapeutic Agents
Overview
Many of the drugs introduced in the following subsections act on more than one type of neuroreceptor. Each agent acts differently, making it possible for certain drugs to be given for specific actions without many adverse reactions. It should be clear that if dosages are exceeded, many receptors may be excessively stimulated, causing widespread and serious effects.
 Antianxiety Agents
Antianxiety Agents
Anxiety is a common problem associated with many medical and surgical conditions, as well as a primary symptom in many psychiatric disorders. Anxiety is a normal human emotion, but when it is felt too frequently or interferes with a person’s ability to perform activities of daily living, it is considered abnormal. There are a number of disorders associated with anxiety. Anxiety creates subjective feelings of helplessness, indecision, worry, apprehension, and irritability. Patients may complain of headache, gastric distress, and inability to concentrate. It may also produce objective symptoms of restlessness, tremor, constipation, diarrhea, nausea, and muscle tension. Insomnia is one of the most common problems associated with anxiety.
Specific regions of the brain produce symptoms of anxiety. There are a number of strategies that are used to prevent, control, or treat anxiety. When anxiety is so severe that it must be treated with medication, antianxiety medications such as benzodiazepines are used to reduce some of the symptoms. They do not prevent the anxiety, because the feelings or problems that produce the anxiety are still there. These are the products commonly referred to as tranquilizers. Some other medications such as the SSRIs act at the level of the brain to prevent feelings of anxiety. In general, antianxiety medication should be used for only a short time until other remedies can be found. It is especially important to view the use of these medications as a short-term solution because of the potential for addiction of these agents.
The major products used today for anxiety are the benzodiazepines, accounting for approximately 75% of the antianxiety prescriptions written today. Although benzodiazepines have a variety of uses, there are particular drugs in this category that are used primarily for treating anxiety. These drugs are intended primarily for short-term treatment of anxiety or related insomnia. Other antianxiety agents are briefly included in this discussion.
The other drugs used for treating anxiety are categorized as nonbezodiazepine antianxiety agents. These include buspirone (BuSpar), doxepin (Sinequan), and hydroxyzine (Hypan and Vistaril).
Action
Benzodiazepines are thought to act at the limbic, thalamic, and hypothalamic levels of the CNS, producing a calming effect.
Uses
Benzodiazepines such as alprazolam (Xanax) and diazepam (Valium), as well and nonbenzodiazepines, are used to relieve anxiety, tension, and fears that occur by themselves or as the result of illness. Other indications include management of delirium tremens after alcohol withdrawal; premedication for surgical and endoscopic procedures or electric cardioversion; treatment of convulsive disorders (diazepam only); and relief of muscle spasm.
Adverse Reactions
Adverse reactions to antianxiety agents include hypotension, tachycardia, clumsiness, confusion, depression, drowsiness, fatigue, headache, insomnia, paradoxical reactions (excitement, hallucinations, agitation, hostility, or rage), syncope (light-headedness and fainting), unsteadiness, visual disturbances, weakness, anorexia, constipation, difficulty swallowing, dry mouth, hiccups, jaundice, nausea, vomiting, urinary retention, blood cell changes, pruritus, skin rash, joint pain, and unexplained sore throat and fever.
Overdosage may produce sleepiness, confusion, coma, diminished reflexes, and hypotension. Tolerance is easily developed.
Drug Interactions
Giving benzodiazepines along with any of the following substances may increase the effect of either agent: alcohol; anesthetics; MAO inhibitors; or CNS depressants such as antihistamines, barbiturates, phenothiazines, narcotics, sedatives, tranquilizers, hypnotics, anticonvulsants, or tricyclic antidepressants (TCAs). Caffeinated products and excessive cigarette smoking can antagonize (decrease) the anxiolytic (antianxiety) effect of these drugs. Herbal products are also often used by patients to treat stress and anxiety. The Complementary and Alternative Therapies box summarizes herbal preparations the patient may be using and their drug interactions.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including hypersensitivities, underlying systemic disease (especially pulmonary, cardiac, liver, or renal disease; epilepsy or seizures; myasthenia gravis; mental illness; and drug abuse or dependence), possibility of pregnancy, breastfeeding, or whether the patient is currently taking any medications (both prescribed and OTC) that may produce drug interactions. These conditions are contraindications or precautions to the use of antianxiety agents.
The patient may have a history of feelings of apprehension, uncertainty, fear, an unpleasant state of tension, a sense of impending doom, insomnia (inability to sleep), irritability, hypersensitivity to stress, difficulty in concentrating, or nightmares.
n Diagnosis
In addition to the medical diagnosis, what other problems does the patient experience? Does he or she have family support, or is he or she isolated and lonely? Is the patient able to work and take care of daily needs, or is the patient incapacitated with anxiety? Does the patient have to drive long distances or do careful, precision work that requires steady muscles and nerves?
n Planning
Older adult patients (older than age 60) and those with chronic illnesses may require a decreased initial dosage and may need careful monitoring of individual response before changes in dosage are made. These drugs are potentially harmful in the elderly if the patient is not closely supervised. Benzodiazepines generally have a long half-life and can have cumulative effects. Patients with a history of seizures or epilepsy should have their dosages of benzodiazepines tapered slowly.
n Implementation
Administering the benzodiazepines during or immediately after meals decreases the incidence of GI side effects. The manufacturers’ instructions for diluting and slowly injecting parenteral medications should be followed to prevent the possibility of severe respiratory depression and failure.
Patients with anxiety are often depressed and depressed patients may have anxiety. Because both conditions are so commonly seen together, patients should be questioned and observed for suicidal tendencies.
Treatment with antianxiety agents should proceed slowly in older adults, the debilitated, those with limited pulmonary reserve, and those in whom a hypotensive episode might precipitate heart problems.
Table 16-7 summarizes important dosage information about antianxiety medications.
![]() Table 16-7
Table 16-7
| GENERIC NAME | TRADE NAME | COMMENTS |
| Benzodiazepines | ||
| alprazolam | Xanax | Action peaks in 1-2 hr; half-life 12-15 hr. Effectiveness and safety in children younger than the age of 18 have not been determined. Give reduced dosage in older adult or debilitated patients. |
| chlordiazepoxide | H-Tran | Peak levels in 1-4 hr; half-life 5-30 hr. Food or antacids slow absorption. Injection IV must be very slow to avoid producing respiratory arrest. |
| Librium | ||
| Give reduced dosage in older adult or debilitated patients. | ||
| clorazepate | Tranxene | Peak effect in 60 min; half-life 2 days. Some reports indicate a fall in hematocrit with long-term use. Can be given once each day. |
| Give reduced dosage in older adult or debilitated patients. | ||
| diazepam |
Valium | Peak blood levels reached within 1-2 hr; half-life 20-50 hr. |
| Anxiety and management of convulsive disorders. Also used for skeletal muscle spasm. Give reduced dosage in older adult or debilitated patients. | ||
| lorazepam | Ativan | Action peaks in  hr; half-life 10-15 hr. Patients may experience withdrawal manifested as insomnia 2 or 3 nights after cessation of therapy. IM injection used as a preanesthetic agent for adults only. Also given IV for sedation and relief of anxiety. hr; half-life 10-15 hr. Patients may experience withdrawal manifested as insomnia 2 or 3 nights after cessation of therapy. IM injection used as a preanesthetic agent for adults only. Also given IV for sedation and relief of anxiety. |
| Used for anxiety and insomnia. Give reduced dosage in older adult or debilitated patients. | ||
| oxazepam | Serax | Peak blood levels at 2-4 hr; half-life 5-20 hr. Low incidence of toxicity. Used for anxiety. Give reduced dosage in older adult or debilitated patients. |
| Nonbenzodiazepine Antianxiety Agents | ||
| buspirone | BuSpar | Approved for short-term use in anxiety disorders. Mechanism of action unknown; chemically unrelated to other antianxiety medications. |
| doxepin | Sinequan | For oral concentrate, do not mix with grape juice. |
| hydroxyzine | Hy-Pam | Antihistamine for symptomatic relief of anxiety, especially in psychoneurosis. Also has analgesic activity that may be helpful in relieving pruritus caused by allergies. Medication may be used preoperatively for surgery or obstetric patients to permit decrease in narcotic dosages, reduce anxiety, and control emesis. Product also helps control acutely disturbed or hysterical patients. For IM use only. Caution: subcutaneous, intraarterial, or IV use may produce tissue necrosis and hemolysis. |
| Vistaril | ||
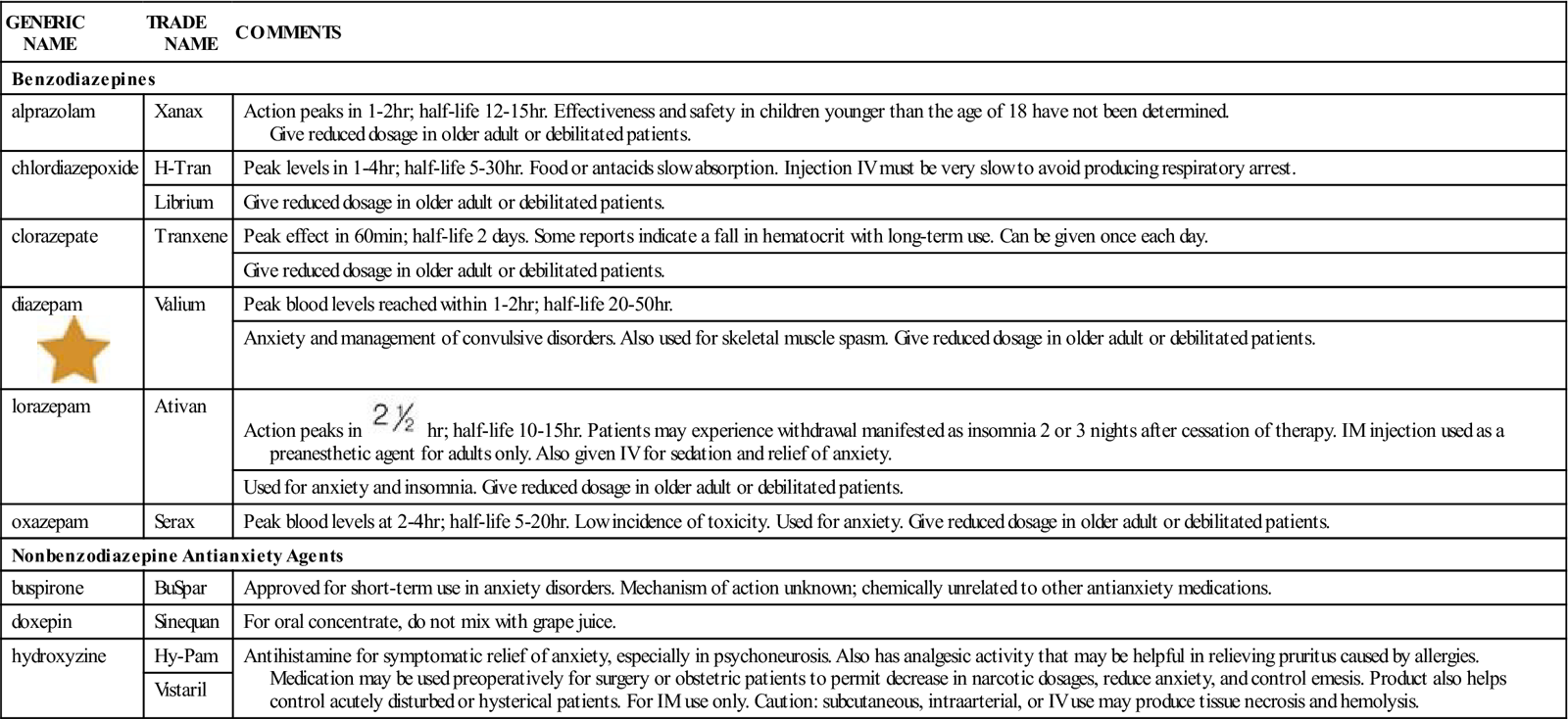
IM, Intramuscular; IV, intravenous.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
Mental alertness, cognitive functions, and physical abilities may be impaired with the use of antianxiety agents. These drugs should be given in conjunction with counseling or psychotherapy for maximum benefit.
