Cardiovascular and Renal Medications
Objectives
1. Identify the approved way to give different forms of antianginal therapy.
2. Discuss the uses and general actions of cardiac drugs used to treat dysrhythmias.
3. Describe the common treatment for various types of lipoprotein disorders.
4. List the general uses and actions of cardiotonic drugs.
5. Explain the actions of different categories of drugs used to treat hypertension.
Key Terms
action potential duration (ĂK-shun PŌ-těn-chăl, p. 220)
congestive heart failure (CHF) (HĂRT FĀL-yŭr, p. 229)
chronotropic (KRŎ-nō-TRŌP-ĭk, p. 221)
compelling indications (p. 238)
dehydration (dē-hī-DRĀ-shŭn, p. 247)
depolarization (dē-pō-lăr-ĭ-ZĀ-shŭn, p. 221)
digitalis toxicity (dĭj-ĭ-TĂL-ĭs, p. 231)
digitalizing dose (DĭJ-ĭ-tăl-īz-ĭng, p. 231)
dromotropic (DRŎM-ō-TRŎP-ĭk, p. 221)
dysrhythmia (dĭs-RĬTH-mē-ă, p. 219)
ectopic beats (ěk-TŎP-ĭk, p. 220)
edema (ě-DĒ-mă, p. 229)
effective refractory period (rē-FRĂK-tŏr-ē, p. 220)
electrocardiogram (ECG) (ě-lěk-trō-KÄR-dē-ō-gram, p. 219)
end-organ damage (p. 238)
fluid and electrolyte mixtures (ě-LĚK-trō-līt, p. 247)
hyperlipidemia (hī-pěr-lĭp-ĭ-DĒ-mē-a, p. 224)
hyperlipoproteinemia (hī-pěr-līp-ō-PRŌT-ě-NĒ-mē-ă, p. 226)
myocardial infarction (MI) (mī-ō-KÄR-dē-ăl ĭn-FÄRK-shŭn, p. 225)
myocardium (mī-ō-KÄR-dē-ŭm, p. 219)
normal sinus rhythm (SĪ-nŭs RĬTH-ĭm, p. 219)
pacemaker (PĀS-MĀ-kěr, p. 219)
positive inotropic action (ĭ-nă-TRŎP-ĭk, p. 230)
primary hypertension (PRĪ-măr-ē hī-pěr-TĚN-shŭn, p. 233)
secondary hypertension (SĔK-ŏn-dār-ē hī-pěr-TĚN-shŭn, p. 233)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
This chapter is divided into six major sections, each with a focus on an important job of the cardiovascular, circulatory, or renal system. Some cardiovascular drugs have more than one action and are used for several reasons in the patient with cardiovascular problems. However, they are usually classified into one of the major drug categories.
The first section, Antianginals and Peripheral Vasodilators, focuses on the drugs used to treat chest pain from angina and problems with diseases causing blockage of the arteries, mostly in the legs. These drugs are widely used, and the nurse will have a major role in teaching the patient how to properly store and use them. The second section discusses the four major classes of medications used for dysrhythmias (irregular heartbeats). The antidysrhythmics are powerful drugs, and there may be many adverse reactions from some of these medications. The third section looks at lipids (fats) and the problem of lipoprotein abnormalities. Antihyperlipidemic agents are discussed as a part of the overall therapy for lipoprotein problems. The fourth section focuses on the drugs that make the heartbeat stronger—the cardiotonics or positive inotropic agents, such as digitalis and related products. These are some of the most common drugs for patients both in and out of the hospital, and some of the “must know” drugs. Antihypertensives, diuretics, and urinary system drugs are explored in the fifth section. Because hypertension (high blood pressure) is so common, the nurse will use many of these drugs. The latest guidelines for lowering blood pressure are listed, as well as common adverse reactions to these drugs. Although most of the drugs acting on the kidney are diuretics, other agents that affect the urinary tract are also presented here. The sixth section covers fluid and electrolytes, which nurses also frequently give.
These classifications have many drugs and these sections give the most important basic information about each drug category. If the nurse reviews the anatomy and physiology of the cardiovascular and urinary systems at the same time, it will help them understand both the problems that occur in these systems and how the different drugs act to solve those problems.
Cardiovascular and Urinary Systems 
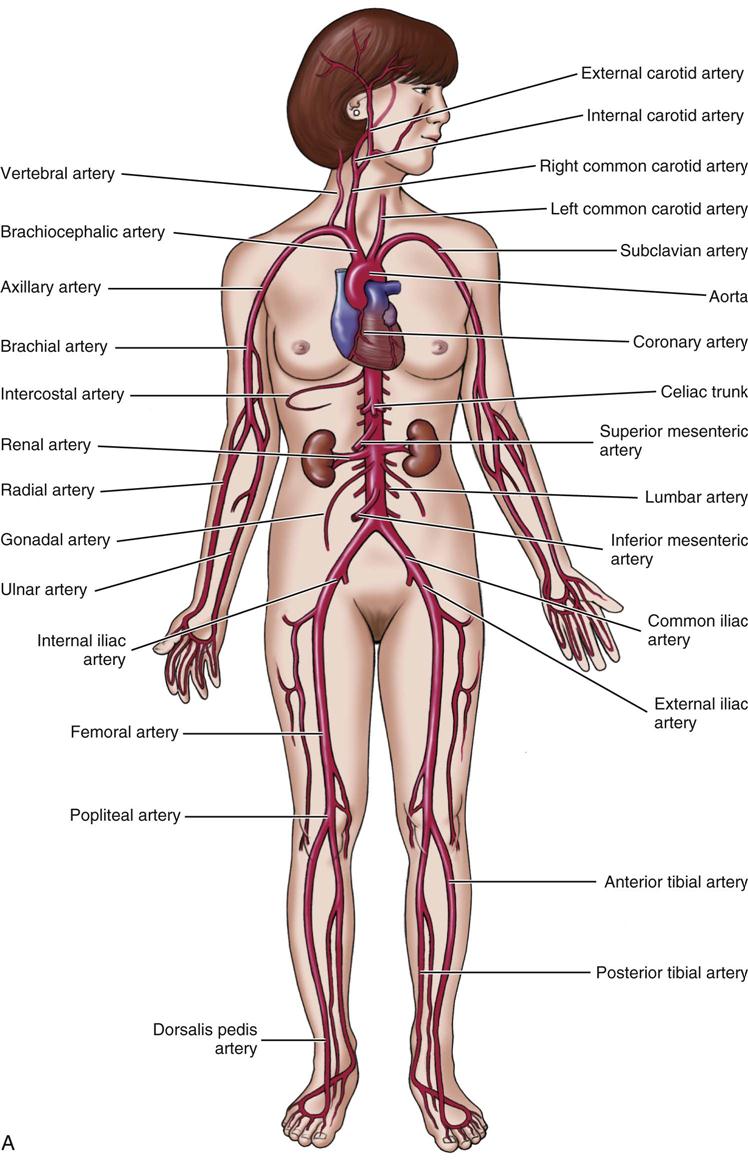
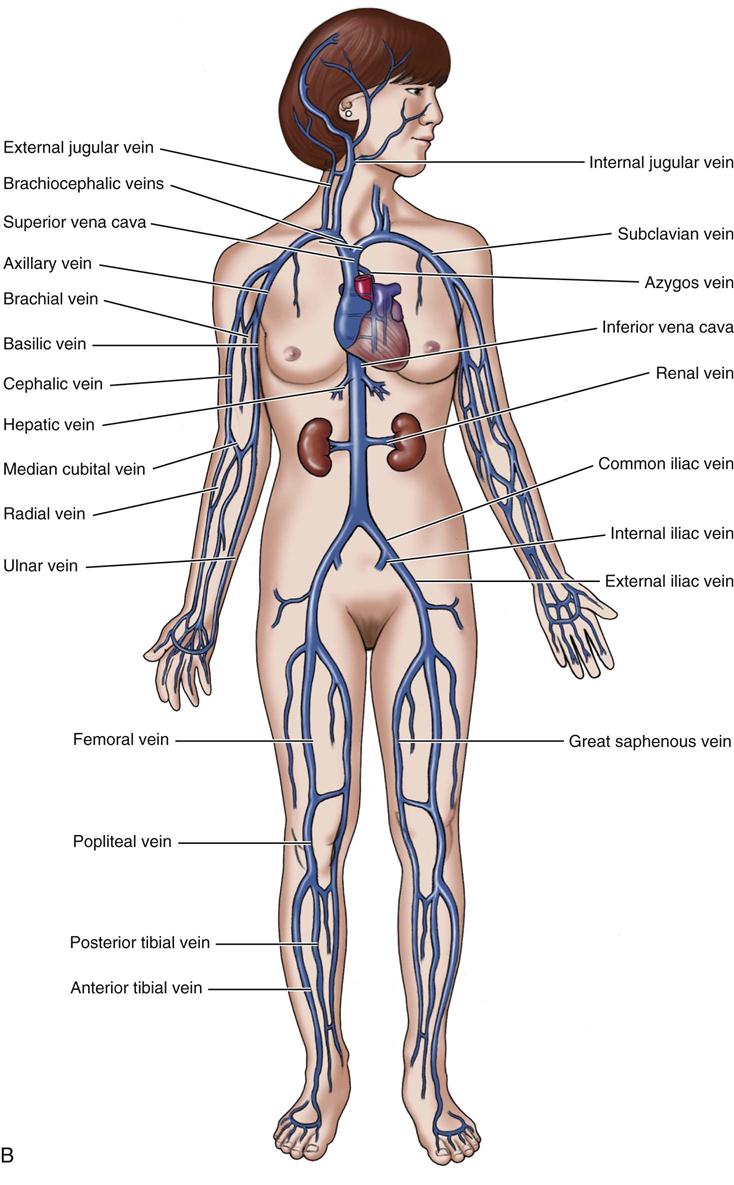
The cardiovascular system is made up of the heart, blood vessels (Figure 15-1), and blood. This system moves nutrients (substances that support life and growth), waste products, gases, and hormones through the body. It also plays a role in the immune response and changes in body temperature.
