Procedure 15 Nerve Transfer Techniques for Elbow Flexion in Brachial Plexus Palsy
Indications
 Lack of elbow flexion/supination
Lack of elbow flexion/supination
 Available functional donor nerve with a lesser-valued function (e.g., ulnar fascicle to flexor carpi ulnaris with normal muscle power) in close proximity with recipient nerve/muscle
Available functional donor nerve with a lesser-valued function (e.g., ulnar fascicle to flexor carpi ulnaris with normal muscle power) in close proximity with recipient nerve/muscle
 Available recipient nerve without distal injury (e.g., intact musculocutaneous nerve branch to biceps in patients with supraclavicular brachial plexus injury)
Available recipient nerve without distal injury (e.g., intact musculocutaneous nerve branch to biceps in patients with supraclavicular brachial plexus injury)
 Donor and recipient nerves ideally with agonistic functions (e.g., flexion of elbow, wrist)
Donor and recipient nerves ideally with agonistic functions (e.g., flexion of elbow, wrist)
Examination/Imaging
Clinical Examination
 Examine the involvement of all muscles that contribute to elbow flexion—biceps, brachialis, and brachioradialis—to determine the site of injury (e.g., nerve root versus peripheral nerve).
Examine the involvement of all muscles that contribute to elbow flexion—biceps, brachialis, and brachioradialis—to determine the site of injury (e.g., nerve root versus peripheral nerve).
 Examine the active and passive range of motion at the elbow.
Examine the active and passive range of motion at the elbow.
 Examine the integrity of the vascular supply to the arm.
Examine the integrity of the vascular supply to the arm.
 Examine the integrity of the donor nerve/muscle (e.g., flexor carpi ulnaris).
Examine the integrity of the donor nerve/muscle (e.g., flexor carpi ulnaris).
 Determine whether the biceps muscle is ruptured, because end-organ injury would preclude nerve transfer.
Determine whether the biceps muscle is ruptured, because end-organ injury would preclude nerve transfer.
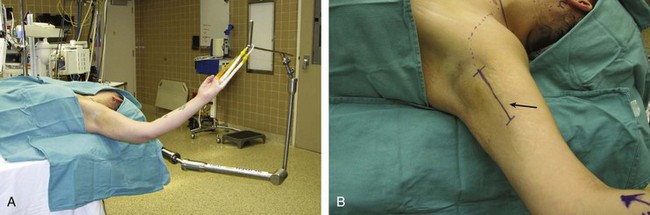
Positioning
Exposures
 Ulnar fascicle to musculocutaneous nerve: An incision is made along the medial arm from the pectoralis muscle insertion site to distally, with the incision overlying the path of the neurovascular bundle that lies between the biceps and triceps (see Fig. 15-1).
Ulnar fascicle to musculocutaneous nerve: An incision is made along the medial arm from the pectoralis muscle insertion site to distally, with the incision overlying the path of the neurovascular bundle that lies between the biceps and triceps (see Fig. 15-1).
 Double fascicular nerve transfer for elbow flexion: The double fascicular nerve transfer for elbow flexion employs (1) the ulnar nerve fascicles innervating the flexor carpi ulnaris to the musculocutaneous branch innervating the biceps; and (2) the median nerve fascicles innervating the flexor carpi radialis to the musculocutaneous branch innervating the brachialis.
Double fascicular nerve transfer for elbow flexion: The double fascicular nerve transfer for elbow flexion employs (1) the ulnar nerve fascicles innervating the flexor carpi ulnaris to the musculocutaneous branch innervating the biceps; and (2) the median nerve fascicles innervating the flexor carpi radialis to the musculocutaneous branch innervating the brachialis.
Pearls
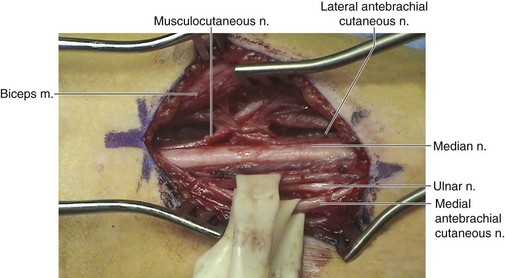
The ulnar nerve is more medial than the median nerve. The brachial artery is adjacent to the median nerve (Fig. 15-2).
The first nerve exposed is usually the medial antebrachial cutaneous nerve that can be traced proximally to the medial cord and ulnar nerve.
The musculocutaneous nerve and its branches can be found under the biceps muscle; identifying the lateral antebrachial cutaneous nerve and tracing it proximally to expose the main trunk of the musculocutaneous nerve may facilitate exposure.
The fascicle of the ulnar nerve to the flexor carpi ulnaris usually lies in the volar radial position within the ulnar nerve.