Abrupt termination of these agents may cause delayed withdrawal symptoms (up to 1 week later) of abdominal or muscle cramps, vomiting, diaphoresis (sweating), tremor, or convulsions. Tapering the dosage for patients on long-term therapy helps prevent this problem.
Take the patient’s blood pressure lying, sitting, and standing to monitor for hypotensive changes.
Alternatives for coping with stress and change should be discussed with the patient. For example, increased regular physical activity, muscle relaxation exercises, and participation in hobbies may be helpful.
n Patient and Family Teaching
 Antidepressants
Antidepressants
Overview
Depression, whether mild or so severe that it interferes with activities of daily living, has been recognized for centuries. Most people have days when they feel “down” or “blue.” Sometimes people have good reasons to be depressed. But intense and prolonged inability to interact with others, go to work, and keep up with the activities of daily life represent more significant depression. Sometimes hormones, substance abuse, or medications taken for other problems may produce depression. There may be a family history of depression, as some conditions seem genetic. There are several different categories of depression including milder dysthymic disorder, major depressive disorder, and bipolar disorder. Many types of therapy have been explored, but only in the last 30 years have medications been discovered that significantly help improve a patient’s mood without extensive side or adverse effects from each drug. Although all medications are equally effective in treating depression if they work, not all patients respond to all medications and patients may experience different side effects with each drug. So if a patient does not respond to one drug, there are many more drugs which might be tried to see which has the best antidepressant effect and the fewest side effects. Research has demonstrated that the best treatment for severe depression involves both psychotherapy and medication.
There are now several new categories of drugs that are used in treating depression. These drugs elevate the mood by affecting neurotransmitters in the brain, primarily norepinephrine and serotonin (Figures 16-3 and 16-4). MAO inhibitors were initially used to treat other diseases. The antidepressant effect was discovered as an unexpected side effect of that therapy. They were then used to treat depressed patients until TCA therapy became available in the 1960s. MAO inhibitors are now ordered primarily when tricyclic therapy is unsatisfactory. In the last few years, a number of other drugs have entered the field for treatment of depressed patients, including several that act on serotonin or norepinephrine reuptake. Each of these groups is discussed separately.
All antidepressants now carry a black box warning detailing the risk of suicide in children and adolescents who are taking medications. The antidepressants may cause young adults to become suicidal, so the benefit must be weighed against the risk of increased suicidality. Patients taking these medications must be observed closely for clinical worsening, suicidality, or unusual changes in behavior, particularly within the first few months of starting therapy or when dosage changes.
None of these drugs should be abruptly stopped by the patient. Care must be taken to teach the patient about gradually reducing the drugs as directed by the health care provider when the drug is to be discontinued.
Tricyclic Antidepressants
Action
The antidepressant effect of tricyclics is not completely understood. It is thought that tricyclic antidepressants (TCAs) potentiate the effects of or inhibit the uptake of norepinephrine andserotonin (biogenic amines) by the presynaptic neuronal membrane in the CNS, thereby increasing the concentration of these biogenic amines at the synapse.
Uses
TCAs are used primarily to relieve the symptoms of severe depression that has internal biologic causes (endogenous depression). They may also be used to treat mild depression caused by factors in the patient’s life (exogenous or reactive depression), which is not self-limiting and does not interfere with usual activities of daily living. They are less commonly used for bipolar disorders as adjunctive or additional therapy.
Adverse Reactions
Adverse reactions to TCAs include dysrhythmias, postural hypotension, confusion, headache, drowsiness that lasts a long time, constipation, nausea, vomiting, blood dyscrasias, fever, photosensitivity, pruritus, skin rash, muscle twitching, tremors, urinary hesitancy or retention, altered liver function tests, blurred vision, and nervousness.
Overdosage may initially produce stimulation of the CNS, resulting in irritability, agitation, hallucinations, delirium, twitching, hypertonia, hyperreflexia, nystagmus, hyperpyrexia (very high body temperature), hypertension, and seizures (more commonly seen in children). This initial CNS stimulation is followed by CNS depression, causing drowsiness, areflexia, hypothermia (abnormally low body temperature), hypotension, dysrhythmias, respiratory depression, coma, or cardiorespiratory arrest.
Drug Interactions
TCA increase the CNS depressant effect of alcohol and other CNS depressants, particularly ethchlorvynol (Placidyl). The effects of anticonvulsants may be decreased when used with TCAs. The antihypertensive effects of guanethidine (Ismelin) and clonidine (Catapres) may be blocked when used with most TCAs, with the exception of doxepin (Sinequan). There may be a reduction in the antidepressant effect of tricyclics and an increase in their side effects when used concurrently with estrogen, including oral contraceptives containing estrogen. An increased incidence of cardiac dysrhythmias has been found with concurrent use of thyroid medication and TCAs. Severe hypertension or hyperpyrexia may result when TCAs are used with MAO inhibitors or sympathomimetics.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient; allergy, disease, and other medications the patient may currently be taking, including OTC preparations, must be considered. Many diseases present contraindications or precautions for the use of tricyclic drugs. Patients may be taking herbal remedies to help with symptoms of depression. The Complementary and Alternative Therapies box provides a summary of herbal products and their drug interactions.
Patients experiencing clinical depression may have a history of insomnia, early morning awakening, anorexia, constipation, loss of motivation, and fatigue. They may express feelings of hopelessness and pessimism, say negative things about themselves, respond slowly to questions, and have slowed motor movements, decreased facial expression, and stooped posture. Assess these patients thoroughly for any suicidal feelings.
n Diagnosis
What problems does the depressed patient have that necessitate nursing intervention? Does the patient eat, bathe, and dress appropriately? Has contact with other people been cut off? Is the patient unable to work? Any of these problems may be addressed once the therapeutic effects of antidepressant medication have eased the patient’s immediate crisis.
n Planning
If the patient has taken any antidepressant drugs before, get a careful history about what medications they took and their response, including any adverse effects. TCAs should not be given if the patient has a history of hypersensitivity to a TCA. A patient who is hypersensitive to one type of tricyclic will likely be sensitive to all tricyclics (cross-sensitivity). Patients with a history of recent myocardial infarction, narrow-angle glaucoma, or severe hepatic or renal failure also should not take these drugs. TCAs should be used very carefully with MAO inhibitors. Discuss the importance of contraception with women of childbearing age who are taking TCAs.
Antidepressants may cause patients with bipolar disorder to go into the manic phase of their illness; exaggerated symptoms of paranoid ideation and schizophrenia may develop in patients who have these disorders. The prescribing health care provider may need to reduce the dosage of the TCA or add a medication to reduce anxiety.
Antidepressants are started in low doses which are increased slowly until the depression is relieved or adverse effects develop. Prescriptions are often given for only the smallest but reasonable amount of antidepressant because the patients should be regarded as potentially suicidal. Patients should be observed taking their pills so they cannot save them up and take them all at one time.
n Implementation
It is often difficult to determine the most appropriate dose for the patient. The plasma concentrations of TCAs vary widely and may not correspond well with the dosage or therapeutic effects. Thus, the initial and maintenance dosages of these drugs must be carefully determined, based on the patient’s age, physical health status, and response to the drug.
Patient’s may experience drowsiness or sedation with the initial dose, especially when the patient is taking a tricyclic known to have moderate to strong sedative effects. Therefore TCA therapy will likely be started with a single bedtime dose, especially for patients who are depressed and also have a sleep disturbance. Typically, the drug dosage is then adjusted or titrated to achieve the best response with the lowest dosage and minimal side effects. A maintenance dosage, administered in divided doses or as a single bedtime dose, may be continued for 6 months to 1 year. The patient should be reevaluated at this time to determine the course of therapy.
Table 16-8 summarizes the important information nurses should know about TCA medications.
![]() Table 16-8
Table 16-8
| GENERIC NAME | TRADE NAME | COMMENTS |
| amitriptyline |
Strong sedative effect, especially early in therapy. Should be taken at bedtime to decrease daytime drowsiness. Used to treat endogenous depression accompanied by anxiety. | |
| doxepin | Sinequan | Has marked sedative effect, particularly during initial phase of therapy. Used to treat psychotic and psychoneurotic depression with associated anxiety and somatic symptoms. Oral concentrate should be diluted in milk, fruit juice, or water before administration. |
| imipramine | Tofranil | Used to treat endogenous depression; only tricyclic that is also used to treat enuresis in children. |
| nortriptyline | Aventyl | Used to treat endogenous depression. |
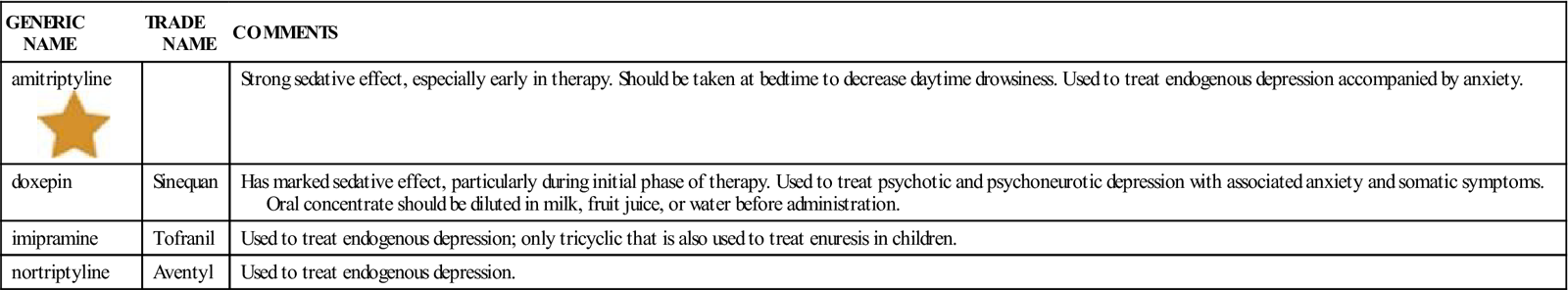
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
The desired antidepressant effect of the drug will usually occur within 3 to 4 weeks after therapy is initiated.
If a TCA is given in large doses or for a long time, the drug should be stopped by gradually reducing the dose over 4 to 8 weeks to avoid withdrawal symptoms of general listlessness, headache, and nausea.
n Patient and Family Teaching
Tell the patient and family the following:
Monoamine Oxidase Inhibitors (MAOIs)
Action
MAO is an enzyme found in the mitochondria of cells located in nerve endings and other body tissues such as the kidney, liver, and intestines. This enzyme normally acts as a catalyst by inactivating dopamine, norepinephrine, epinephrine, and serotonin (biogenic amines) and therefore regulating the intracellular levels of these neurotransmitters. MAO inhibitors block the inactivation of the biogenic amines, resulting in an increased concentration of dopamine, epinephrine, norepinephrine, and serotonin at neuronal synapses. The antidepressant effects of MAO inhibitors such as phenelzine (Nardil) or tranylcypromine (Parnate) are thought to be directly related to this increased concentration of biogenic amines.
Uses
MAO inhibitors are used to relieve the symptoms of severe reactive or endogenous depression that have not responded to TCA therapy, electroconvulsive therapy, or other modes of psychotherapy. Effects may be seen within days but the full antidepressant effect is often delayed for weeks. MAO inhibitors are considered second-line treatment for depression because of their serious adverse effects. MAO inhibitors are not approved for use in children.