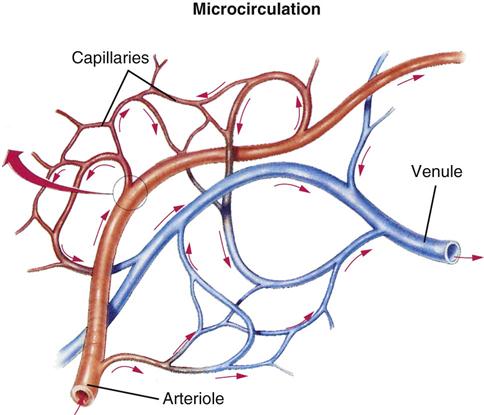
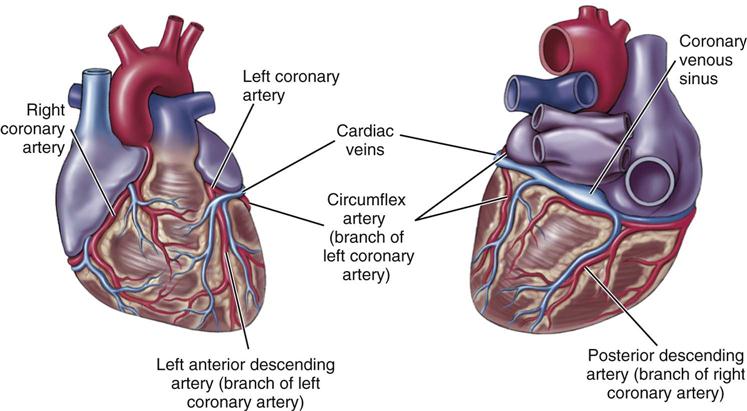
Using special cardiac muscle and nerve systems, electrical impulses tell the heart muscle when to contract, forcing blood from the heart, through blood vessels, and out through the body. Arteries move blood from the heart to tissues using smaller branches called arterioles. Veins move blood from tissues back toward the heart, beginning with their smaller branches, called venules. Capillaries are very small vessels that link arterioles and venules.
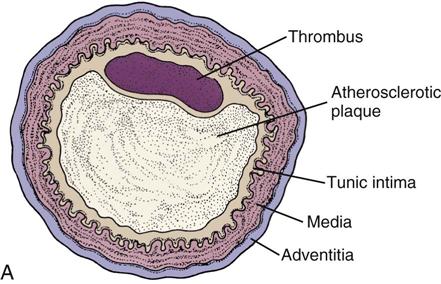
The heart is the pump of the circulation system. The heart itself is fed by small coronary arteries that send nutrients to it during the resting phase of the cardiac cycle. The heart may weaken with disease and age and become less efficient. Sometimes the arteries become stiff and the walls become filled with fatty plaques from cholesterol or lipids. This condition is called atherosclerosis. In patients with hypertension, the blood vessels become less elastic, and the increased pressure against which the heart has to pump causes the heart to work harder. Thus diseases or abnormal conditions of the heart, arteries, or veins produce more stress on the heart itself. When blood cannot flow through the heart muscles, the muscles hurt from lack of oxygen (angina). This severe chest pain is called angina pectoris. In a heart attack (myocardial infarction [MI]), some of the heart muscle cells actually die and a scar forms. Medicine can often control the pain of angina and prevent heart attacks when the heart doesn’t have to work so hard.
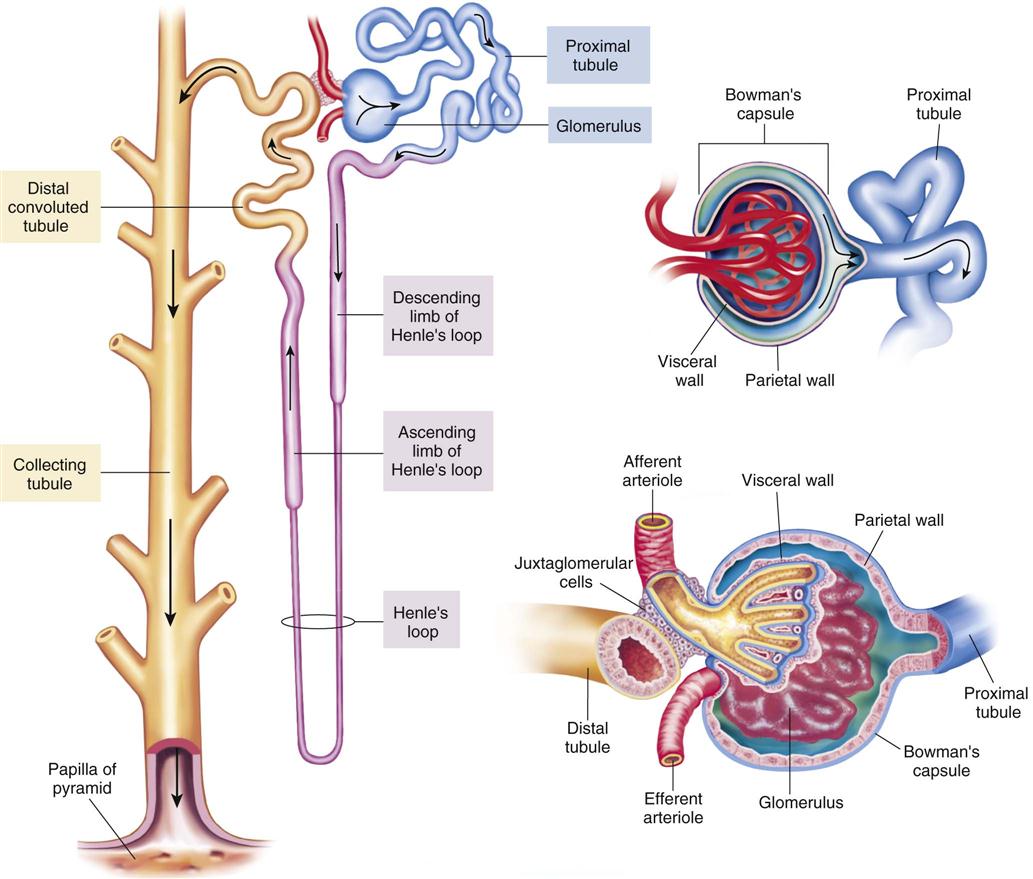
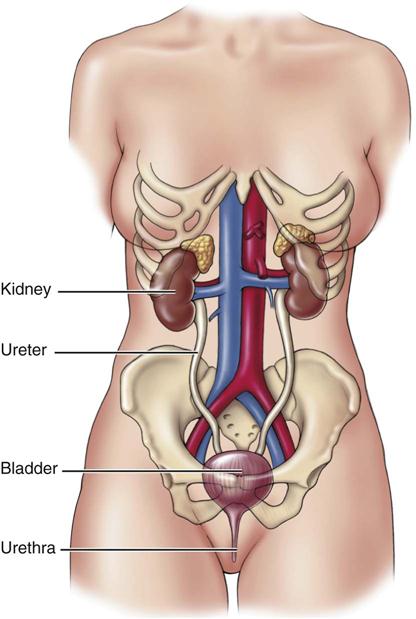
Many of the cardiovascular drugs also have either direct or indirect action on the urinary system (Figure 15-2). The kidneys, urinary bladder, and ducts that carry urine work together to remove waste products from the circulatory system, to regulate blood pH and ion levels, and to maintain water balance. Strong pumping of the heart, good circulation through the vessels, and the full removal of waste products through the urinary system are all needed to keep the body’s fluids and electrolytes in balance.
