CASE 159
History: A 49-year-old man presents with right upper quadrant pain and a relevant past history of laparoscopic cholecystectomy 5 years ago.
1. What should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
2. What imaging modality would you recommend to evaluate further for bile duct injury related to this lesion in planning for intervention?
A. Endoscopic retrograde cholangiopancreatography (ERCP)
C. MRI with magnetic resonance cholangiopancreatography (MRCP)
D. Percutaneous cholangiography
3. What is the most common complication of laparoscopic cholecystectomy?
4. What is the most common benign neoplasm of the liver?
ANSWERS
CASE 159
Intrahepatic Biloma
1. C, D, and E
2. C
3. D
4. B
References
Thurley PD, Dhingsa R. Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol. 2008;191(3):794–801.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 241.
Comment
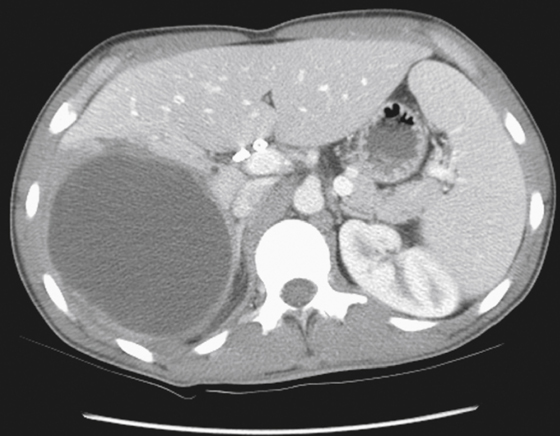
The CT image shows a large cystic, well-defined lesion taking up considerable space in the liver (see the figure). Major diagnostic considerations include some type of cystic structure communicating with the biliary system. Simple hepatic cysts, although lined by biliary tract epithelium, rarely communicate with the biliary system, despite their common occurrence. Echinococcal cysts may communicate with the biliary system, and a major complication is spontaneous rupture into the bile ducts or peritoneal cavity. Necrotic tumors or metastases rarely communicate with the biliary tract.
The most common cause for this intrahepatic cystic lesion, which was later drained, is the accumulation of bile as a result of a ruptured bile duct sustained in the initial injury. This injury may be seen following the course of cholecystectomy. During cholecystectomy, the surgeon often inserts probes or catheters into the bile ducts to identify possible retained calculi or debris. Sometimes a small endoscope is inserted into the ducts. Because intrahepatic ducts often taper rapidly, some of these small intrahepatic ducts may rupture during passage of some of these instruments. If a cholangiogram is obtained in the immediate postoperative period, a small area of extravasation may be identified.
Usually these small intrahepatic duct perforations close spontaneously after 2 to 3 weeks. Problems arise if pressure in the biliary system is increased because of obstruction, as in this patient. In this scenario, the bile collection may increase in size and form a biloma. If the biliary tract also is infected, the bile may become infected and form an abscess. The radiologist must recognize this complication and identify its true nature accurately. This study usually can be followed by drainage of the biloma and injection into the evacuated cavity to see if the leaking bile duct can be identified. If so, repeat injections of the drained biloma over the course of the next few weeks may be undertaken to show healing and integrity of the biliary system. Similar but more expensive mechanisms for following the healing biliary system would be serial CT and MRI studies. The most worrisome complications of a biloma are infection and leakage into the peritoneal cavity.