Adverse Reactions
Adverse reactions to MAO inhibitors include postural hypotension, dysrhythmias, ataxia, drowsiness, hallucinations, headache, hyperactivity, insomnia, seizures, tremors, vertigo, anorexia, constipation, diarrhea, nausea, vomiting, fever, photosensitivity, skin rash, dysuria (painful urination), incontinence, blurred vision, dry mouth, edema, and impotence.
Overdosage produces mental confusion, restlessness, hypotension, respiratory depression, tachycardia, seizures, and shock, which may persist for 1 to 2 weeks.
Drug and Food Interactions
MAO inhibitors have many drug interactions. The potential for drug interactions differs between agents based upon the type of MAO inhibition that occurs. Drugs that inhibit MAO A may interact with other serotonergic agents, causing a potentially fatal serotonin syndrome characterized by mental status changes, myoclonus, fever, and tremor. Therefore, concurrent use of MAO A inhibitors with medications such as SSRIs, meperidine, dextromethorphan, sumatriptan, and buspirone should be avoided. Conversely, MAO B inhibitors, such as selegiline, may interact with other dominergic drugs such as amantadine and bromocriptine.
MAOIs may potentiate the CNS depressant effect of alcohol, anesthetics, sedatives, hypnotics, and narcotics and may cause severe hypertension and hyperpyrexia. If they are used with anticonvulsants, they may cause a change in the seizure pattern of the patient, and the dosage of the anticonvulsant medication may have to be adjusted accordingly. The hypotensive effects of diuretics and antihypertensives may be enhanced when those agents are used with MAO inhibitors. The hypoglycemic effects of insulin or oral hypoglycemics may be enhanced by MAO inhibitors, and dosages may require adjustment accordingly. MAO inhibitors and tricyclic antidepressants are generally not used together because hyperpyrexia, severe convulsions, hypertensive crisis, and death may result. MAOIs should not be given with other MAOIs drugs.
Foods with more than 6 mg of tyramine per serving must be avoided: These include aged and mature cheeses, air-dried sausages (e.g., pepperoni), fermented soy products (soy and teriyaki sauce), sauerkraut, and all tap beers, to name a few.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the presence of any diseases that may contraindicate the use of MAO inhibitors. The patient should be asked about other medications including OTC and herbal products (particularly St John’s Wort) currently being taken (especially TCAs) and the possibility of pregnancy. Also assess the level of the patient’s depression and check for suicidal ideas.
n Diagnosis
What other problems does the patient have as a result of this diagnosis? Is the patient able to understand the dietary restrictions that must be followed while taking these medications? What self-care assistance does the patient need? The nurse should focus on things to teach or learn about the patient that will provide encouragement and support in getting well.
n Planning
The safe use of MAO inhibitors in pregnant patients or nursing mothers has not been established.
n Implementation
MAO inhibitors are given only orally and are well absorbed by this route. The desired antidepressant effect of MAO inhibitors usually occurs within 1 to 4 weeks of drug therapy. If results are not obtained after this time, the patient will not be helped by continuing to take the drug. When improvement is noted during the first 4 weeks of drug therapy, the dosage will likely be reduced gradually over a period of several weeks until an effective maintenance dosage is reached. MAO inhibitors are usually not given in the evening because of their psychomotor stimulating effect, which may produce insomnia.
The maintenance dose of MAO inhibitors can be administered in either single or divided doses. MAO inhibitors should be discontinued at least 2 weeks before elective surgery. If emergency surgery is indicated, doses of narcotics and anesthetics should be reduced. All patients treated on an outpatient basis need to be closely monitored.
Information about MAO inhibitors is provided in Table 16-9.
![]() Table 16-9
Table 16-9
| GENERIC NAME | TRADE NAME | COMMENTS |
| tranylcypromine | Parnate |
Improvement in symptoms usually seen 1-3 wk after therapy is begun. Higher incidence of hypertensive reactions with this drug than with other MAO inhibitors. Used to treat endogenous depression. |
| phenelzine sulfate | Nardil |
For depressed patients clinically described as typical, non- endogenous or neurotic. Use in patients who have failed other drugs. |
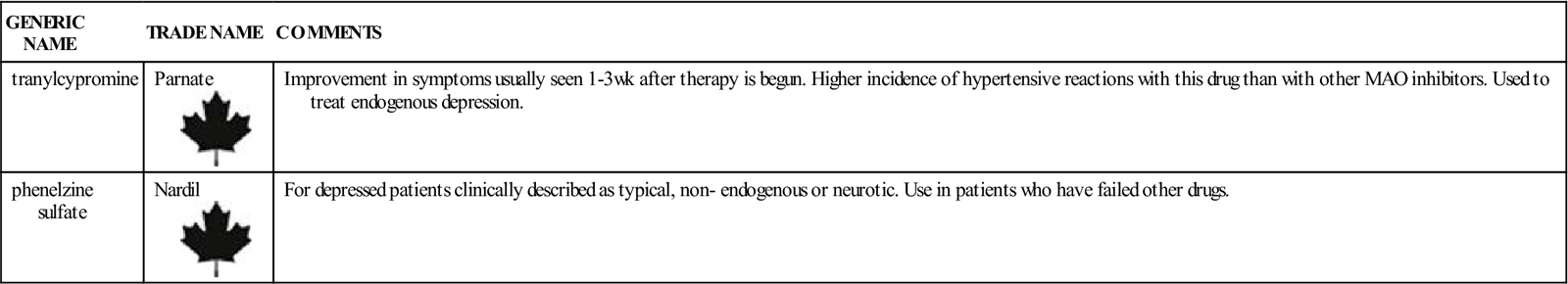
n Evaluation
All patients taking MAO inhibitors must be monitored for symptoms of orthostatic hypotension. If this occurs, the dosage of the drug may need to be reduced or the drug discontinued.
Patients who are agitated or who have schizophrenia may become more hyperactive. Bipolar patients may go into the manic phase of their illness; this is sometimes treated by stopping the drug for a brief period and then starting again at a lower dosage.
The effects of MAO inhibitors continue for approximately 2 weeks after the drug is stopped. Therefore patients who have been taking MAO inhibitors should avoid taking any drugs or eating any foods that are known to interact with MAO inhibitors for this 2-week period.
n Patient and Family Teaching
Tell the patient and family the following:
Selective Serotonin Reuptake Inhibitors, Serotonin/Norepinephrine Reuptake Inhibitors and Other Miscellaneous Antidepressants
Action
Since the beginning of the 1980s, a series of new antidepressant medications have been available. Some are chemically unrelated to one another, but all act in some way to prolong serotonin in the brain. Their differences are often in terms of side effects.
Among the selective SSRIs, several products have become very well known: Their antidepressant action is thought to be linked to their inhibition of CNS neuronal uptake of serotonin. These products are powerful and selective inhibitors of neuronal serotonin reuptake. Other medications have been developed that work by SNRIs or norepinephrine/dopamine reuptake inhibiton (NDRIs). Because these more focused products cause far fewer side effects than other antidepressant medications, they have become extensively used and are considered the drugs of choice in the treatment of depression.
There are also other antidepressant products that have an effect on serotonin uptake but that are chemically unrelated to the SSRIs, but are all tetracyclic compounds. Trazodone (Desyrel) and nefazodone (Serzone) are serotonin 2-agonists/blockers/serotonin reuptake inhibitors (SARIs/SSRIs)—A totally new classes of drugs. Nefazodone (Serzone) inhibits neuronal uptake of serotonin and norepinephrine, but the mechanism for this action is unknown.
Mirtazapine (Remeron) is an α2 noradrenergic antagonist, another new drug class. Tetracyclic compounds enhance central noradrenergic and serotonergic activity through an unknown mechanism. They have different amounts of antagonistic activity toward alpha2 and5-HT2 receptors. These products inhibit the uptake of serotonin at the neuronal synaptosomes in the brain and enhance the behavioral changes caused by serotonin. The action of these drugs is more selective than that of other types of antidepressants. They have less effect on the cardiac conduction system than do tricyclic antidepressants, and they cause almost no CNS stimulation, which occurs frequently with MAO inhibitors.
Uses
SSRI drugs are the drugs of choice for most depressive disorders due to their low adverse effect profile and for short-term treatment (less than 5 weeks) of outpatients with a diagnosis that is listed in the category of major depressive disorders in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders. They have also been used extensively for long-term therapy in patients with dysthymic depressive disorders and minor depressive episodes. Fluoxetine (Prozac) is the only SSRI approved for treating depression in the pediatric population and it is only given to those children older than 8 years of age.
Some of these antidepressant agents are approved to treat specific anxiety and eating disorders, assist in smoking cessation (bupropion [Wellbutrin]), or obcessive compulsive disorders.
Adverse Reactions
Adverse reactions to these drugs in general include dizziness, drowsiness, tachycardia, dysrhythmias, hypertension, hypotension, rash, pruritus, constipation, weight loss, nausea and vomiting, anorexia, weight gain, diarrhea, appetite increase, dyspepsia (stomach discomfort after eating), menstrual complaints, impotence, urinary frequency, dry mouth, headache, excessive sweating, tremor, sedation, insomnia, blurred vision, agitation, confusion, hostility, and disturbed concentration.
In nearly 4% of patients taking fluoxetine (Prozac), a rash develops with accompanying fever, leukocytosis, arthralgia (joint pain), edema, carpal tunnel syndrome, respiratory distress, lymphadenopathy, proteinuria, and mild transaminase elevation.
Trazodone (Desyrel) has also produced early menses, hematuria (blood in the urine), urinary frequency, and weight changes.
Patients who abruptly stop taking the medication may experience a sudden increase in dangerous symptoms. Patients must be taught to follow their health care provider’s directions and gradually decrease the amount of medicine taken if the drug is to be stopped.
Drug Interactions
If bupropion (Wellbutrin) is taken with levodopa, the chance of adverse effects increases. If bupropion is used with carbamazepine (Tegretol), cimetidine, phenobarbital, or phenytoin (Dilantin), the hepatic metabolism of the drugs may be increased. Acute toxicity may develop if bupropion is given with phenelzine (Nardil).
Fluoxetine (Prozac) increases the half-life of some drugs and may displace drugs bound to protein, such as warfarin and digitoxin, or be displaced by them. Concurrent use of trazodone (Desyrel) and antihypertensives can cause hypotension. There are many other isolated drug interactions. Trazodone (Desyrel) may increase the effects of alcohol, barbiturates, and other CNS depressants. The drug should be stopped as long as possible before general anesthesia because interactions are unknown.
Some antidepressants may cause cardiac repolarization problems shown by prolongation of the QT Interval on the electrocardiogram (ECG). These patients are at risk for sudden death. The more drugs the patients take, the more care should be shown to try to prevent drug interactions that might lead to this problem.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including history of hypersensitivity, presence of seizure disorder, current or prior diagnosis of bulimia or anorexia nervosa (these patients tend to have more seizures when receiving bupropion [Wellbutrin]), or recent use of an MAO inhibitor. After stopping MAO inhibitor therapy, the patient should wait at least 14 days before starting bupropion (Wellbutrin).
n Diagnosis
Determine what other problems this patient may be having as a result of depression. Assessment of deficits in nutrition, safety, and knowledge are important. What other problems does this patient have specifically? For a patient who has been taking the medication, side effects such as insomnia, impotence, and taste disorders may make the underlying depression worse. Evaluate the extent of side effects and the impact on the patient’s ability to function.
n Planning
The incidence of seizures in patients taking bupropion (Wellbutrin) is approximately four times greater than that in patients taking other antidepressant medications.