Antianginals and Peripheral Vasodilators
Overview
Narrowing or constriction of the smooth muscle in the small coronary arteries of the heart and the peripheral vascular system (vessels in the arms and legs) reduces the amount of blood carried to the heart and the peripheral tissues (Figure 15-3). When there is a lack of blood supply to bring oxygen and nutrients to the heart or to peripheral tissues, the pain of angina or peripheral vascular disease is felt.
Action
The heart receives its blood supply and oxygen from the coronary arteries. These small arteries are often plugged or damaged when the patient has angina or a heart attack. Blood may also be cut off from the coronary arteries if there is coronary vasospasm. Blockage or spasm causes cardiac angina when the heart muscle is without oxygen. Currently there are three major classes of drugs used in the medical management of angina. Nitrates (both short and long acting), β-blockers, and calcium channel blockers. Some other vasodilating agents (agents to open up the vessels) are used for increasing circulation in peripheral vascular disease. (Information about the use of beta blockers in treating angina by decreasing the oxygen demands of the heart and calcium channel blockers that may relieve angina by dilating the coronary vessels and reducing the work load of the heart can be found in the discussion of antihypertensives and diuretics in the fifth section of this chapter.)
Nitrates
Nitrate products have a direct action on vascular smooth muscle and cause it to relax. This effect is felt in both the circulation in arteries and veins. Arterial relaxation reduces the pressures the heart has to pump against (afterload), whereas venous relaxation helps in pooling of venous blood, thereby decreasing the amount of blood returned to the heart (preload). These effects work together to decrease myocardial oxygen use. In addition, nitrates increase the use of the other small blood vessels in the heart (collaterals) so that there is better oxygen supply to the inner layers of the heart muscle.
Calcium Channel Blockers 
Calcium is an electrolyte that helps move electrical impulses through cardiac tissue. Calcium channel blockers are drugs that help slow down the flow of calcium ions across the cell membrane, thus reducing the amount of calcium available for electrical impulse movement. The drugs in this group are used for a variety of actions. Some calcium channel blockers act directly on vascular smooth muscle to dilate (open up) coronary arteries and arterioles, which relieves anginal pain because more oxygen can go to the cardiac tissue. Other calcium channel blockers are used to reduce the response of the cardiac conduction system to electrical impulses and treat cardiac dysrhythmias. They are also used along with other drugs to treat hypertension. (See the sections on antidysrhythmics and antihypertensives for additional information on calcium channel blockers and beta-adrenergic blockers.)
Peripheral Vasodilators
Patients with occlusive arterial disease (blockage of the arteries that makes them smaller) have been treated with vasodilating drugs (drugs that help expand or open up the arteries), but with only limited success. These patients have decreased blood flow, which produces cold extremities, thin shiny skin, decreased hair growth on the legs, and the inability to walk without experiencing pain in their legs. Vasodilator drugs relax the smooth muscles of peripheral arterial blood vessels and help lead to better circulation to the arms and legs (Figure 15-4).
Uses
Rapid-acting nitrates (such as amyl nitrite, sublingual nitroglycerin, and sublingual or chewable isosorbide dinitrate) are used mostly to relieve pain in acute angina. The long-acting nitrates and topical, transdermal, transmucosal, and oral sustained-release nitroglycerin products are used to prevent or treat anginal attacks when they are likely to occur (for example, with exercise) and to reduce the severity and frequency of anginal attacks. They are also used to reduce the work of the heart in cases of MI and in chronic heart failure; and for relief of gallbladder, gastrointestinal (GI), urethral, and bronchial smooth muscle pain.
It is not always clear if it is safe to use nitroglycerin in patients with acute MIs. When it is used in patients with recent MIs, the transdermal patch systems work best, but patients must be closely evaluated. Intravenous (IV) nitroglycerin is used to control severe angina in an acute MI and also to control acute pain during procedures on the heart, such as cardiac catheterization. This IV nitroglycerin requires careful monitoring of the patient in a cardiac care or critical care unit due to the possibility the medicine may cause a severe drop in blood pressure.
Peripheral vasodilating agents are used to treat pain in the legs caused by problems such as intermittent claudication, arteriosclerosis obliterans, Raynaud’s disease, nocturnal leg cramps, and vasospasm caused by blood clots.
Adverse Reactions
There are many common adverse reactions to nitrates, including flushing, postural hypotension (low blood pressure when a person suddenly stands up), tachycardia (rapid heartbeat), confusion, dizziness, fainting, headache, light-headedness, vertigo (feeling of dizziness or spinning), weakness, drug rash, localized pruritus (itching), local burning in the mouth, nausea, and vomiting.
Some of these cardiac preparations contain tartrazine, a chemical that may cause an allergic type of reaction with symptoms similar to asthma. Patients who are allergic to aspirin have a greater chance of reacting to tartrazine.
When nitrate products are used, high doses may cause violent headaches. All nitrates should be given with care to patients with a recent history of stroke or cerebrovascular accident, because these conditions cause widening of the cerebral arteries.
Peripheral vasodilating agents may cause dizziness, headache, weakness, tachycardia, flushing, postural hypotension, dysrhythmias, confusion, severe rash, nervousness, tingling, and sweating. Some side effects disappear within a few weeks if they are mild and if the patient can keep taking the medication.
Drug Interactions
Nitrates increase the effects of atropine-like drugs and tricyclic antidepressants and decrease the effects of all choline-like drugs. The action of anticholinergic drugs and antihistamines may be made stronger. Nitrates should not be taken at the same time as prazosin because of the possibility of a significant interaction. Taking alcohol, beta blockers, antihypertensives, narcotics, and vasodilators with nitrates and nitrites (especially amyl nitrite) may produce severe hypotension (low blood pressure) and cardiac collapse. Nitrates may antagonize (interfere with) the vasopressor actions of sympathomimetic drugs. A cold environment or the use of tobacco reduces the action of nitroglycerin.
