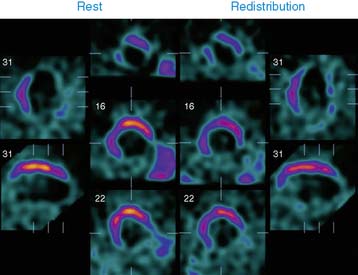
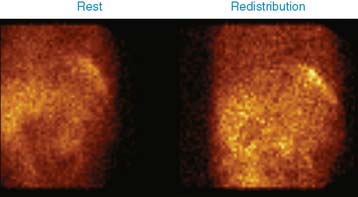
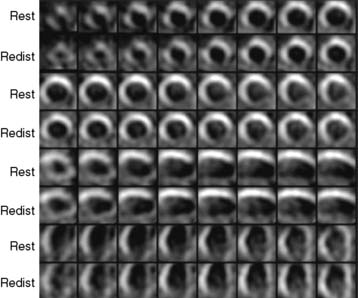
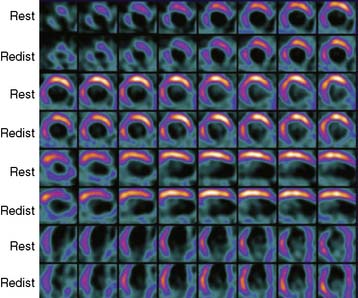
Case 16
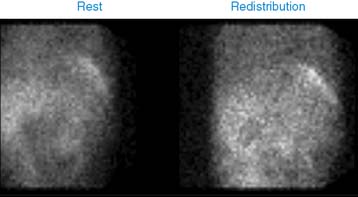
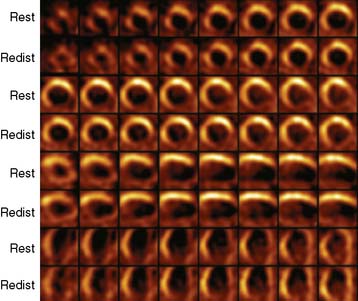
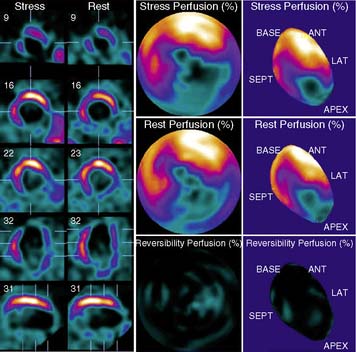
He was referred for a viability study to decide the further course of management and possible revascularization. A dose of 3.2 mCi of thallium-201 was injected at rest, followed by gated SPECT imaging 15 minutes and 4 hours later (Videos 4 and 5 and Figures 1 and 2). What is your interpretation of this study?