Fluoxetine (Prozac) has a relatively long half-life (2 to 3 days), and problems with liver or renal failure may prolong the drug’s action in the body. There is growing evidence that this product may be useful in treating panic attacks, obsessive-compulsive disorders, and other psychiatric problems.
Dosage levels are individualized based on symptoms. Patients may need to keep a diary or journal to actually realize that they are feeling better. A stable amount of the drug in the blood may not be reached until 4 to 5 weeks after starting therapy. Fluoxetine (Prozac) stays in the body for weeks. This may be important when drug therapy must be stopped.
Trazodone (Desyrel) should not be used while the patient is having electroshock therapy.
n Implementation
Patients on bupropion (Wellbutron) therapy should be watched for worsening of depressive symptoms, agitation, insomnia, and suicide risk. Be alert for seizure activity, because this drug has been linked to a risk for dose-related seizures at levels of more than 450 mg. Bupropion (Wellbutrin) has been known to produce unwanted changes in appetite, weight, and blood pressure (i.e., increase); monitor for these changes.
Additional important information about these medications is summarized in Table 16-10.
![]() Table 16-10
Table 16-10
Selective Serotonin Reuptake Inhibitors and Other Miscellaneous Antidepressants
| GENERIC NAME | TRADE NAME | COMMENTS |
| Selective Serotonin Reuptake Inhibitors | ||
| citalopram | Celexa | For treatment of depression, alcoholism, panic disorder, premenstrual dysphoria, and social phobia. |
| escitalopram | Lexapro | Reassess after 8 wks of treatment. |
| fluoxetine |
Prozac | Full antidepressant effect may not be seen for 4 wk. Lower dosage used in patients with renal or hepatic impairment, patients with multiple diseases or medications, and the elderly. Effective in reducing symptoms of premenstrual syndrome in women, panic attacks, and obsessive-compulsive disorders. |
| fluvoxamine | Luvox CR | |
| paroxetine | Paxil | |
| sertraline | Zoloft | |
| Miscellaneous Antidepressants | ||
| Tetracyclic Compounds | ||
| mirtazapine | Remeron | For treatment of major depressive disorder. |
| trazodone | Desyrel | If drowsiness occurs, a larger dose can be given at bedtime. |
| maprotiline | Maprotiline | For relief of anxiety associated with depression. |
| Unrelated Products | ||
| bupropion |
Wellbutrin | Instituted gradually to avoid producing seizures. May require addition of sedative-hypnotic in first week of therapy. |
| desvenlafaxine | Pristique | Comes as extended release tablet. |
| duloxetine | Cymbalta | May require prolonged duration of therapy. |
| nefazadone | Nefazadone | Has chemical structure unrelated to all other antidepressants. Has potential for serious drug interactions with many other drugs. |
| venlafaxine | Effexor | Take with food. Patients should taper off drug and not stop it suddenly. |
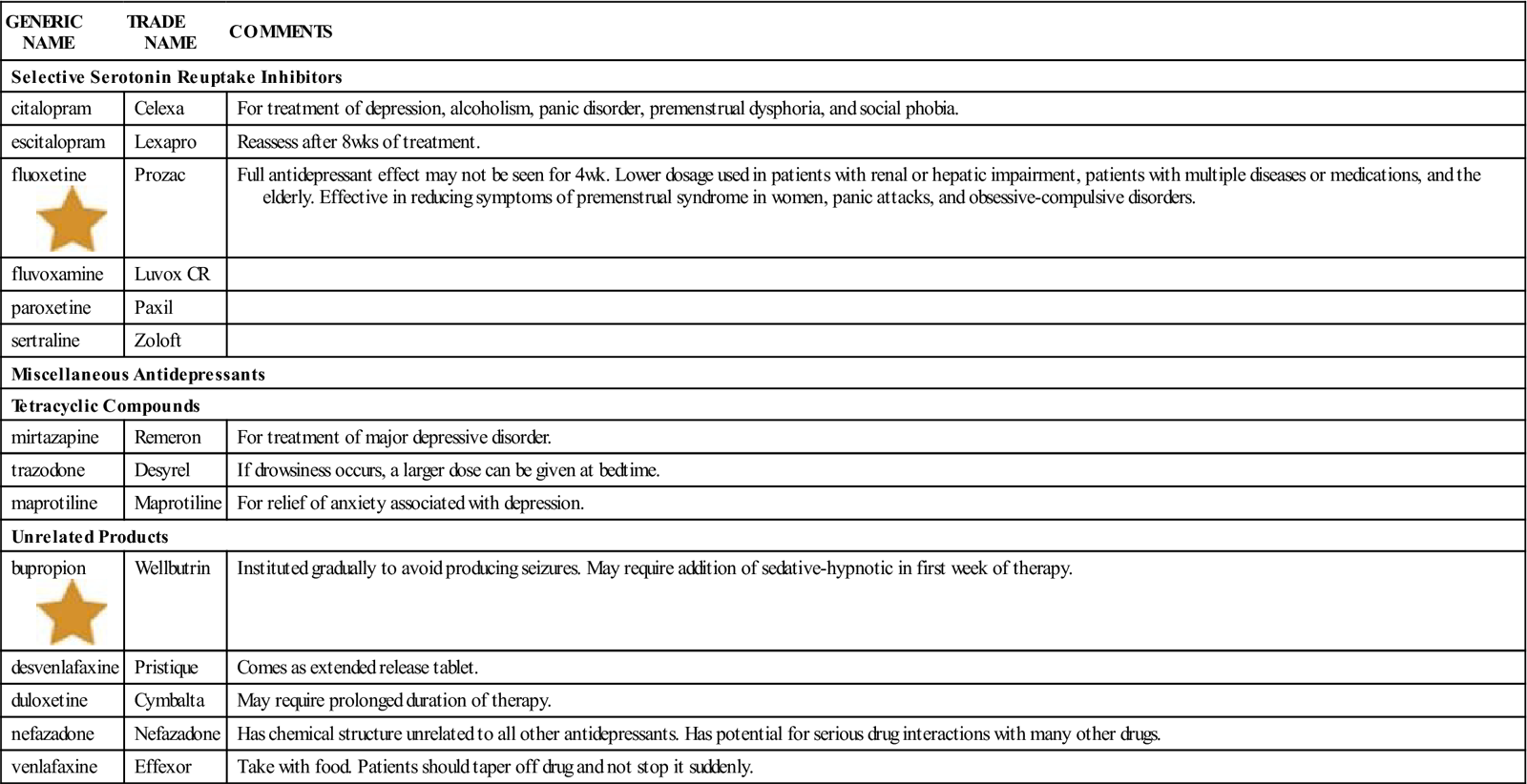
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
The desired antidepressant effect usually begins within 1 to 2 weeks after drug therapy is initiated and reaches its full effect within 4 weeks. The patient’s level of depression should respond with an improvement in symptoms and attitude, and a return to the normal activities of daily living should be possible. Some patients who begin feeling better have enough emotional energy to commit suicide and family or friends should closely monitor patients for this possibility.
n Patient and Family Teaching
Tell the patient and family the following:
 Antipsychotic Drugs
Antipsychotic Drugs
Overview
Severe mental illness such as schizophrenia, psychotic depression, mania, or organic brain syndrome have no identifiable cause and require long term therapy with antipsychotic drugs. These medications are used initially to sedate, or slow the patient down, thereby reducing some of the psychotic symptoms. This allows other therapy to be used. Antipsychotic medications have many side effects and require constant monitoring. Psychotic symptoms may change over time, requiring constant adjustment of medication. Psychotic symptoms, particularly those associated with schizophrenia, are labeled as either positive because they add on to normal behavior (delusions, disorganized thoughts or speech, hallucinations), or negative because they subtract from normal behavior (lack of interest, failure to respond, no motivation, nothing provides pleasure). Monitoring of these symptoms helps in choosing the best medications to give.
Antipsychotic drugs are powerful drugs with significant actions and side effects. They are grouped into three broad categories:
All antipsychotic agents act by blocking the action of dopamine in the brain. Because they are from different chemical groups, however, these drugs work at different sites in the brain and also produce side effects on different body systems. The major categories will be presented separately. The atypical antipsychotics have become the standard of care in the treatment of schizophrenia and associated psychotic disorders and in treating various other psychiatric conditions such as bipolar disorder. They may also be used in treatment of obsessive-compulsive disorder, aggression due to dementia, post-traumatic stress disorder, psychosis in Parkinson’s disease, and borderline personality disorder. Chlorpromazine (Thorazine) is the prototype antipsychotic from which all other antipsychotic potencies are compared.
First Generation or Conventional Antipsychotic Drugs—Phenothiazines and Nonphenothiazines
Action
The conventional phenothiazine antipsychotics first came into the market and, while somewhat effect in treating psychophrenia, had many side effects. It was disappointing for clinicians to find that the nonphenothiazines that were introduced later also had many side effects. They did offer some treatment options for patients.
The three major actions of both the phenothiazine and nonphenothiazines are as follows:
Uses
Conventional antipsychotics such as chlorpromazine (Thorazine), thioridazine (Mellaril), and promazine (Prozine) are used primarily for reducing or relieving the symptoms of acute and chronic psychoses, including schizophrenia, schizoaffective disorders, and involutional psychosis. The nonphenothiazine class thioxanthene is preferred for use in psychotic patients who are withdrawn or are exhibiting retarded behavior. Clinical evidence has shown that patients with certain types of apathetic psychosis respond well to this drug. Haloperidol (Haldol) may be injected and is often used in calming patients with dementia.
Adverse Reactions
Adverse reactions to phenothiazines and nonphenothiazines include severe extrapyramidal symptoms which may not be reversible: psueoparkinsonism, dystonic reactions (severe spasms, particularly of back muscles, tongue and facial muscles), akathiasia (constant pacing and compulsive movements), tardive dyskinesia (bizarre tongue and face mvoements such as lip smacking an chewing movements). Additionally, the drugs may cause, postural hypotension, tachycardia, confusion, drowsiness, hyperactivity, insomnia, amenorrhea, gynecomastia (enlargement of the breasts in men), hyperglycemia (high blood sugar level), hyperreflexia, tardive dyskinesia, blood cell abnormalities, contact dermatitis, photosensitivity, constipation, dry mouth, dyspnea (uncomfortable breathing), incontinence, nasal congestion, opaque deposits on the cornea and lens, and urinary retention. Production of a severe agranulocytosis has prevented Clozapine (Clorazil) from becoming a first line treatment drug.
In general, the nonphenothiazine agents cause less sedation and fewer anticholinergic side effects than phenothiazine products, but cause an equal or even greater incidence of extrapyramidal symptoms. Therapy with these products and other CNS depressants must be carefully watched because of potential additive effects.
Haloperidol (Haldol) produces orthostatic hypotension, drowsiness, tardive dyskinesia, blurred vision, breast engorgement, constipation, decreased libido, dry mouth, impotence, nausea, and vomiting.
Overdosage produces exaggerated CNS depression, coma, or severe hypotension, and extrapyramidal symptoms, seizures, or cardiac dysrhythmias may appear.
Drug Interactions
Phenothiazines taken concurrently with CNS depressants (alcohol, barbiturates, narcotics, and anesthetics) may increase and prolong the effects of either the CNS depressant or the phenothiazine. The effects of MAO inhibitors and TCAs are increased when they are taken at the same time as phenothiazines, and antacids and antidiarrheal drugs reduce the absorption rate. The effects of many other drugs and the results of laboratory tests are altered by phenothiazines and thioxanthenes.
Haloperidol (Haldol) increases the CNS depressant effects of alcohol, barbiturates, opioids, and anesthetics, and may produce severe hypotension when taken with antihypertensive drugs or epinephrine.