The action of peripheral vasodilating agents is stronger if used with antihypertensives and alcohol and may cause hypotension.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient. Ask about heart disease, other health problems, the possibility of pregnancy, allergies, smoking, and whether the patient is taking other drugs that may cause interactions. Get a full description of the angina pain.
n Diagnosis
What other problems does this patient have that may interfere with treatment? For example, is the patient overweight? Does he or she smoke? What is the patient’s understanding of what is happening? What is the patient’s nutritional status and what dietary habits does the patient have? Is there any problem with the patient’s kidneys?
n Planning
Many times angina may be reduced or controlled if the patient makes lifestyle changes. This might include stopping smoking, limiting alcohol, limiting salt (sodium), increasing physical exercise, losing weight, eating a balanced diet rich in fruits and vegetables with lots of potassium and magnesium, avoiding dietary saturated fats, reducing stress, and treating other diseases such as hypertension and hyperlipidemia. Some patients who have the coronary arteries blocked may be candidates for surgery (coronary arterial bypass grafts or percutaneous transluminal coronary angioplasty) to reduce the symptoms. Medications are also an important part of treatment.
In reviewing the medicines that might be ordered, refer to the information in Table 15-1, which compares the action of various nitrate products. Nitrates are readily absorbed under the tongue, from nasal spray, through the skin, and orally, but products taken orally are rapidly changed in the liver to inactive products. The half-life for nitroglycerin given sublingually (under the tongue) is only 1 to 4 minutes. Newer forms of the medication can be applied directly to the skin or used as a patch, allowing nitrates to pass directly into the bloodstream, thus reaching the heart before being destroyed by the liver.
![]() Table 15-1
Table 15-1
Comparison of Nitrate Products
| PRODUCT | ONSET | DURATION | PREPARATION |
| Agents for Acute Angina | |||
| Amyl nitrate (Vaporole) | Short-acting 10-30 seconds; repeat 3-5 minutes | Inhalation | |
| isosorbide dinitrate (Dilatrate SR, Isordil, Sorbitrate, Titradose) | 2-3 min | 1-2 hr | Sublingual/chewable May take 5-10 minutes before activities that may cause pain. Take every 5 minutes × 3 doses in 15 minutes for acute pain. |
| nitroglycerin |
1-3 min | 3-5 min | Sublingual |
| 1-2 min | 4-6 hr | Transmucosal | |
| Immediately | 5-10 min | Intravenous, translingual | |
| Agents for Angina Prophylaxis | |||
| isosorbide dinitrate | 45-60 min | 8 hr | Oral |
| Slow | 12 hr | Sustained release, PO | |
| isosorbide mononitrate (Ismo, Imdur, Monoket) | 45-60 min | 6 hr | Oral, sustained release |
| nitroglycerin |
24-45 min | 3-8 hr | Sustained release, PO |
| 30-60 min | 3-7 hr | Topical ointment | |
| 30-60 min | 8-10 hr | Transdermal Patch. Remove for 12 or 24 hr to reduce development of tolerance. | |
| Ranolazine (Ranexa ER) | Variable | Variable | Extended release product. Do not take with grapefruit. |
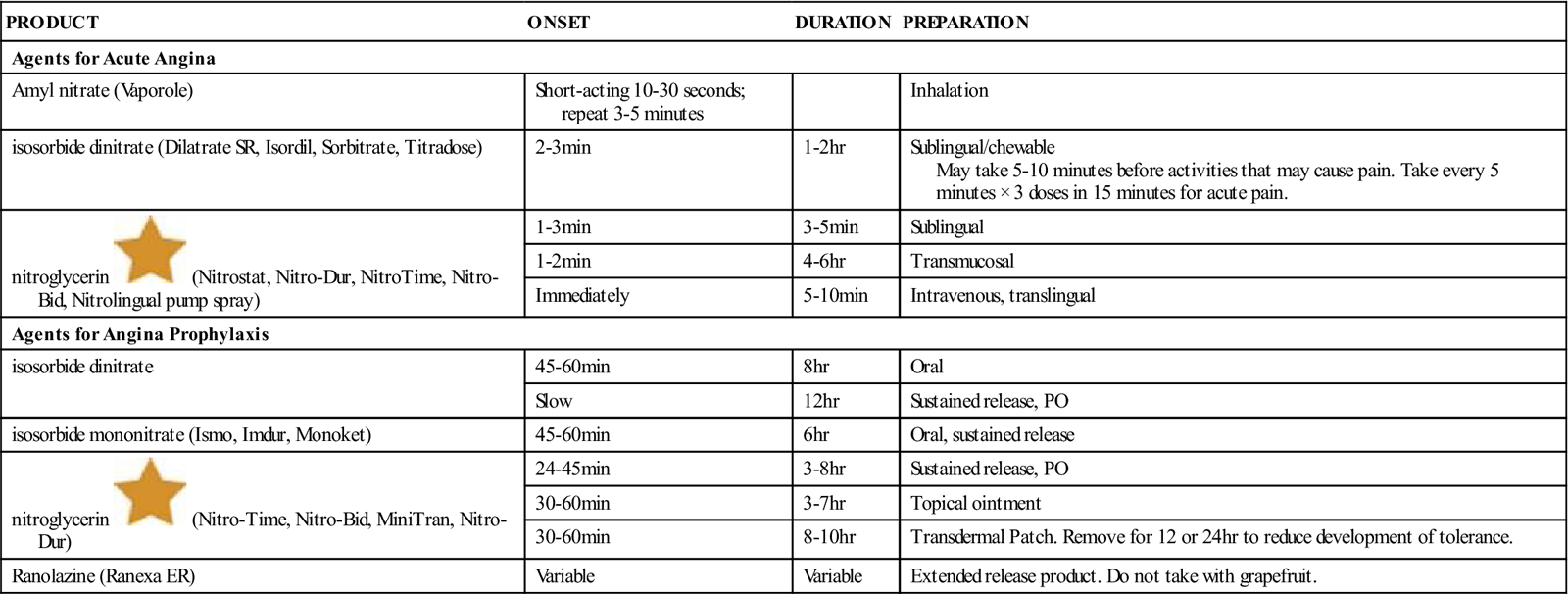
PO, By mouth.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Implementation
Review Chapter 10 for the ways to administer different types of nitroglycerin products.
Nitrate headaches often go away with a lower dose and analgesics. As the patient continues to take the nitroglycerin product, these headaches will gradually stop.
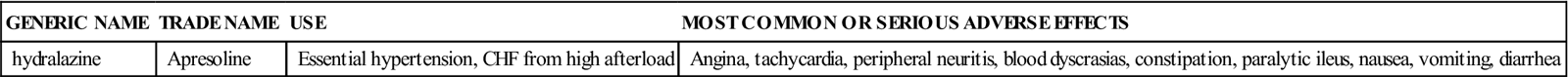
Table 15-2 provides a list of peripheral vasodilating medications.
![]() Table 15-2
Table 15-2
Peripheral Vasodilating Medications
| GENERIC NAME | TRADE NAME | USE | MOST COMMON OR SERIOUS ADVERSE EFFECTS |
| hydralazine | Apresoline | Essential hypertension, CHF from high afterload | Angina, tachycardia, peripheral neuritis, blood dyscrasias, constipation, paralytic ileus, nausea, vomiting, diarrhea |
n Evaluation
The drug should be stopped if blurred vision or dry mouth occurs. If the patient says that some of the sustained-release medication is being passed in the stool, it is likely that food moves through the patient’s GI tract too fast to allow the drug to be absorbed. Such patients may need to switch to transdermal or sublingual medication.
Older adult patients may have postural hypotension with these drugs and need to be watched very carefully. They may need to have someone with them when they take the medication.
The patient must learn the uses and limits of the nitrate being taken, understand the schedule of when to take the drug, and be given information about when to call for help if chest pain does not go away after taking the drug. There are many important things to learn about giving this medication by its various routes. A person who has been using a nitrate for a long time should not stop taking the drug suddenly as this may cause more angina.
n Patient and Family Teaching
Tell the patient and family the following:
• The medication should be taken on an empty stomach when possible.
