CHAPTER 158
Stroke
Definition
Stroke is an acquired injury of the brain caused by occlusion of a blood vessel or inadequate blood supply leading to infarction or a hemorrhage within the parenchyma of the brain. Ischemic stroke is most commonly due to atherosclerosis of large extracranial or intracranial blood vessels, hypertensive disease of small vessels (lipohyalinosis), or embolism from cardiac or other sources. Approximately 15% of strokes in the United States are hemorrhagic, resulting most commonly from hypertensive hemorrhages, aneurysms, vascular malformations, or cerebral amyloid angiopathy. Approximately 800,000 strokes occur annually in the United States, with a large population of survivors with permanent disability. Important modifiable risk factors for ischemic stroke include hypertension, smoking, diabetes, obesity, sedentary lifestyle, and hyperlipidemia; nonmodifiable risk factors include age, sex, and race/ethnicity. Risk factors for hemorrhage include hypertension and smoking as well as alcohol consumption.
Symptoms
The symptoms of stroke depend on the location of the injury in the brain. For example, a stroke in the distribution of the left middle cerebral artery will typically result in right hemiplegia, aphasia, and right homonymous hemianopia, whereas a lacunar infarct in the left internal capsule may result in a less severe degree of right-sided hemiparesis and few other symptoms. Left hemispatial neglect and impaired attention are common features of right hemispheric stroke. Ischemic strokes generally conform to the vascular territory of a specific artery within the brain and therefore result in characteristic combinations of neurologic impairments that constitute a particular stroke syndrome.
In general, difficulties in walking, performing activities of daily living, speaking, and swallowing are common manifestations of stroke. Cognitive impairments (memory, attention, visual-spatial perception) and impaired communication due to aphasia or dysarthria may be present. Impaired sexual function should be identified because patients may not volunteer functional impairments in this area unless the physician inquires. Loss of libido is common among both stroke survivors and their spouses or other partners and appears multifactorial in origin. Erectile dysfunction in men may result from comorbid conditions (such as diabetes or atherosclerosis), with frequent contributions from side effects of medications including antihypertensives, antidepressants, and anticonvulsant medications.
Weakness, difficulty in speaking or swallowing, aphasia, cognitive disturbance, sensory loss, and visual disturbance are the most common presenting symptoms of stroke, and deficits in these areas often persist even after initial rehabilitation. Weakness (typically hemiparesis) results from loss of motor control primarily, and some stroke survivors retain good strength despite limited ability to perform isolated precise movements of the affected side. Urinary urgency, increased muscle tone, fatigue, depression, and pain are symptoms that may be manifested after a stroke has already occurred. Reflex sympathetic dystrophy (also known as complex regional pain syndrome type I) may occur after stroke, although most post-stroke pain results from mechanical (e.g., joint subluxation) or central (e.g., thalamic pain syndromes) causes.
Depression is common after stroke, affecting as many as 40% of stroke survivors. Depression should be identified as a treatable complication of stroke rather than accepted as a consequence of functional loss.
Physical Examination
A full neurologic examination is appropriate. This includes evaluation of mental status, cranial nerves, sensation, deep tendon reflexes, abnormal reflexes (e.g., Babinski), motor strength and coordination, muscle tone, and functional mobility (sitting, transfers, and ambulation). The protean manifestations of stroke can cause many different combinations of abnormalities in these aspects of the neurologic examination. Common findings include hyperreflexia and hemiparesis on the affected side, with variable degrees of sensory loss. Dysarthria may be present, as can aphasia or hemineglect, depending on the areas affected. Hemiplegic gait is commonly seen, with reduced stride length, reduced knee flexion (“stiff-legged gait”), ankle plantar flexion and inversion, and circumduction to allow clearance of the affected leg. An assessment of mood and affect is important, given the high prevalence of post-stroke depression. Some degree of sadness is typically present as a normal grief reaction to a sudden disabling event and should be distinguished from true major depression on the basis of how pervasive the symptoms are and associated symptoms such as anhedonia. Emotional lability may also occur, with symptoms that tend to be fleeting and changeable. Range of motion in affected limbs should be measured; ankle plantar flexion contractures and upper limb contractures are common in patients with long-standing hemiplegic stroke and interfere with rehabilitation efforts. Shoulder subluxation may occur in hemiparetic patients and should be noted and quantified. Skin is examined for any areas of breakdown. Limb swelling is common and should be noted. The fit and function of leg braces, upper extremity splints, slings, wheelchairs, and ambulatory aids are assessed as part of the routine physical examination.
Functional Limitations
Depending on the impairments that patients have, they may be unable to drive or to use public transportation. Communication difficulties can lead to social isolation. Some individuals require ongoing supervision because of cognitive limitations. In severe cases, individuals with aphasia or cognitive impairments may not be able to live independently. Incontinence due to detrusor instability and urinary urgency can interfere with leaving the home and contribute to skin breakdown and social isolation.