Some of these products have been implicated in causing changes in cardiac repolarization as shown by prolongation of the QT interval on the ECG. This problem places the patient at sudden risk. Any patient taking several antidepressant-antipsychotic medications should be closely monitored for any alteration in ECG.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the presence of hypersensitivity to any phenothiazines (because cross-sensitivity occurs); the history of cardiac, respiratory, or blood diseases; current use of other medications; and the possibility of pregnancy. These conditions are either contraindications or precautions to the use of phenothiazines and nonphenothiazines.
The patient may have a history of emotional unrest, agitation, paranoid ideas, hallucinations (visual, auditory, or tactile), delusions, inability to think clearly, severe mood swings, and inability to cope with reality. Patients may or may not talk about paranoid thoughts and often have difficulty paying attention and responding to things going on around them. They may not give appropriate answers to questions, and behavior, dress, and general appearance may not be appropriate.
n Diagnosis
What other needs does this patient have? Safety? Nutrition? Does the patient have a support system of family or friends?
n Planning
Phenothiazines and nonphenothiazines are not recommended for use in pregnant women or nursing mothers.
Patients with severe asthma, emphysema, or acute respiratory infections (especially children) may have slowing of respiration as a result of the CNS depressant effects of phenothiazines. Phenothiazines may also depress the cough reflex, putting a patient who is vomiting in danger of aspirating.
n Implementation
Phenothiazines can be taken either orally or parenterally. The oral form is fairly well absorbed, but the absorption rate will be slowed if the drug is taken with antacids or antidiarrheal agents.
Most nonphenothiazines are only available orally.
Stomach upset from the oral form of phenothiazines can be reduced or avoided by taking the drug with bland food or 8 ounces of water. Additional information about these medications is listed in Table 16-11.
![]() Table 16-11
Table 16-11
| GENERIC NAME | TRADE NAME | COMMENTS |
| First Generation—Conventional Antipsychotics | ||
| Phenothiazines and Phenothiazine-Type Drugs | ||
| Aliphatic Phenothiazines | ||
| chlorpromazine | Thorazine | Traditional phenothiazine product, popular and inexpensive. Used in psychotic disorders to control the manic phase of manic-depressive reactions, preoperatively for restlessness, to treat behavioral problems of children who are combative, or for hyperactive children with excessive motor activity. |
| promazine | Promazine | Used primarily to manage psychotic disorders. Oral medication usually preferred. |
| Piperazine Phenothiazines | ||
| fluphenazine | Prolixin | Also used for dementia; comes IM or SQ |
| perphenazine | Trilifon | Also used for dementia; for nausea in IM and IV |
| trifluoperazine | Stelazine | Also for dementia; available only IM |
| prochlorperazine | Compazine | Also as antiemetics. Comes in a variety of delivery systems. |
| Piperdine Phenothiazines | ||
| mesoridazine | Serentil | Strong sedative. Also used for dementia, anxiety, hyperactivity, and alcohol dependence |
| thiordazine | Mellaril | Strong sedative; used for moderate to severe depression |
| First Generation Conventional Nonphenothiazine Antipsychotic Medications | ||
| Thioxanthene Derivative | ||
| thiothixene | Navane |
Monitor the patient for early signs of tardive dyskinesia and jerky movements, particularly of the hands. |
| Phenylbutylpiperadines | ||
| haloperidol | Haldol | Used to calm demented or manic patients |
| Miscellaneous Conventional Nonphenothiazines | ||
| chloroprothixene | Taractan | Strong sedative effects; available in IV form |
| loxapine succinate | Loxitane | Also used for dementia |
| molindone | Mobane | Has either sedative or stimulating effect, insomnia |
| primozide | Orap | Anticholinergic effects increased; Tardive dyskinesia if abruptly stopped. Also used for Tourette’s syndrome |
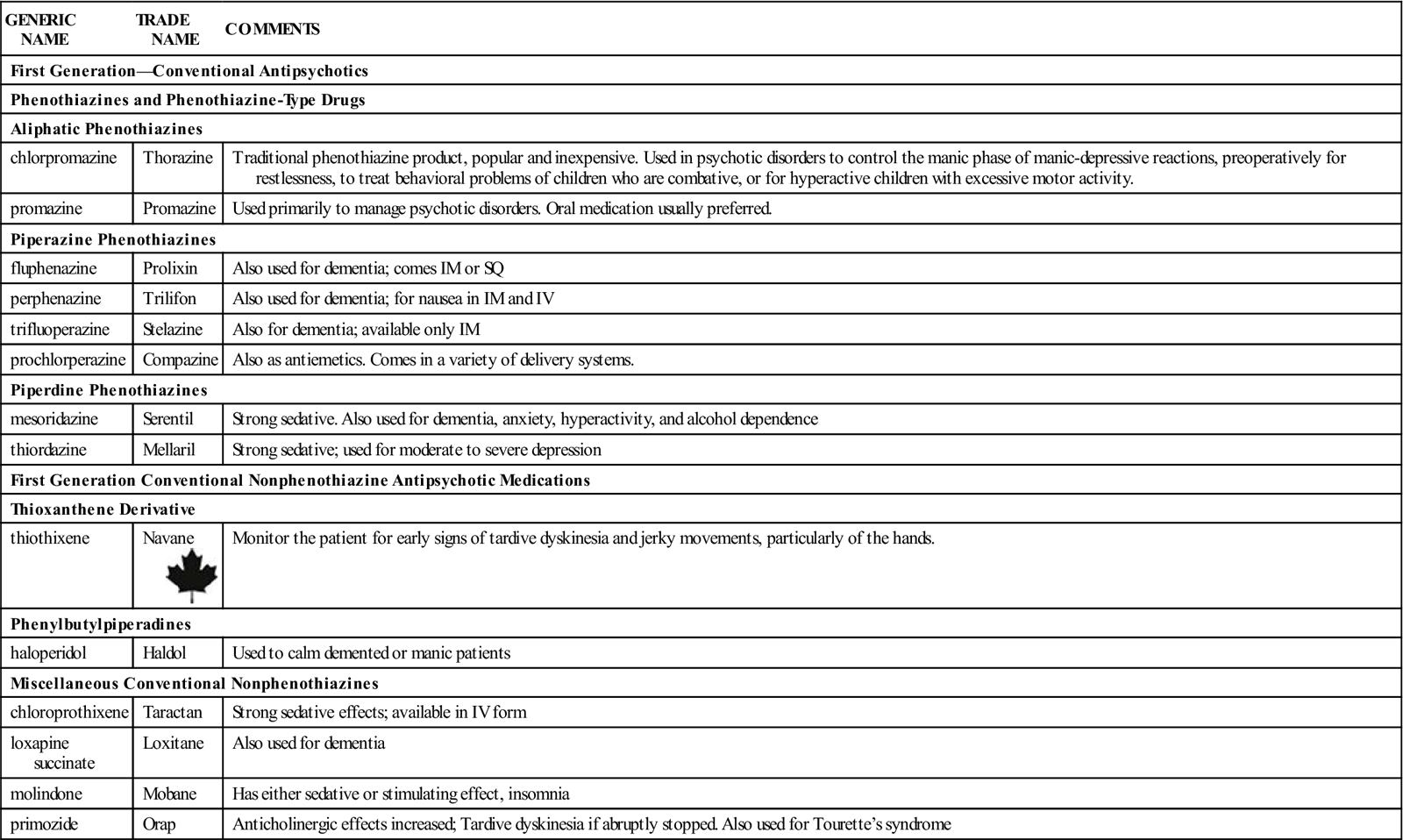
n Evaluation
The desired antipsychotic effects of phenothiazines may take several weeks to appear after therapy is started. The beginning dose should be the lowest recommended amount, according to the individual’s tolerance and the severity of psychosis, until the psychotic symptoms are controlled. The dosage of phenothiazines that controls the patient’s symptoms will likely be maintained for 2 to 3 weeks and then gradually reduced until the lowest effective maintenance dosage is reached. Phenothiazines given in large doses or for a long time should be discontinued by gradual reduction over several weeks to avoid symptoms of dyskinesia (difficulty in movements of the body), nausea, vomiting, dizziness, and trembling.
The patient should have a complete eye examination by a specialist, including inspection of the internal structures and the lens, to establish baseline data.
n Patient and Family Teaching
Tell the patient and family the following:
Second Generation or Atypical Antipsychotics
A variety of chemically unrelated products have more recently come on the market to help in treating psychotic patients. The newest addition to this category is a new class of medication called dopamine system stabilizers.
Action
The mechanism of action for these products is often not precisely understood but they are thought to act by blocking several different receptor types in the brain. Aripiprazole (Abilify) is the new dopamine system stabilizer. It is thought to be a partial dopamine agonist (whereas other antipsychotic agents are full dopamine agonists) and thus has a targeted mechanism of action.
Uses
These atypical antipsychotic drugs have a broad spectrum of action, controlling both positive and negative symptoms of schizophrenia and have now become the drugs of choice for treating psychoses. These drugs are now used primarily in the treatment of schizophrenia.
The new dopamine system stabilizer apripiprazole (Abilify) shows both negative and positive symptoms of schizophrenia are reduced by this drug. Motor side effects appear to be less of a problem than with other antipsychotics with low incidence of extrapyramidal effects. Overall efficacy appears to be similar to haloperidol (Haldol) and risperidone (Risperdal) in schizophrenia. It has been approved for use in schizophrenia and as adjunctive treatment in major depressive disorder in adults, and in treatment of acute manic or mixed episodes of bipolar I disorder. It has been approved by the Food and Drug Administration as an adjunctive therapy to lithium or valproate (Depakote) in bipolar I disorder and for the treatment of irritability associated with autistic disorder. Some indications are approved for children and adolescents; some indications are reserved for adults.
Adverse Reactions
These drugs do not cause extrapyramidal side effects when taken at therapeutic doses. Although there are fewer side effects with these drugs, most cause weight gain and may cause obesity. Some of these agents may alter glucose metabolism and increase the risk for development of type 2 diabetes. Risperidone (Risperdal) may cause decreased sex drive in men and women and menstrual disorders and osteoporosis in women.
The antipsychotic medications in general have been found to cause changes in cardiac repolarization as measured by a prolonged QT interval on the ECG. This places the patient at risk for sudden death. These patients should have their ECGs closely monitored. Some patients know that they have a gene that increases their risk for LQT syndrome and there are some drugs that these patients should not be given. When studying about drugs or reading package inserts, the nurse should be aware that some products are found to prolong the QT interval. A complete list of those drugs which these patients should not be prescribed may be found at www.sads.org/living-with-sads/Drugs-to-Avoid.
Aripiprazole has fewer side effects than many other current antipsychotics. Common effects include vomiting, somnolence, and tremor. Overdoses may produce acidosis, aggression, atrial fibrillation, bradycardia, coma, confusional state, convulsions, depressed level of consciousness, hypertension, hypotension, lathery, ECG disturbances, respiratory arrest, status epilepticus. Patients may experience increase in anxiety and headache.
Some of the major features of these products are briefly presented in Table 16-12.