• The patient must not drink alcoholic beverages while taking nitrate products.
• The topical ointment tube should be kept tightly closed. Store nitroglycerin in the refrigerator.
• This medication must be kept out of the reach of children and others for whom it is not prescribed.
Antidysrhythmics
Overview 
A person with heart disease or other diseases, or nutritional or congenital problems that may affect heart muscle, is at risk of developing irregular beating of the heart, or cardiac dysrhythmia. Because the term dysrhythmia (irregular rhythm) explains what happens to the patient better than the older term arrhythmia (without rhythm), it is now commonly used. Dysrhythmias may be fast or slow, with an irregular or regular pattern. The most common causes of dysrhythmias are irritation to the heart tissue after the patient has suffered an MI, fluid and electrolyte imbalances, problems with diet, hypoxia (reduced blood oxygen), and reactions to drugs.
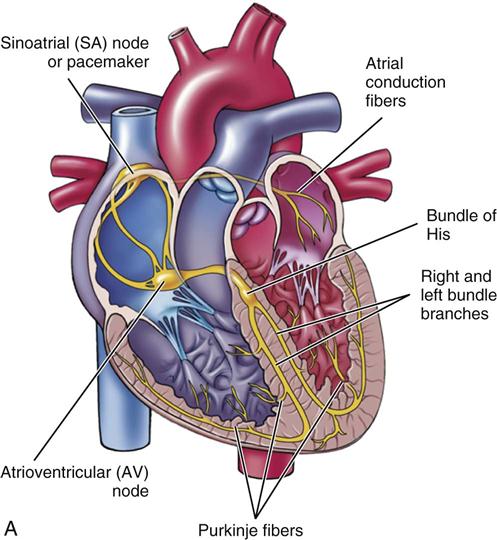
The middle layer of the heart wall, or myocardium, is made up of special muscle cells. These muscle cells work together under the direction of a special group of nerve fibers called the pacemaker, which located in the sinoatrial (SA) node. The pacemaker cells direct the rest of the cardiac cells by sending electrical impulses through a special nerve system known as the cardiac conduction system. These impulses cause atrial and ventricular contraction (pumping). A person’s heart rate is governed by how fast the pacemaker cells direct the heart to pump and by how fast this information is spread through the heart. The usual path of information flow begins in the SA node, passes through the atrium to the atrioventricular (AV) node, through the bundle of His, through the right and left bundle branches, and out through the Purkinje fibers of the myocardium. When the electrical impulse has spread along this pathway, the heart will contract, forcing blood out into the arteries. After a brief rest, the cycle will begin again. This is called normal sinus rhythm.
The electrical message directing the heart to contract depends on a special balance of electrolytes (such as calcium and sodium) in the cardiac tissues and on good function of the cardiac conduction system. This electrical message is what is recorded on the electrocardiogram (ECG). Figure 15-5 illustrates the conduction system of the heart and the ECG pattern that it makes.
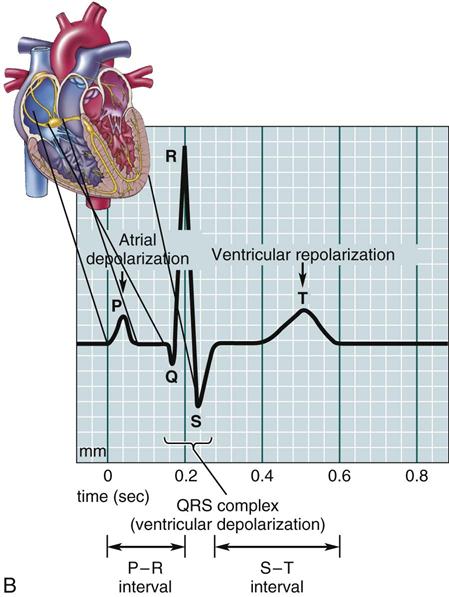
When the cells in the conduction system do not have enough oxygen or are destroyed or damaged through disease, or when the electrolytes are not present in the right balance, irregular heart action is found. Some patients may describe very slow, regular or irregular heartbeats; some patients may have fast, irregular heartbeats. Some individuals may only feel a little dizzy or report that their heart has “skipped a beat.” Sometimes patients have no symptoms; sometimes the symptoms are life threatening. The nurse may feel an irregular pulse or hear the irregularity with the stethoscope. The exact type of irregular rhythm can only be determined by taking an ECG. The dysrhythmia is often classified by its location and type of rhythm abnormality produced, for example, atrial tachycardia. Outside the hospital, some patients may wear a heart monitor strapped to their chest, or inside the hospital, they may be placed in a coronary care unit so they may be closely watched. The goal of any treatment plan or therapeutic regimen is for the patient’s heart to regain a normal rate and rhythm.
Research has confirmed that some individuals have a gene that places them at risk for sudden death. The problem occurs when there is lengthening or prolongation of the QT interval measured by the ECG. The problem is known as Long QT (LQT) Syndrome and is a disorder of cardiac repolarization caused by alterations in the transmembrane potassium and sodium currents. Congenital LQT is a disease of transmembrane ion-channel proteins. Six different genes might cause this problem and many members of a family may have the same problem. Single cases of the disease occur as a result of spontaneous gene mutations. The acquired causes of LQT include drugs, electrolyte imbalance, marked bradycardia, cocaine, organophosphorus compounds, subarachnoid hemorrhage, myocardial ischemia, protein sparing fasting, autonomic neuropathy, and human immunodeficiency virus disease. There are a great many drugs which might provoke this problem in at risk patients, including many cardiac and central nervous system (CNS) drugs. A complete list of drugs which these patients should not be prescribed may be found at www.sads.org/living-with-sads/Drugs-to-Avoid. When studying about drugs or reading package inserts, the nurse should be aware that some products are found to prolong the QT interval. These individuals often require internal defibrillators to be inserted into their heart.
Action 
Many dysrhythmias require placing of a pacemaker, administration of an electric shock, or other nonpharmacologic therapy. But medications do play a role. Medications that act to make the heart rhythm normal are called antidysrhythmic medications. They act on the individual cells of the heart. Each individual heart cell might be thought of as a gun. With each heartbeat, the cardiac muscle cell (gun) has to get ready to shoot (fire), fire, and then reload. As one cell discharges (fires), it triggers the next cell to discharge. After passing the electrical message to the next cell, each conduction cell must rest (reload) before it can pass another electrical signal. Antidysrhythmic drugs affect the cells that are beating (firing) irregularly by acting on each of these phases of cell activity. Dysrhythmic medications are classified by the stage at which they affect the cellular action potential. These include:
Uses
The cause of the dysrhythmia will determine which drug will be most effective in correcting it. The two basic actions within the heart that cause dysrhythmias are: (1) increased sensitivity of electrical cells in the heart, resulting in irregular or early ectopic beats (the cell fires before it should); and (2) electrical activity moving through abnormal conduction pathways (the trigger that causes the cell to fire does not always work properly). For example, a block of the sinus or AV node pacemakers force the heart to use a different pathway than usual. The amount of medication that can be given for these dysrhythmic drugs has a very small range. If too much is given, the dose may be toxic and add to the problems of the heart.
There are now many dysrhythmic drugs on the market. Only a few of the most commonly used drugs are described here. Two drugs that are often used to treat rapid and irregular dysrhythmias are quinidine and procainamide. These drugs are chemically different, but both act to quiet the myocardial cells and make them less excitable and less likely to fire. This not only decreases the heart rate but also stops some of the extra or irregular beats. These drugs were once the mainstay of dysrhythmia therapy but new drugs now have less significant side effects.