Among stroke survivors older than 65 years who were evaluated 6 months after a stroke, 30% were unable to walk without some assistance, 26% were dependent for activities of daily living, and 26% were institutionalized in a nursing home [1].
Diagnostic Studies
In the acute setting, computed tomography is often the first diagnostic test performed because of the rapidity with which it can be obtained, its widespread availability, and its high sensitivity for cerebral hemorrhage. Magnetic resonance imaging provides greater anatomic resolution and avoids radiation exposure. With diffusion and perfusion-weighted sequences, magnetic resonance imaging abnormalities can be demonstrated at a very early stage, providing important information for acute treatments such as thrombolysis [2]. Magnetic resonance angiography, computed tomographic angiography, noninvasive flow studies, Holter monitoring, and echocardiography are important studies to help determine the cause of a stroke and to determine the best treatment for prevention of recurrent stroke. In selected patients (particularly young individuals or those without typical risk factors), an evaluation for a hypercoagulable state is indicated. In patients with prior stroke, diagnostic studies are typically directed to complications of stroke, such as persistent dysphagia or urinary incontinence. Videofluoroscopic swallowing studies can be useful in swallowing disorders, as can flexible endoscopic evaluation of swallowing. Urodynamic studies may be useful in the assessment of urinary symptoms, particularly if initial treatment with anticholinergic medications is unsuccessful.
Treatment
Initial
When ischemic stroke is diagnosed within the first 3 hours, thrombolytic therapy has been shown to reduce disability [3]. There is evidence that thrombolysis may be useful in selected individuals between 3 and 4.5 hours after stroke onset as well [4]. Mechanical clot retrieval and intra-arterial thrombolysis have been used successfully for patients who do not experience resumption of flow in the occluded artery with intravenous thrombolysis or who fall outside of the time window for this therapy [5]. Aspirin (between 80 and 325 mg) has been found to be effective when it is used in the acute setting. In younger patients with large ischemic strokes, increased intracranial pressure due to swelling may require hemicraniectomy to prevent herniation and death.
Secondary prevention depends on the cause of the stroke. Warfarin (Coumadin) is commonly used for the secondary prevention of embolic stroke, with the most extensive evidence for prevention of stroke in atrial fibrillation. Several new oral anticoagulants are increasingly used as alternatives to warfarin, including dabigatran (Pradaxa), apixaban (Eliquis), and rivaroxaban (Xarelto) [6,7]. Antiplatelet agents, including aspirin, clopidogrel (Plavix), or a combination of aspirin and dipyridamole (Aggrenox), are used for prevention of most non-cardioembolic strokes or when anticoagulation is desirable but contraindicated because of comorbid conditions. Risk factor modification, including treatment of hypertension, diabetes, hyperlipidemia, and obesity as well as smoking cessation and exercise, should be addressed for all stroke survivors.
Treatment of cerebral hemorrhage is based in part on the presumed cause. For hypertensive hemorrhages, control of blood pressure with antihypertensive medications is the mainstay of treatment. Large hemorrhages may require hematoma evacuation and removal of a portion of the skull to treat elevated intracranial pressure. For all causes of cerebral hemorrhage, avoidance of anticoagulants, antiplatelet medications, and alcohol is important.
Medications for the management of post-stroke symptoms on an outpatient basis are shown in Table 158.1. Anticholinergic medications are useful for bladder detrusor instability. Oral antispasticity medications are of limited efficacy in many cases (see Chapter 153). For sexual dysfunction in men, phosphodiesterase type 5 inhibitors may be effective. Treatment with selective serotonin reuptake inhibitors for post-stroke depression is widely employed, although a wide range of antidepressant medications can be effective. Psychostimulants (e.g., methylphenidate) and eugeroics (e.g., modafinil) may be useful for impaired attention. Anticonvulsants are used for central pain syndromes, but with variable benefit.