Table 16-12![]()
Second Generation or Atyical Antipsychotic Medications
| DRUG | ACTION | ADVERSE REACTIONS | DRUG INTERACTIONS |
| Nonphenothiazine Antipsychotic Medications | |||
| clozapine (Clozaril) |
Increased affinity for 5-HT receptors; acts on several neurotransmitters, including antagonism of some dopamine receptors. | Life-threatening agranulocytosis (very low number of white blood cells) | Increases effect of digoxin and warfarin; may decrease effects of other highly protein-bound drugs. |
| olanzapine (Zyprexa) | Increased affinity for 5-HT receptors; acts on several neurotransmitters, including antagonism of some dopamine receptors. | CNS stimulation | Carbamazepine decreases concentrations; interferes with cytochrome P-450 system. |
| quetiapine (Seroquel) | Increased affinity for 5-HT receptors; acts on several neurotransmitters, including antagonism of some dopamine receptors. | May produce cataracts with long-term use; may increase cholesterol level. Lengthens ECG Q-T interval in some patients. | Increased levels when given with phenytoin; cimetidine decreases clearance and thus increases serum level. |
| risperidone (Risperdal) | Increased affinity for 5-HT receptors; acts on several neurotransmitters, including antagonism of some dopamine receptors. | Lengthens ECG Q-T interval in some patients; elevated prolactin level; causes agitation, anxiety, headache, insomnia, constipation, dyspepsia, and rhinitis. | Use with clozapine decreases clearance of risperidone. |
| ziprasidone (Geodon) | Acts on several neurotransmitters. | Lengthens ECG Q-T interval in some patients and may produce lethal dysrhythmias. | Take medication with food. |
| Dopamine System Stabilizers | |||
| Aripiprazole (Abilify) | Partial dopamine agonist | Many side effects including lengthening of ECG QT-interval; increased risk of suicide. | Patient should not stop taking suddenly. Watch for development of high blood glucose, cardiac problems, changes in consciousness or neurologic function, and weight. |
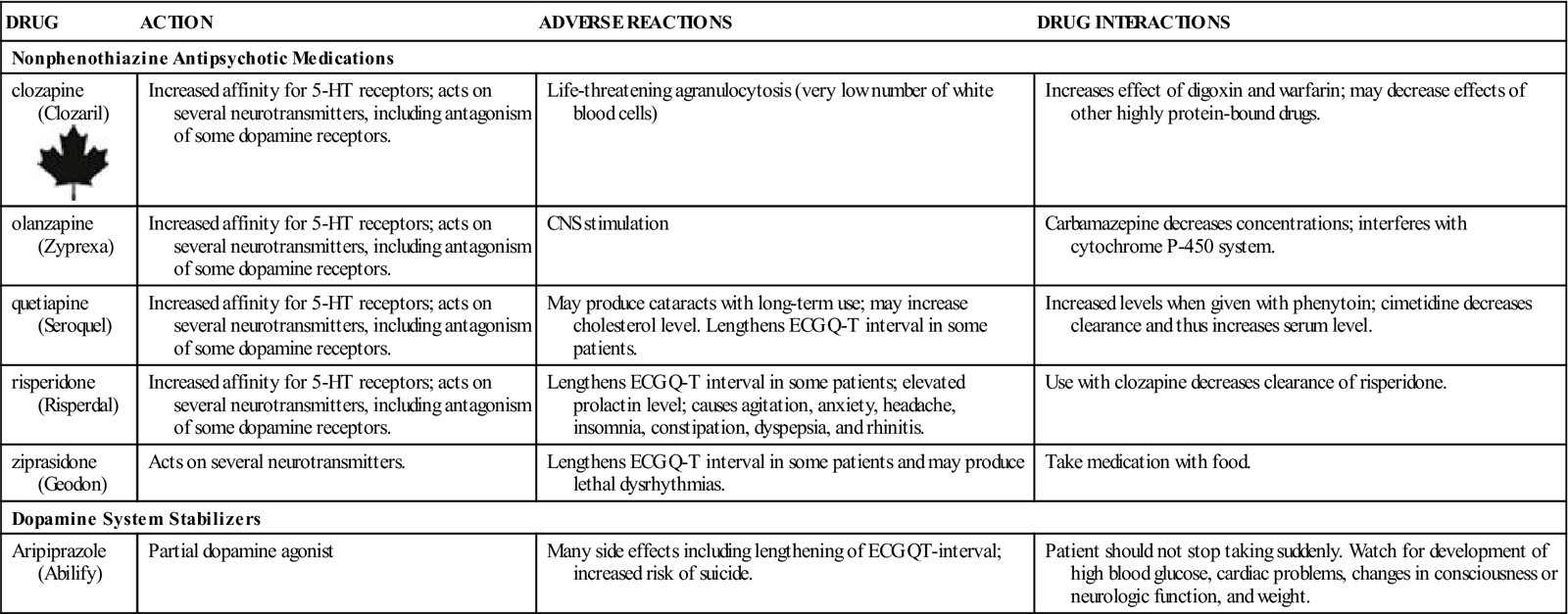
5-HT, 5-Hydroxytriptamine; CNS, central nervous system; ECG, electrocardiogram.
Drug Interactions
Many of these drugs have the same interactions as the phenothiazine drugs. One of the most widely used drugs, haloperidol (Haldol) interacts with many drugs. It may block the action of centrally acting antihypertensives. It’s action may be decreased by aluminum- and magnesium-containing antacids, levodopa, lithium, phenobarbital, phenytoin, rifampin, and beta blockers.
Aripiprazole is metabolized by liver enzymes and so has the potential to interact with many different types of drugs. The patient should be monitored very closely when aripiprazole is taken with other drugs because the action of aripiprazole may be increased or decreased or the other drug absorption may be increased or decreased.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Care should be taken to collect a detailed psychiatric history and a thorough drug history about past and current drugs and the patient’s reaction to taking them.
n Diagnosis
Does the patient have other problems that might interfere with taking this drug such as dehydration, confusion? When these drugs are used in psychotic patients, patient symptoms may become worse, with development of agitation, irritability, unusual changes in behavior, or suicidality.
n Planning
Use with caution in patients with preexisting hypotension or cerebrovascular disease, cardiac disease, heart failure, history of heart attack, angina, and some arrhythmias. The patient should have a baseline ECG taken before beginning this medication. Because of high risk of suicide in some of these patients, prescriptions should be written for the smallest quantity of tablets possible to reduce the risk of overdose. Safety of the drug during pregnancy and breastfeeding has not been established. Patient should have baseline weight and blood sugar levels recorded to use in following up response to the drug.
n Implementation
Encourage the patient and family to watch for any changes in behavior or symptoms and report them promptly. These drugs should not be stopped abruptly. Patients should avoid extremes of cold or heat, as the drug may affect the area of the brain responsible for temperature regulation and patients could develop heat stroke.
n Evaluation
High blood sugars and seizures have both been seen in patients who take these medications. Drowsiness has also been a common problem and may interfere with driving or operating machinery or other tasks that require mental alertness. This drug has a black box warning regarding increased risk of suicide, particularly in adolescents. Behavior should be closely monitored and any suspicious behavior reported.
Antimanic Mood Stabilizers and CNS and Non-CNS Stimulants
Mood stabilizers are used in patients with manic-depressive disorder or psychosis to limit the extremes of both the depression and manic episodes and also to decrease the mood switches back and forth. These drugs seem to have a calming effect on the brain. But sometimes patients have a need for CNS stimulation. This is most often seen in patients with attention-deficit/hyperactivity disorder (ADHD). The drugs in these two categories have different actions and uses, but both act to modify the brain action so patient behavior is more normal.
Antimanic Mood Stabilizers
Action
Lithium is the primary drug used to treat patients in manic states. Some other antiseizure drugs are also used for mood stabilization. The exact mechanism of lithium action is not known. The mood-stabilizing effect of the drug may be attributed to its ability to alter sodium transport at the nerve endings, inhibit cyclic AMP formation in nerve cells, and enhance the uptake of serotonin and norepinephrine by nerve cells, thus increasing the inactivation of these neurotransmitters. It has no sedative, depressant, or euphoric actions, making it unique from all other psychiatric drugs.
Uses
Lithium is specifically used for patients with bipolar disorder (manic-depressive psychosis) who are in an acute manic phase. It also may be used to prevent recurrent episodes of mania in the bipolar patient.
Adverse Reactions
Adverse reactions to lithium include dysrhythmias, hypotension, ataxia, coma, dizziness, drowsiness, motor retardation, restlessness, slurred speech, tinnitus (ringing in the ears), pruritus, rash, abdominal pain, anorexia, diarrhea, vomiting, urinary incontinence or retention, polyuria (excretion of a large amount of urine), albuminuria, blurred vision, hyperglycemia, hypothyroidism, leukocytosis, and weight gain.
Overdosage may produce toxicity which will present as diarrhea, vomiting, muscle weakness, drowsiness, and ataxia.
Drug Interactions
Use of lithium with diuretics can lead to lithium toxicity. There are many significant drug interactions with various medications. No other medication should be taken by the patient without the knowledge and approval of the health care provider.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the presence of hypersensitivity, underlying disease, the possibility of pregnancy, and other medications being used. These conditions may be contraindications or precautions to the use of lithium.
The patient may have a history of excessive talkativeness, restlessness, hyperactivity, aggressiveness, and perhaps ideas of being very important, talented, or powerful.
n Diagnosis
What other problems does this patient have that might influence the effectiveness of the medication? If the patient becomes dehydrated, grows excitable and forgets to take the medication on a regular basis, or dislikes the effects of lithium and believes it is not needed, this may result in significant treatment problems.
n Planning
Lithium is not safe for use in pregnant patients and breastfeeding mothers. If a patient receiving lithium becomes pregnant, especially during the first trimester, the drug needs to be stopped because it may cause birth defects.
Older adult patients are often more sensitive to lithium toxicity. It is important to start these patients on lower doses and monitor the therapeutic and adverse effects closely while increasing dosage.
n Implementation
Make sure the patient has adequate hydration (enough fluids) and that electrolytes are balanced during lithium therapy.
Table 16-13 summarizes the important information the nurse needs to know about lithium.
![]() Table 16-13
Table 16-13
| GENERIC NAME | TRADE NAME | COMMENTS |
| lithium | Carbolith |
Lithium administered orally is rapidly absorbed in the GI tract. The desired effect of lithium may take 1 to several weeks to occur. Lithium is excreted by the kidneys, with a half-life of approximately 24 hr in a healthy adult, but in the older adult patient, half-life may be increased to 36 hr; therefore lower dosages are indicated for this group. Lithium excretion is inhibited in the presence of low serum sodium levels. The therapeutic serum level of lithium is 1-1.5 mEq/L. Lithium is not recommended for children younger than 12 years of age. Used to treat acute phase of mania and for prophylaxis. |
| Eskalith | ||
| Lithane |
||
| Lithonate | ||
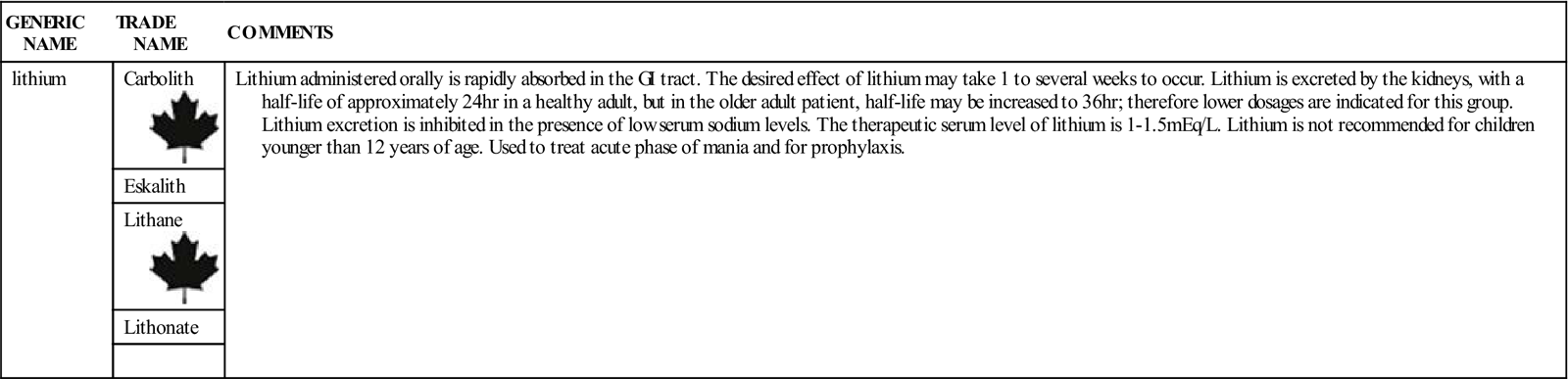
n Evaluation
The therapeutic blood level of lithium is relatively close to the toxic level, so the serum lithium level must be monitored on a regular basis. Blood should be drawn 12 hours after the dose of lithium is given. Monitoring should be carried out every few days during the initial therapy and then at least every 2 months after the patient is stabilized. The therapeutic serum lithium level is 1 to 1.5 mEq/L in most laboratories. At each patient visit, observe for therapeutic effects and monitor the patient’s mental and emotional status.