Bretylium is another drug that used to be in greater use to slow the conduction rate of the electrical impulse in the ventricular muscle. This drug also acts to slow the release of norepinephrine, a powerful chemical in the cardiac cells, so the heart muscle beats more slowly.
Disopyramide slows the depolarization of the cardiac cells. Depolarization is the movement of electrolytes into and out of the cell as it gets ready to send another electrical message. Under the influence of disopyramide, the heart rate is slowed because each cell is slower in recovering from sending the message to the next cell (the reloading time takes longer).
Lidocaine IV is a drug that was formerly widely used. The electrical impulse sent to the cardiac muscle must be of certain strength, or it cannot pass along the conducting nerve fibers. Lidocaine increases the strength of the impulse. A drug that affects the rate of rhythmic movements, such as the heartbeat, is called a chronotropic drug. A dromotropic drug influences the velocity (speed) of the passage of an electrical impulse in nerve or cardiac muscle fibers.
A diseased heart may have many electrical impulses trying to move at the same time, but some impulses are very weak. By increasing the strength the impulse must reach before it may be conducted, many weak impulses will be screened out, and the overall heart rate will be slower.
Adenosine is a powerful drug that slows the conduction through the AV node and decreases how rapidly the SA node will fire. An IV injection to end serious atrial tachycardia may cause the heart to stop beating for several seconds when a very rapid heartbeat is changed to normal (normal sinus rhythm). Although this drug has only a 10-second half-life, this pause in the heart beat is very upsetting for patients, who often refuse to take it more than once. Some institutions may use benzodiazepines at the same time to help the patients relax during this procedure.
Digoxin is used primarily to treat heart failure but also plays a role in treating fast dysrhythmias such as atrial fibrillation or tachycardia. It slows the heart rate by slowing how fast the SA node fires and slowing conduction through the AV node. It also strengthens the contraction of the heart. Toxic levels of this medication also cause dysrhythmias. (See cardiotonics in a later section.) Other drugs that affect heart activity are the beta-adrenergic blockers, of which propranolol (Inderal) and metoprolol (Lopressor) are the most well known. Drugs in this category act very much like quinidine, but they also decrease the response of the heart muscle to epinephrine and norepinephrine (other chemical neurotransmitters) by blocking the stimulation of the heart’s beta receptors. (Again, the reloading of the cell is affected.)
It is clear that many of the antidysrhythmic drugs are so powerful that they should only be used in critical care units where the patient may be closely monitored. Some of these drugs are given as an IV injection followed by an IV solution filled with the medication. As the patient’s condition becomes more stable, some drugs may be changed to other antidysrhythmic drugs that are better for long-term therapy.
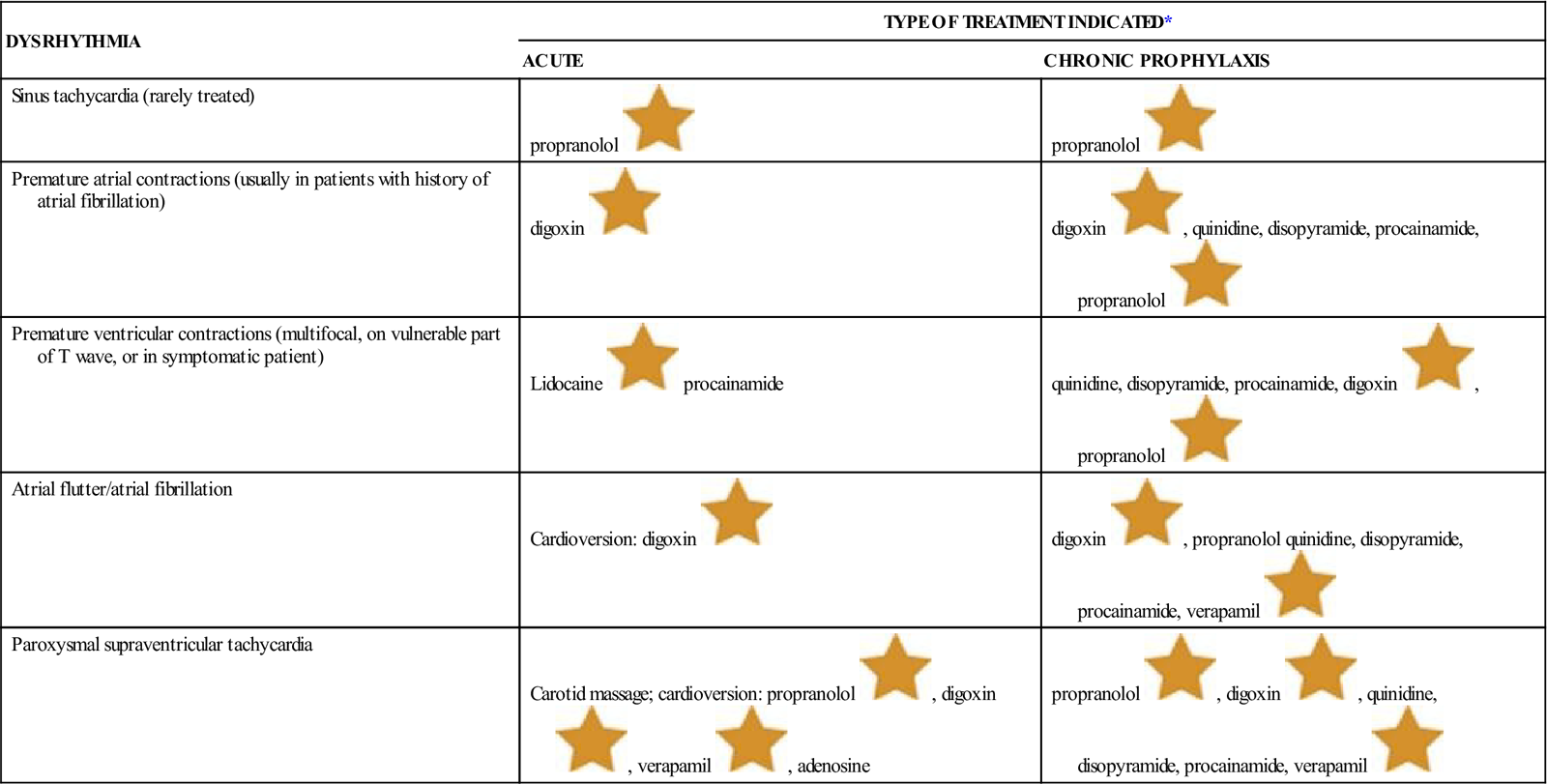
Table 15-3 lists drugs that may commonly be used in the treatment of acute and chronic dysrhythmias.
![]() Table 15-3
Table 15-3
Acute Treatment and Chronic Prophylaxis of Dysrhythmias
| DYSRHYTHMIA | TYPE OF TREATMENT INDICATED* | |
| ACUTE | CHRONIC PROPHYLAXIS | |
| Sinus tachycardia (rarely treated) | propranolol |
propranolol |
| Premature atrial contractions (usually in patients with history of atrial fibrillation) | digoxin |
digoxin |
| Premature ventricular contractions (multifocal, on vulnerable part of T wave, or in symptomatic patient) | Lidocaine |
quinidine, disopyramide, procainamide, digoxin |
| Atrial flutter/atrial fibrillation | Cardioversion: digoxin |
digoxin |
| Paroxysmal supraventricular tachycardia | Carotid massage; cardioversion: propranolol |
propranolol |
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Adverse Reactions
Most drugs given to control dysrhythmias may also cause other dysrhythmias. All patients receiving these drugs should have their heart carefully monitored by ECG for any change.
Quinidine is an older drug that is still in use in some hospitals and parts of the world, although it has many adverse effects. It may cause cardiac dysrhythmias, hypotension, diarrhea, tinnitus, headache, vertigo, confusion, delirium, disturbances in vision, and abdominal pain. Toxic effects are called cinchonism, and the patient will complain of tinnitus, light-headedness, headache, fever, vertigo, nausea, vomiting, and dizziness. The first time the patient takes the medicine, a test dose should be given to check for quinidine syncope—a condition in which the body reacts to quinidine by reducing blood flow to the brain, producing syncope (light-headedness and fainting), loss of consciousness, and sometimes death.
