CASE 153

History: A 35-year-old woman presents with heartburn and dyspnea.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the most common viscus used for esophageal interposition surgery?
3. What is the most common serious postoperative complication of esophageal interposition surgery?
4. Esophagectomy with interposition is also performed for management of esophageal carcinoma; however, tumors recur in 60% to 75% of cases. Where do tumors most commonly recur?
ANSWERS
CASE 153
Colonic Interposition
1. A, B, D, and E
2. A
3. A
4. B
References
Kim SH, Lee KS, Shim YM, et al: Esophageal resection: indications, techniques, and radiologic assessment. Radiographics. 2001;21(5):1119–1137.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 39.
Comment
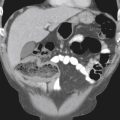
A patient with severe esophageal disease may require surgical bypass when the native esophagus is obstructed or no longer functional. Some surgeons use a length of colon and anastomose it from the upper thoracic or cervical esophagus to the stomach (see figures). Alternatively, jejunum may be used, bypassing the diseased esophagus. The remaining esophagus may be surgically isolated but usually is not removed because of potential damage to nerves, lymphatics, and collateral blood flow. Colonic interposition is commonly performed in patients with benign diseases, such as caustic or peptic strictures, or severe motor disorders. Occasionally, this procedure is performed in patients with malignant disease, in particular, if there is a good chance of survival or if a complication, such as perforation, has occurred.
Complications are common because of the complexity of the surgery. Early complications include anastomotic leakage and possible fistula formation. Stenoses also may develop at the anastomotic sites, typically the proximal site. Aspiration of ingested contents is another problem. Later problems include stasis of swallowed material within the interposed segment and reflux of gastric contents into the colonic interposition. Malignancy has been described in these colonic interpositions, but it is rare.
In the course of the surgery, if the surgeon isolates the esophagus by surgically closing its ends, a mucocele of the esophagus may develop. This mucocele consists of mucous or proteinaceous secretions that fill the lumen of the isolated esophagus and have nowhere to drain. The phenomenon is usually self-limited because increasing pressure within the lumen causes cessation of the mucous secretion. Rarely, the mass continues to increase in size, leading to symptoms. However, in the absence of an adequate history, the presence of a transposed colon or jejunum in the chest may surprise the resident or radiologist. Talking to the patient before the examination is very good; being surprised during the performance of the examination is not.