Procedure
Step 1
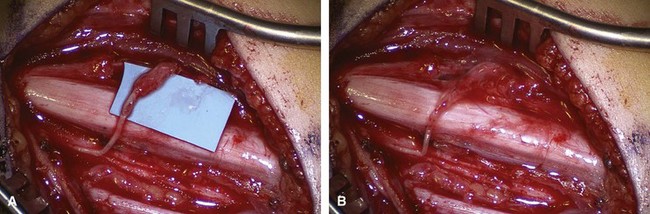
 Open the biceps fascia to reveal the branch of the musculocutaneous nerve innervating the biceps muscle and transect it proximally.
Open the biceps fascia to reveal the branch of the musculocutaneous nerve innervating the biceps muscle and transect it proximally.
Step 1 Pearls
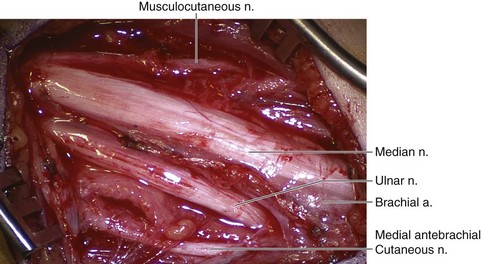
Ensure careful identification and protection of the median nerve, ulnar nerve, and brachial artery (Fig. 15-3).
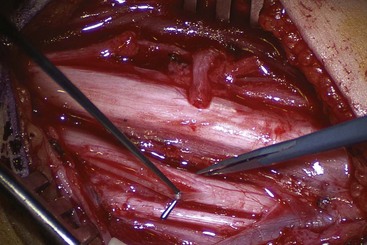
The branches of the musculocutaneous nerve to the biceps can be dissected proximally by opening the epineurium until its fascicles become physically inseparable from the parent nerve, then transected sharply to serve as the recipient nerve (Fig. 15-4).
Step 2
 Isolate the appropriate ulnar nerve fascicles for use as the donor by opening the epineurium of the ulnar nerve (see Fig. 15-4).
Isolate the appropriate ulnar nerve fascicles for use as the donor by opening the epineurium of the ulnar nerve (see Fig. 15-4).
 The desired fascicles can be dissected proximally and distally until they are of adequate length for a tension-free coaptation with the musculocutaneous nerve. The fascicles are then transected sharply as distally as possible and coapted with the appropriate recipient nerve (see Fig. 15-4).
The desired fascicles can be dissected proximally and distally until they are of adequate length for a tension-free coaptation with the musculocutaneous nerve. The fascicles are then transected sharply as distally as possible and coapted with the appropriate recipient nerve (see Fig. 15-4).
Step 2 Pearls
Careful intraneural dissection will reveal one or two fascicles with diffuse innervation of the distal muscles with emphasis on the flexor carpi ulnaris (usually found superficially in the ulnar nerve) using intraoperative nerve stimulation; avoid those fascicles with primary innervation to the hand intrinsic muscles.
Step 3
 If both the musculocutaneous branches to the biceps and brachialis are desired, in addition to the dissection for the ulnar nerve fascicles, an intraneural dissection of the median nerve is undertaken.
If both the musculocutaneous branches to the biceps and brachialis are desired, in addition to the dissection for the ulnar nerve fascicles, an intraneural dissection of the median nerve is undertaken.
 Locate the branch of the musculocutaneous nerve innervating the brachialis distal to the branch to the biceps.
Locate the branch of the musculocutaneous nerve innervating the brachialis distal to the branch to the biceps.
Postoperative Care and Expected Outcomes
 A soft wrap or sling can be used with care to avoid pressure on the medial aspect of the arm.
A soft wrap or sling can be used with care to avoid pressure on the medial aspect of the arm.
 Physical therapy for range of motion can start 4 to 6 weeks postoperatively.
Physical therapy for range of motion can start 4 to 6 weeks postoperatively.
 Recovery of reinnervated muscle function occurs from 6 months to 3 years postoperatively.
Recovery of reinnervated muscle function occurs from 6 months to 3 years postoperatively.
 The expected outcome of the surgery is improved active elbow flexion.
The expected outcome of the surgery is improved active elbow flexion.
Bertelli JA, Florianopolis SC, Ghizoni MF, Tubarao SC. Reconstruction of C5 and C6 brachial plexus avulsion injury by multiple nerve transfers: spinal accessory to suprascapular, ulnar fascicles to biceps branch, and triceps long or lateral head branch to axillary nerve. J Hand Surg [Am]. 2004;29:131-139.
Carlsen BT, Kircher MF, Spinner RJ, et al. Comparison of single versus double nerve transfers for elbow flexion after brachial plexus injury. Plast Reconstr Surg. 2011;127:269-276.
Goulet B, Boretto JG, Lazerges C, Chammas M. A comparison of intercostal and partial ulnar nerve transfers in restoring elbow flexion following upper brachial plexus injury (C5-C6 ± C7). J Hand Surg [Am]. 2010;35:1297-1303.
Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg [Am]. 2005;30:978-985.