See Table 15-3 for common adverse effects.
Drug Interactions
Quinidine’s effect is increased by potassium and is reduced by hypokalemia. Verapamil actions are stronger when used at the same time as digitalis and beta blockers. Beta blockers have many interactions with other drugs, and the nurse should read about every other drug the patient is taking when a beta blocker is prescribed.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn everything possible about the patient’s health history, including any drug allergies, other drugs being taken that may cause drug interactions, and other medical problems, including factors such as hypoxia (reduced blood oxygen), acid-base imbalance, increased or decreased potassium, or drug toxicity. It is good practice to always take an apical heart rate with any patient that may have an arrhythmia by placing the stethoscope in the left chest cardiac area. Some irregular heart rates are very weak and are difficult to accurately feel with a radial pulse.
n Diagnosis
Does the patient have other health problems that will affect therapy? Does the patient drink lots of caffeine? Smoke? Exercise? Is the patient overweight?
n Planning
An ECG should be obtained before medications are started. This will determine the status of the heart before treatment so that changes can be seen if treatment is helpful.
n Implementation
Vital signs must be taken before giving any antidysrhythmic medication. The nurse often has the responsibility of monitoring any changes that might develop in blood pressure or pulse while initial thrapy is given. Hospitalized patients often continue their antidysrhythmic medications when they go home, so the nurse might take advantage of every opportunity to teach patients about these medications and be prepared to answer questions.
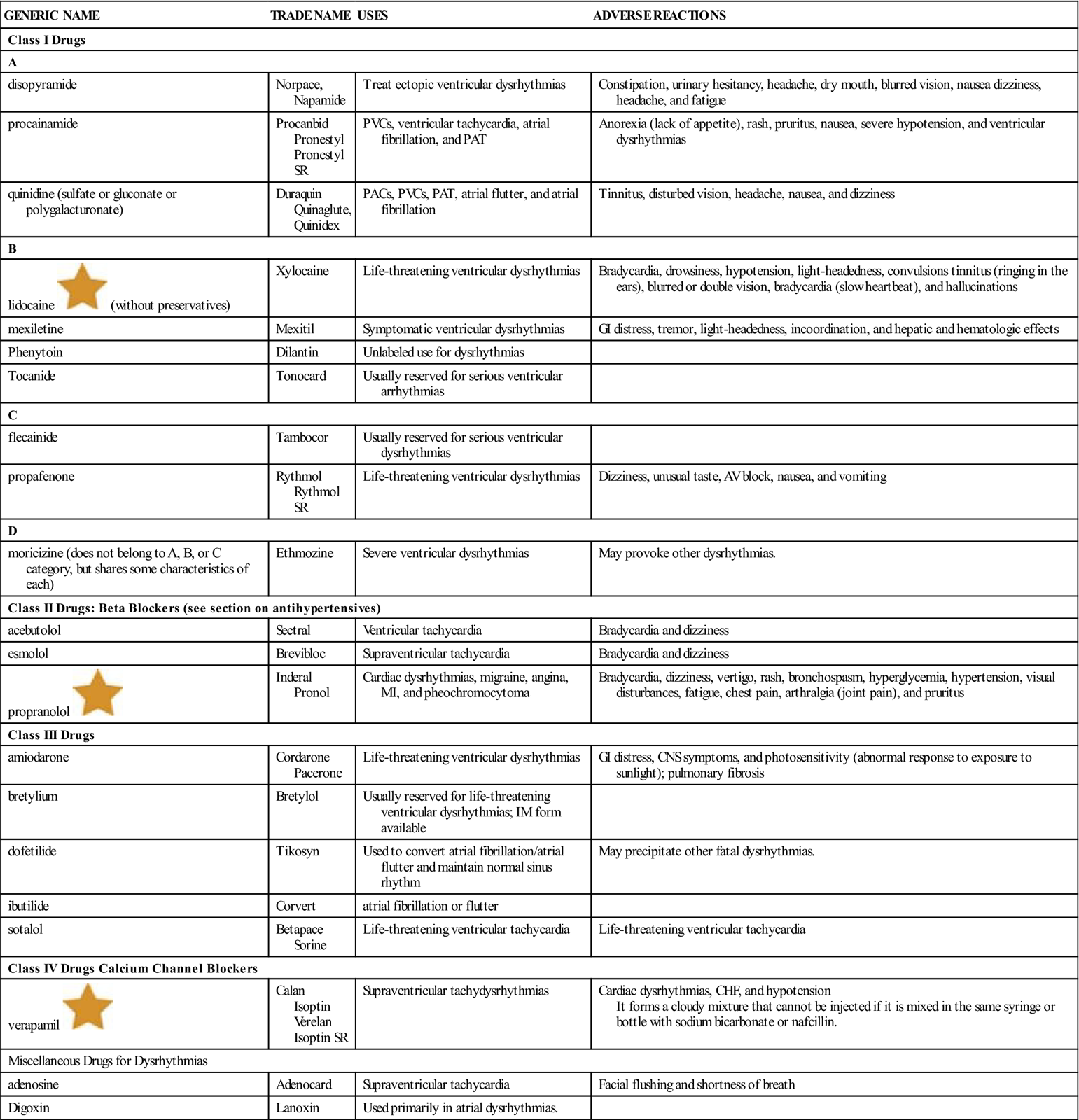
Table 15-4 presents information about the antidysrhythmics.
![]() Table 15-4
Table 15-4
| GENERIC NAME | TRADE NAME | USES | ADVERSE REACTIONS |
| Class I Drugs | |||
| A | |||
| disopyramide | Norpace, Napamide | Treat ectopic ventricular dysrhythmias | Constipation, urinary hesitancy, headache, dry mouth, blurred vision, nausea dizziness, headache, and fatigue |
| procainamide | Procanbid Pronestyl Pronestyl SR |
PVCs, ventricular tachycardia, atrial fibrillation, and PAT | Anorexia (lack of appetite), rash, pruritus, nausea, severe hypotension, and ventricular dysrhythmias |
| quinidine (sulfate or gluconate or polygalacturonate) | Duraquin Quinaglute, Quinidex |
PACs, PVCs, PAT, atrial flutter, and atrial fibrillation | Tinnitus, disturbed vision, headache, nausea, and dizziness |
| B | |||
| lidocaine |
Xylocaine | Life-threatening ventricular dysrhythmias | Bradycardia, drowsiness, hypotension, light-headedness, convulsions tinnitus (ringing in the ears), blurred or double vision, bradycardia (slow heartbeat), and hallucinations |
| mexiletine | Mexitil | Symptomatic ventricular dysrhythmias | GI distress, tremor, light-headedness, incoordination, and hepatic and hematologic effects |
| Phenytoin | Dilantin | Unlabeled use for dysrhythmias | |
| Tocanide | Tonocard | Usually reserved for serious ventricular arrhythmias | |
| C | |||
| flecainide | Tambocor | Usually reserved for serious ventricular dysrhythmias | |
| propafenone | Rythmol Rythmol SR |
Life-threatening ventricular dysrhythmias | Dizziness, unusual taste, AV block, nausea, and vomiting |
| D | |||
| moricizine (does not belong to A, B, or C category, but shares some characteristics of each) | Ethmozine | Severe ventricular dysrhythmias | May provoke other dysrhythmias. |
| Class II Drugs: Beta Blockers (see section on antihypertensives) | |||
| acebutolol | Sectral | Ventricular tachycardia | Bradycardia and dizziness |
| esmolol | Brevibloc | Supraventricular tachycardia | Bradycardia and dizziness |
| propranolol |
Inderal Pronol |
Cardiac dysrhythmias, migraine, angina, MI, and pheochromocytoma | Bradycardia, dizziness, vertigo, rash, bronchospasm, hyperglycemia, hypertension, visual disturbances, fatigue, chest pain, arthralgia (joint pain), and pruritus |
| Class III Drugs | |||
| amiodarone | Cordarone Pacerone |
Life-threatening ventricular dysrhythmias | GI distress, CNS symptoms, and photosensitivity (abnormal response to exposure to sunlight); pulmonary fibrosis |
| bretylium | Bretylol | Usually reserved for life-threatening ventricular dysrhythmias; IM form available | |
| dofetilide | Tikosyn | Used to convert atrial fibrillation/atrial flutter and maintain normal sinus rhythm | May precipitate other fatal dysrhythmias. |
| ibutilide | Corvert | atrial fibrillation or flutter | |
| sotalol | Betapace Sorine |
Life-threatening ventricular tachycardia | Life-threatening ventricular tachycardia |
| Class IV Drugs Calcium Channel Blockers | |||
| verapamil |
Calan Isoptin Verelan Isoptin SR |
Supraventricular tachydysrhythmias | Cardiac dysrhythmias, CHF, and hypotension It forms a cloudy mixture that cannot be injected if it is mixed in the same syringe or bottle with sodium bicarbonate or nafcillin. |
| Miscellaneous Drugs for Dysrhythmias | |||
| adenosine | Adenocard | Supraventricular tachycardia | Facial flushing and shortness of breath |
| Digoxin | Lanoxin | Used primarily in atrial dysrhythmias. | |
AV, Atrioventricular; CHF, congestive heart failure; CNS, central nervous system; GI, gastrointestinal; IM, intramuscular; MI, myocardial infarction; PAC, premature atrial contraction; PAT, paroxysmal atrial tachycardia; PVC, premature ventricular contraction.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
If the patient’s heart is not being watched with a cardiac monitor, the results from ECGs must be closely followed to see any changes. Electrolyte levels and other laboratory data should also be obtained.