Lithium is better tolerated when the patient is in an acute manic stage than in a stage in which symptoms of mania have decreased. The dosage of lithium may have to be adjusted according to the patient’s symptoms and the lithium blood serum levels.
Patients who develop diarrhea or become ill and do not eat are at increased risk of toxicity, and their condition should be followed closely.
n Patient and Family Teaching
CNS And Non-CNS Stimulants
Over the years an increasingly large number of children who have trouble completing tasks and paying attention have been identified with ADHD. They have increased motor activity, which gets children in trouble when they cannot sit still in school, cannot stay on task, talk constantly, interrupt others, and are always “wiggling, poking, and moving”. There may be aggressive behavior, impulsivity, and anxiety, all of which may make it difficult for these children to learn or creates behavior problems when they can’t interact with other children in a normal way. These children are easily distracted, have trouble remembering, do not follow instructions properly, cannot complete long or complex tasks, and may have sleep disturbances. It may take several years for some children to be accurately diagnosed—usually girls are diagnosed later than boys.
Some adults now recognize that attention deficit disorder (ADD) is a problem that they have had since childhood and are seeking treatment for the same problems. In adults, the primary symptoms include restlessness, depression, anxiety, or even manic like behavior. They may have mood swings that are similar to bipolar depression disorder. All of these symptoms have usually contributed to struggles in educational, employment, and social situations that have created poor self-esteem. This may in turn lead to introverted behaviors causing people to pull away and isolate themselves from others.
Action
The cause of ADD or ADHD is not clearly identified, so treatment is been difficult. It is now believed that the hyperactivity may be related to a deficit or dysfunction of neurotransmitters in the brain—particularly dopamine, norepinephrine, and serotonin in the reticular activating system of the brain. The drugs used to treat ADHD are mostly CNS stimulants that increase activity in specific areas of the brain to heighten alertness and help them focus better. The drugs do this by increasing norepinephrine release in some pathways of the reticular activating system. They also directly stimulate the release of dopamine in areas of the brain responsible for concentration. These drugs have some potential for addiction and so most are classified as Schedule II drugs.
Another non-CNS stimulant drug, atomoxetine (Strattera) is approved for treating ADHD. Although the exact mechanism of action is not clear, it is classed as a selective norepinephrine reuptake inhibitor—thus it is not an addictive or Schedule II drug.
The two categories of drug therapy appear to be equivalent in efficacy but patients may respond better to one than the other.
Uses
These drugs are limited to treatment of ADD and ADHD.
Adverse Reactions
These CNS stimulants are associated with a wide variety of symptoms that make some children reluctant to take them. These include anorexia, abdominal pain, depression, dizziness, nausea, nervousness, and weight loss. Common adverse effects of atomoxetine includes headache, cough, decreased appetite, upper abdominal pain, and insomnia.
Drug Interactions
These drugs interact with many other drugs and may decrease the effectiveness of anticoagulants and anticonvulsants. Use with some other drugs may increase the adverse effects. CNS stimulants should not be given with MAO inhibitors.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the presence behavioral or social problems related to ADHD. The patient may have a history of excessive talkativeness, restlessness, hyperactivity, and aggressiveness.
n Diagnosis
What other problems does this patient have that might influence the effectiveness of the medication? Does the patient have a support system to help him or her take the medicine—particularly if the patient is a child?
n Planning
Some patients experience anorexia. While dosing depends on specific agents, drugs should be given after meals to reduce the appetite suppressant symptoms. Insomnia is a common side effect of CNS stimulants, as well as of ADHD itself. Drugs should be taken at least 6 hours before bedtime to reduce the risk of sleep problems. These drugs are pregnancy category C drugs and Schedule II controlled substances. Is there any suggestion of previous drug addiction? Because this drug has the potential for addiction or patients may develop tolerance to the drug when used for a long time, periodic drug-free “holidays” are recommended to help clear the patient’s system of the drug. Due to high potential for abuse, parents should keep these drugs in a locked cabinet to prevent the patient from taking the drugs to give to or sell to people at school.
Some children like taking the drugs because they feel more in control of themselves. They may even remind their parents when they need to take the drugs. This feeling of control might be encouraging to children.
n Implementation
Avoid taking these drugs with caffeine products, which may produce increased stimulation.
These drugs must be taken on a regular basis. They may also require that the patient take them for several months before an adequate evaluation can be made about the adequacy of their effects. Thus patients should be encouraged to keep regular appointments for drug evaluation.
Table 16-14 summarizes the important information needed to know about drugs for ADHD.
![]() Table 16-14
Table 16-14
| GENERIC NAME | TRADE NAME | COMMENTS* |
| CNS Stimulants | ||
| d- and l-amphetamine racemic mixture | Adderall | High potential for abuse. Used for narcolepsy (daytime sleep disorder). |
| dextroamphetamine | Dexedrine | Used only for short-term treatment. Produces severe anorexia and insomnia. May prolong QT interval on ECG. |
| methamphetamine | Desoxyn | Commonly abused. |
| methylphenidate | Ritalin | Controls attention deficit better than hyperactivity. Most widely used drug for ADHD. |
| pemoline | Cylert | Used with other drugs rather than alone. |
| Non-CNS Stimulants | ||
| atomoxetine | Strattera | Inhibits reuptake of norepinephrine. |
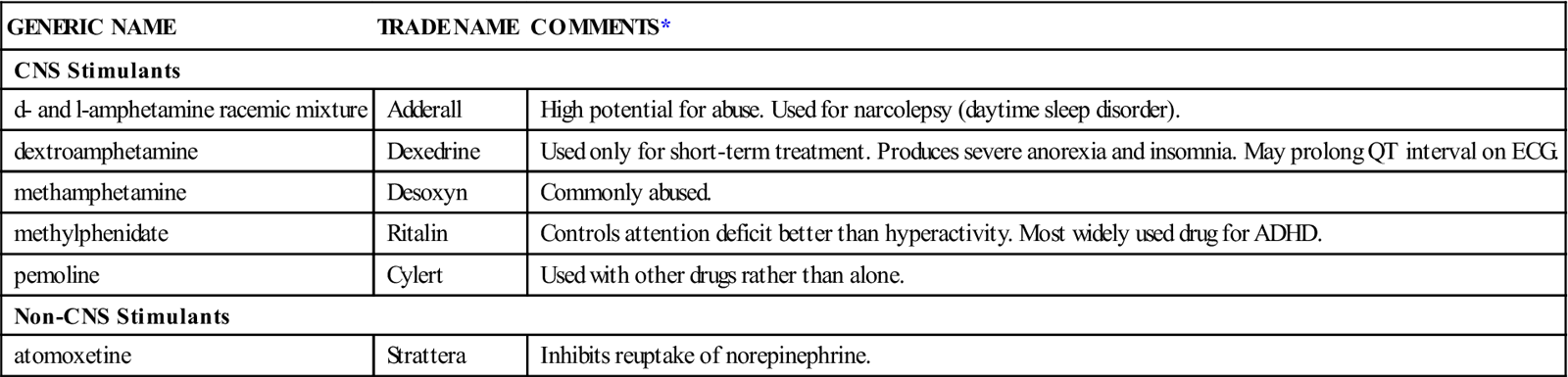
ADHD, Attention-deficit/hyperactivity disorder; CNS, central nervous system.
*Many of these drugs have not been approved for use in children younger than 3 or 6 years old. Consult prescribing information for safety recommendations.
n Evaluation
Changes in dosages are usually based on long-term changes in patient behavior. CNS stimulants may increase blood pressure and this should be monitored regularly. Height and weight should be monitored in children with long-term therapy because of the potential for changes in body metabolism.
n Patient and Family Teaching
Tell the patient and family the following:
Sedative-Hypnotic Medications
Overview
Sedatives help calm and reduce anxiety in a patient. Hypnotics induce drowsiness and promote both sleep and an inability to remember. Both medications are often used in the hospital to help patients relax and produce sleep before anesthesia or medical testing procedures such as EEG. They are also used to treat patients with insomnia (inability to sleep) caused by mental and physical stress.
Sleep is a normal cyclic process that involves varying levels of unconsciousness from which a patient may be aroused. Normal sleep produces relaxation and relief from stress. Although individual patterns vary, each time a person sleeps, four stages occur in a cycle for varying lengths of time. Stages I and II are very light stages of sleep, during which the person may be easily aroused. Stage III is a transition to stage IV, the period of deepest sleep in which basic vital signs slow and the body totally relaxes. It is this period of sleep that makes people feel very refreshed. Approximately every 90 minutes, a period of body arousal is reached, which is often superimposed on stage I or stage II of sleep. This is called paradoxical sleep because instead of relaxing, the body is more active. It is also called REM time because dreaming is common, as demonstrated by rapid eye movements (REM). This is an important part of sleeping, when the unconscious mind works out anxieties and tensions. When people do not have enough REM time each night, they feel anxious and tired.
Action
At times, people may be unable to sleep because of stresses or anxiety. Difficulty falling asleep is termed initial insomnia. The inability to stay asleep is termed intermittent insomnia, and terminal insomnia refers to early awakening with an inability to return to sleep. Terminal insomnia is often associated with depression.
If warm baths, warm drinks, appropriate temperature, and bedding changes do not help the patient relax, a medication may be prescribed on a short-term basis. A sedative agent is a medication that relaxes the patient and so may lead to sleep. A hypnotic agent actually induces drowsiness and promotes sleep in the patient. Whether a medication acts as a sedative or a hypnotic is often determined not by the drug, but by the dosage used, with smaller dosages producing sedative effects and larger dosages producing hypnotic effects.
The ideal medication would reproduce the normal sleep pattern for the patient; the patient would sleep an appropriate length of time, have no side or adverse effects, and wake up feeling rested and relaxed with no risk of developing drug dependency. Unfortunately, no ideal medication exists.
Postmedication “hangover” from reduced REM time often leads the patient to feel they haven’t slept “well” and may increase their desire for more medicine so that the patient may have a refreshing sleep. This pattern may result in dependency or abuse.
Once a patient has taken sedative-hypnotics, the normal sleep patterns may not return for several weeks. During that time, an increased period of REM will be seen, as if the body is trying to “catch up” for missed time. This may produce long, vivid, or frightening dreams.
Uses
Barbiturates are CNS depressants used for a variety of medical problems. All barbiturates act primarily on the brainstem reticular formation, reducing nerve impulses to the cerebral cortex. Barbiturates also depress the respiratory system and the activity of nerves and muscle (smooth, skeletal, and cardiac), thus producing relaxation and sleep.
Barbiturates are used for short-term treatment of anxiety, agitation, and insomnia caused by transient psychosocial stresses. They are also prescribed at times when rest is mandatory, such as before surgery. Large doses of short-acting barbiturates can produce surgical anesthesia (see the third section of this chapter).