Table 158.1
Medications Commonly Used for Treatment of Post-Stroke Symptoms
| Class of Medication | Examples | Indication |
| Anticholinergics | Oxybutynin (Ditropan) Tolterodine (Detrol) |
Bladder detrusor instability |
| Antispasticity | Baclofen (Lioresal) Tizanidine (Zanaflex) Diazepam (Valium) Dantrolene (Dantrium) |
Muscle spasticity |
| Phosphodiesterase type 5 inhibitors | Sildenafil (Viagra) Vardenafil (Levitra) |
Erectile dysfunction |
| Selective serotonin reuptake inhibitors | Fluoxetine (Prozac) Paroxetine (Paxil) Sertraline (Zoloft) |
Post-stroke depression |
| Stimulants | Methylphenidate (Ritalin) Dextroamphetamine (Dexedrine) |
Impaired attention, arousal |
| Eugeroics | Modafinil (Provigil) Armodafinil (Nuvigil) |
Impaired arousal, attention |
| Anticonvulsants | Gabapentin (Neurontin) Carbamazepine (Tegretol) |
Central pain syndromes, seizure disorders |
Rehabilitation
The rehabilitation program needs to be customized on the basis of the severity and nature of the impairments caused by the stroke. For individuals with moderate to severe stroke, a comprehensive multidisciplinary inpatient rehabilitation program in a rehabilitation hospital is often appropriate and may lead to improved outcomes [8]. Stroke patients with significant functional limitations in mobility, communication, cognition, or self-care who are capable of participating in and benefiting from an intensive rehabilitation program consisting of 3 hours or more of rehabilitation therapy per day commonly undergo an inpatient rehabilitation stay. For these individuals, rehabilitation commonly continues through home care or outpatient services after discharge from the rehabilitation hospital/unit. Patients with more circumscribed and less severe deficits may be discharged directly from the acute care hospital to home and participate in an outpatient rehabilitation program [9]. Patients who are unable to participate in an aggressive rehabilitation program because of poor motivation, severe cognitive deficits, or poor prognosis may receive inpatient rehabilitation at a subacute program (skilled nursing facility) instead, as may some patients with milder deficits who are unable to be discharged directly home. There is considerable practice variation regarding referral to an inpatient rehabilitation facility versus a skilled nursing facility and only limited observational data comparing outcomes in the two types of facilities [8,10]. Although not definitive, these studies suggest better outcomes for patients receiving inpatient care, and stroke patients who meet the admission criteria and have insurance coverage for this type of care should be preferentially referred to inpatient rehabilitation facilities when it is feasible.
Exercise
Therapeutic exercise programs are usually functionally oriented, with an emphasis on restoration of functional mobility and ability to perform activities of daily living (Fig. 158.1). Instruction in compensatory techniques and family teaching are important in assisting individuals to return home. There is growing evidence of the impact of therapeutic exercise on cortical reorganization after stroke, with associated improvements in motor control and functional use of the affected limbs [11]. Newer approaches being studied to enhance motor abilities include constraint-induced movement therapy, robot-assisted exercise training (Fig. 158.2), and virtual reality exercise training [11–14]. These novel techniques appear to improve motor function, but the optimal exercise program to facilitate recovery remains to be defined.
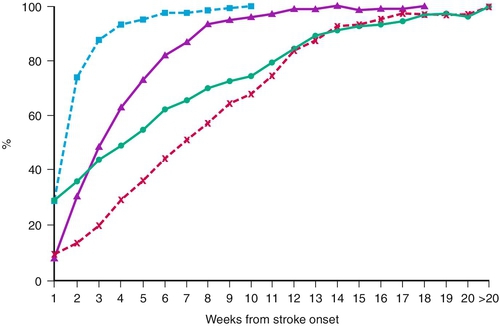
 , mild disability;
, mild disability;  , moderate disability;
, moderate disability;  , severe disability; and
, severe disability; and  , very severe disability. (From Jorgensen HS, Nakayama H, Raaschou HO, et al. Outcome and time course of recovery in stroke. Part II. Time course of recovery. The Copenhagen Stroke Study. Arch Phys Med Rehabil 1995;76:406-412.)
, very severe disability. (From Jorgensen HS, Nakayama H, Raaschou HO, et al. Outcome and time course of recovery in stroke. Part II. Time course of recovery. The Copenhagen Stroke Study. Arch Phys Med Rehabil 1995;76:406-412.)
Electrical Stimulation
Noninvasive brain stimulation has been studied as a means of enhancing motor recovery and for treatment of aphasia after stroke. This can be delivered by transcranial magnetic stimulation or transcranial direct current stimulation. Preliminary studies suggest benefit of this therapy when it is combined with exercises, but definitive trials have not yet been performed [15].
Dysphagia
Management of dysphagia may include nasogastric or gastrostomy tube feedings, modified diets (e.g., thickened liquids, pureed foods), and swallowing therapy (e.g., the use of compensatory strategies, such as “tucking” the chin during swallowing).
Communication
The rehabilitation of aphasia relies on extensive speech therapy as its mainstay; selected patients benefit from communication aids, such as a picture board. Speech therapy may provide significant benefit for dysarthria as well, resulting in improved intelligibility. Severely dysarthric or anarthric patients may benefit from the use of computer-based communication aids, including those with speech synthesis, as well as “low-tech” solutions, such as spelling boards.