The main action of benzodiazepines is CNS depression. Although the exact mechanism is not known, they are thought to act on the hypothalamus and limbic system of the brain, decreasing the vasopressor response and increasing the arousal threshold. They are used as hypnotic agents to treat insomnia. The therapeutic objective is to prevent insomnia and restore normal sleep patterns. Benzodiazepines are used in patients with acute or chronic medical problems who require restful sleep or sedation (see the third section of this chapter for more detail).
The nonbarbiturate-nonbenzodiazepine sedative-hypnotics include a variety of chemically unrelated medications, as well as the GABA receptor agonists such as eszopiclone (Lunesta), zolpidem (Ambien), and zalepion (Sonata). All produce some effects on REM sleep, and most have a potential for tolerance and habituation and so are schedule IV drugs. Many may produce rebound REM. Ramelteon (Rozerem) is a little different in that it stimulates melatonin, the body’s normal chemical to produce sleep, so it has no addictive properties.
Adverse Reactions
Nonbarbiturate-nonbenzodiazepine sedative-hypnotics may produce drowsiness, decreased emotional reaction, dullness, distortion of mood, impaired coordination, hypersensitivity, lethargy, headache, muscle or joint pain, and mental depression. A feeling of “hangover” commonly occurs with their use.
Drug Interactions
Nonbarbiturate-nonbenzodiazepine sedative-hypnotics increase the sedative effects of CNS depressants, including sleeping aids, analgesics, anesthetics, tranquilizers, alcohol, and narcotics. Chloral hydrate may increase the anticoagulant effects of warfarin.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including any medications the patient may be taking that may produce drug interactions, other barbiturates the patient is taking (sometimes these are present in bronchodilators or antispasmodics), response to barbiturates taken in the past, or hypersensitivity. Sedative-hypnotics are not considered safe in pregnancy. Determine whether there are any underlying diseases that would represent contraindications to the use of sedative-hypnotics. The Complementary and Alternative Therapies box summarizes herbal preparations patients may be using to induce sleep and their potential to interact with other drugs.
n Diagnosis
What are the underlying problems that require use of a sedative? Does the patient have physical or emotional concerns that could be the cause of these problems?
n Planning
In general, if sedative-hypnotics are used for more than 1 week, they may cause further disturbances in the sleep cycle and rebound insomnia. Hypothermia may occur with the use of barbiturates. Alcohol can increase the sedation produced by these drugs and depress vital brain functions.
Flurazepam (Dalmane) is increasingly effective on the second or third night of consecutive use. For one to two nights after the drug is stopped, both the amount of time before the patient falls asleep and the total awake time may still be decreased.
Barbiturates and benzodiazepines are Schedule IV controlled substances. The patient may develop dependence if these drugs are used indiscriminately, and abrupt withdrawal is dangerous.
n Implementation
I general, sedative-hypnotics should be given 15 to 30 minutes before bedtime. Table 16-15 summarizes important information regarding benzodiazepine sedative-hypnotics.
![]() Table 16-15
Table 16-15
Benzodiazepine Sedative-Hypnotic Medications
| GENERIC NAME | TRADE NAME | COMMENTS |
| estazolam | Intermediate-acting oral benzodiazepine. Similar to flurazepam, but has fewer side effects. | |
| flurazepam | Dalmane | Flurazepam can be used for a longer time (effective for 28 nights) and has less REM rebound than some other hypnotics. Markedly suppresses stage IV, increases stage II sleep. Hypnotic. Less likely to cause rebound insomnia and tolerance than other drugs. |
| lorazepam | Ativan | This antianxiety agent is generally used for mild or transient situational stress. It is used parenterally as a preanesthetic medication. |
| Mild anxiety or insomnia, preanesthesia medication, and sedation. | ||
| quazepam | Doral | |
| temazepam | Restoril | Induces sleep in 20-40 min. |
| Hypnotic: Give PO before bedtime; in elderly or debilitated patients lower dosage is adequate. | ||
| triazolam | Halcion | Used primarily for short-term treatment of insomnia or early morning awakening. |
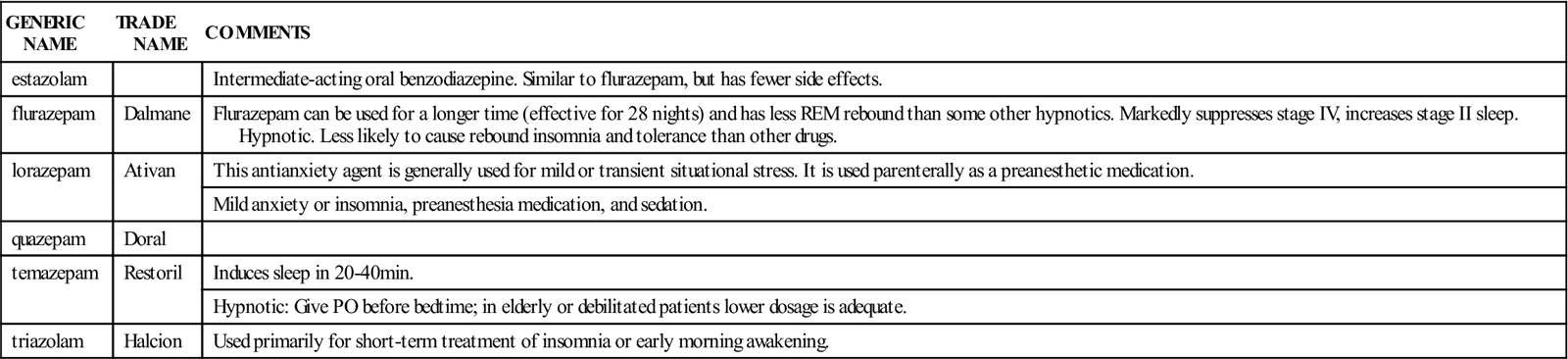
Use great caution when parenterally administering barbiturates to avoid intraarterial injection or extravasation, because serious ischemia or gangrene could result. Barbiturates may worsen a patient’s pain.
Geriatric or debilitated patients should receive lower-than-recommended dosages of barbiturates.
All barbiturates exhibit the same sedative-hypnotic effect, but they differ in time of onset, duration, and potency. Onset and duration are determined by the lipid solubility of the particular drug. Therapy typically begins with the lowest possible effective dose and is adjusted upward according to the individual patient’s response. Patients given barbiturates should be closely monitored for untoward effects. Table 16-16 presents a comparison of different barbiturates used for sedation and hypnosis. As these drugs produce respiratory depression, benzodiazepines are usually preferred.
![]() Table 16-16
Table 16-16
Barbiturate Sedative-Hypnotic Medications*
| DRUG | ONSET OF ACTION (MIN) | DURATION (HOURS) |
| Long-Acting | ||
| phenobarbital (Barbital) |
60 | 10-16 |
| Intermediate-Acting | ||
| butabarbital (Butisol) | 30 | 6-8 |
| Short-Acting | ||
| pentobarbital (Nembutal) | 30 | 3-6 |
| secobarbital (Seconal) | 15-30 | 3-6 |
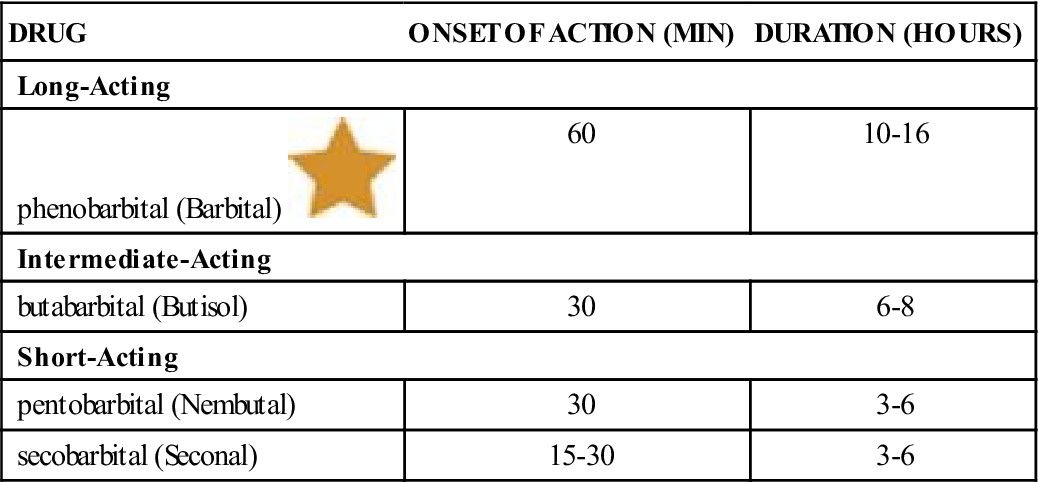
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
There are a variety of other drugs whose primary use may be for other indications, but which also have sedative-hypnotic effects and may be useful in selected situations. Table 16-17 summarizes the nonbarbiturate-nonbenzodiazepine sedative-hypnotics.
![]() Table 16-17
Table 16-17
Non-Benzodiazepine Non-Barbiturate Sedative-Hypnotic Medications*
| GENERIC NAME | TRADE NAME | COMMENTS |
| Chloral Derivatives | ||
| chloral hydrate | Aquachloral | Effective in 30-60 min and lasts 4-8 hr. Has a very disagreeable taste and causes gastric irritation; should be taken after meals; elixir may be taken in water, juice, or soda. |
| Miscellaneous | ||
| zolpidem | Ambien | Approved for short-term use only. |
| eszopiclone | Lunesta | Approved for short term use only. |
| ramelteon | Rozerem | Avoid taking medication after high-fat meal. |
| zaleplon | Sonata | Do not take for longer than 7 to 10 days. |
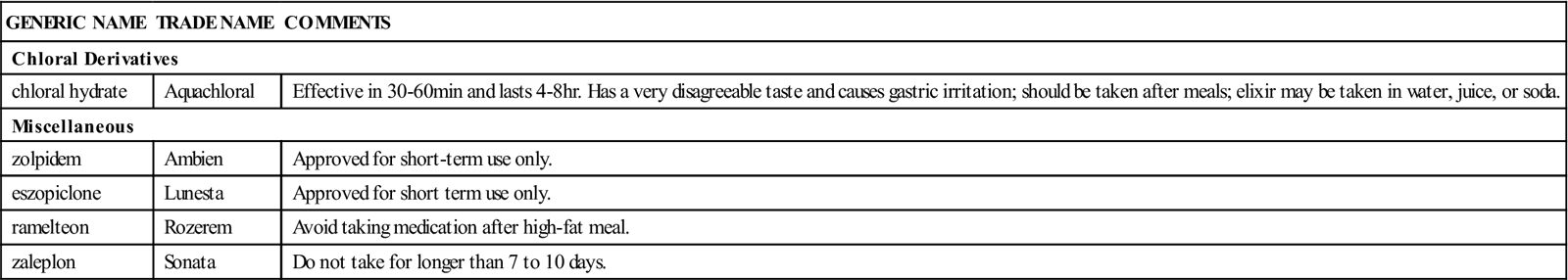
n Evaluation
Benzodiazepines are transformed by the liver into long-acting forms that may remain in the body for 24 hours or more and produce increasing sedation. Liver function may be impaired with long-term use. The onset of action is approximately 30 to 60 minutes; the effects last 7 to 8 hours. Sedative-hypnotics should always be discontinued slowly in people who have been on long-term therapy. Tolerance is usually proportional to the total amount of the drug received. Barbiturates are controlled substances, so attempts should be made to avoid giving them to patients with a history of abuse or addiction.
n Patient and Family Teaching
Tell the patient and family the following:
• The patient should take the medication exactly as prescribed.
• The medication should be kept out of reach of children and all others for whom it is not prescribed.
• It is dangerous for the patient to drink alcohol within 24 hours after taking this drug.
• Smoking may decrease the length of time the drug helps the patient sleep.
• The patient may develop excessive dreaming when the drug is stopped; this should lessen each night.