Cognition
Cognitive abilities are frequently affected by stroke; alterations in memory, attention, insight, and problem solving are common. Neuropsychological testing may be useful in defining the precise nature of these deficits and in helping to develop a remediation plan. Speech-language and occupational therapy approaches include attempts at remediation and teaching of compensatory techniques. Family education and training are important components of cognitive rehabilitation. Recognition and treatment of post-stroke depression are important because depression can contribute to reduced cognitive performance after stroke [16].
Bracing
Lower extremity bracing is frequently helpful in restoration of mobility in hemiparetic stroke survivors. Most commonly, a plastic or carbon-fiber ankle-foot orthosis is used, although other braces are appropriate in selected circumstances. Bracing is helpful as a compensation for impaired ankle dorsiflexion, controlling ankle inversion and plantar flexor spasticity as well as providing some stabilization at the knee. Electrical stimulation systems (e.g., Bioness L300, WalkAide) can be used to stimulate dorsiflexion as an alternative to a brace for selected patients.
Ambulatory Aids and Wheelchairs
Because of hemiparesis, many stroke survivors require ambulatory aids, which may include a straight cane, a four-pronged (“quad”) cane, a hemi-walker, or, in some cases, a conventional walker. Wheelchairs are often needed for more severely impaired stroke survivors or for moderately impaired stroke survivors for longer distance travel. A hemi-wheelchair is lower to the ground and allows use of the nonparetic leg to assist with propulsion. On occasion, a one-arm drive wheelchair is useful; it allows control of both wheelchair wheels from one side. Active, nonambulatory individuals may benefit from a power wheelchair.
Shoulder Subluxation
Shoulder subluxation commonly occurs in the setting of hemiplegia after stroke, although the presence of pain is highly variable. Arm boards and the selective use of slings help in reducing subluxation. Electrical stimulation may have a beneficial effect as well [17].
Splints
Splints for proper positioning of the hemiplegic arm and ankle-foot are important to prevent contracture. These are particularly important when spasticity is present. Failure to properly splint and stretch the hand and wrist can result in progressive contracture leading to deformity, even with relatively mild spasticity.
Vocational Rehabilitation
Although stroke is predominantly a disease of older individuals, a significant portion of stroke survivors are of working age. Once activities of daily living have been mastered, vocational counseling may assist individuals seeking to return to work. Coordination with the rehabilitation team is important because retraining for certain job tasks may involve a multidisciplinary effort. Accommodations in the workplace may be necessary, and the Americans with Disabilities Act may require the employer to provide reasonable accommodation for individuals with disabilities.
Procedures
Botulinum toxin or phenol injections may be useful in the management of spasticity after stroke. These injections are described in greater detail in Chapter 153.
Surgery
Selected patients require craniotomy in the acute phase for evacuation of a large intracerebral hematoma or for severe swelling with increased intracranial pressure. Carotid endarterectomy or stenting in appropriately selected patients has been shown to reduce the risk of recurrent stroke [18]. Intrathecal baclofen pumps have been found to be effective in treatment of post-stroke spasticity [19,20] but are infrequently used for hemiplegic stroke at this time. In patients with chronic impairments from stroke, tendon lengthening procedures are occasionally needed for contractures.
Potential Disease Complications
Seizures can develop as an early or a late complication of stroke; strokes involving the cerebral cortex and hemorrhagic stroke carry greater risk. The risk of deep venous thrombosis is substantially elevated in hemiplegic stroke, and prophylactic treatment with subcutaneous heparin or low-molecular-weight heparin is advisable during the initial recovery phase [21]. The ideal duration of prophylaxis for deep venous thrombosis after stroke has not been established; in most cases, this is discontinued after a period of several weeks. Stroke recurrence is a feared complication of stroke, and individuals with a history of stroke remain at increased risk for recurrent stroke despite risk factor reduction. Aspiration pneumonia can occur as a complication of dysphagia, although this risk tends to abate over time except in the most severe cases.
Potential Treatment Complications
Both anticoagulants and antiplatelet medications can contribute to bleeding complications. Aspirin can cause gastritis. Clopidogrel has been associated with thrombotic thrombocytopenic purpura. The combined use of aspirin and clopidogrel does not provide additional protection against stroke but increases the risk of gastrointestinal hemorrhage [22].
Anticholinergic medications commonly cause dry mouth and may precipitate urinary retention. Antispasticity medications can cause sedation and may exacerbate cognitive impairments. Sildenafil is known to be hazardous when it is used concurrently with nitrates and should be avoided in patients receiving these medications. Selective serotonin reuptake inhibitors can cause gastrointestinal symptoms (especially nausea and anorexia) as well as interfere with libido and sexual function. Psychostimulants can cause anorexia, insomnia, anxiety, or agitation and should be slowly titrated upward. Gabapentin is usually well tolerated, although occasional sedation has been reported. Carbamazepine may cause leukopenia.