n Patient and Family Teaching
Antihyperlipidemics
Overview
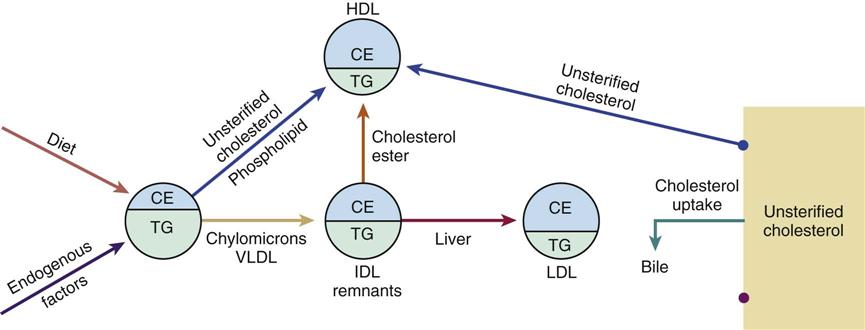
Cholesterol and other fatty acids are called lipids. The body needs a certain amount of cholesterol and triglycerides, which are both normal and vital parts of blood plasma. Like other lipids, they are not soluble in liquid, so they are carried in the plasma by linking to lipoproteins (albumin and globulins). Lipoproteins are described by how thick or dense they are (“high-density lipids” and “low-density lipids”). The four major types of lipoproteins are as follows:
Chylomicrons and VLDLs are seen as triglyceride-rich lipoproteins, whereas LDLs and HDLs are viewed as cholesterol-rich lipoproteins. These two lipoproteins differ in several respects, including their cholesterol transporting activities. Simply stated, LDLs move cholesterol from the liver to peripheral tissues, and HDLs remove cholesterol from the periphery and transport it to the liver. Figure 15-6 shows the normal physiology of lipoprotein transport. Chylomicrons are the largest and least dense of the lipoproteins; as size decreases and density increases, the next type is the VLDLs (pre-beta lipoproteins), then the intermediate-density lipoproteins (IDLs, or broad beta lipoproteins), then the LDLs (beta lipoproteins), and finally the HDLs (alpha lipoproteins, the smallest and most dense).
The high blood lipid levels may be caused by problems in moving lipids (lipid transport) or chemical breakdown (metabolism) of lipids. Hyperlipidemia is the term used to describe high levels of lipoproteins in the blood. This may mean high amounts of triglycerides, high amounts of cholesterol, or both. These high levels may be classed according to Types I through V. Some of these types are genetic; some respond to drug or dietary treatment; and some are more likely to cause atherosclerosis. It is important to determine the type of hyperlipidemia the patient has (Figure 15-7),
Atherosclerosis in the coronary arteries causes coronary heart disease (CHD). The coronary arteries that feed and nourish the heart become smaller because the inner wall of the arteries are narrowed as they fill with plaques, or patches of atherosclerotic tissue. Although the narrowing of the coronary artery may decrease the blood supply to the heart, it is only when a plaque is broken or torn, and platelets cling to the torn area and produce a blockage, that the blood supply is decreased enough to cause a heart attack. When the heart does not get enough blood to its muscle cells, those cells experience pain (angina) and then those cells die. This is called myocardial infarction (MI), or heart attack. When the physician or nurse practitioner looks in the patient’s eyes with the ophthalmoscope, they may see plaque in the linings of the arteries in the eyes. If there is plaque in the arteries of the eyes, then there are likely atherosclerotic plaques throughout all the arteries in the body and might be present before the patient shows any symptoms. These areas of plaque that lead to the lack of oxygen in the blood may also lead to cerebrovascular disease (including stroke), peripheral ischemia (lack of oxygenated blood in the legs caused by problems in the circulation of the legs), and renovascular hypertension (high pressures and damage in the kidneys). Research suggests that high blood LDL cholesterol levels lead to CHD. There is an opposite link between HDLs and CHD risk—that is, high levels of HDL cholesterol are viewed as protecting the patient against CHD. This is why LDLs are sometimes called “bad cholesterol” and HDLs are called “good cholesterol.” Evaluation of LDL and HDL levels is of primary importance, because research has now shown that lowering serum lipids or cholesterol can help reduce the risk of atherosclerotic disease. There are many people with high lipid and cholesterol levels that place them at risk for CHD. These lipid levels can often be lowered through diet, exercise, and lifestyle changes and the use of medications.
Guidelines for the diagnosis and treatment of hyperlipidemia are issued and regularly updated by the National Cholesterol Education Program. These guidelines emphasize the following:
Many times activity and diet will help achieve the proper blood lipid levels. The recommended laboratory values for all patients include:
• Total cholesterol level less than 200 mg/dL
• LDL cholesterol less than 100 mg/dL
Both exercise and diet therapy are important and should always be a part of the treatment plan. If changing the diet and exercise alone does not produce the needed changes, drug therapy may also be offered. Five classes of drugs are used to treat hyperlipidemia: hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, the fibric acid derivatives, bile acid sequestrants, selective cholesterol absorption inhibitors, and niacin. A list of the usual diet and drug therapy regimens in the various types of hyperlipidemias is provided in Table 15-5.
Table 15-5
Diet and Drug Therapy for the Hyperlipidemias
| TYPE | DIET | DRUGS |
| I | Low fat; no other restrictions | None is effective |
| IIa | Low cholesterol, low in saturated fats; increased intake of polyunsaturated fats | HMG-CoA reductase inhibitors, bile acid sequestrants, nicotinic acid |
| IIb | Same as above | HMG-CoA reductase inhibitors, bile acid sequestrants, gemfibrozil, nicotinic acid, clofibrate, fenofibrate |
| III | Low cholesterol, low calorie, low in saturated fats; high protein | Nicotinic acid, gemfibrozil, clofibrate, fenofibrate |
| IV | Low carbohydrate, low alcohol, low cholesterol, low calorie; maintain protein intake | Gemfibrozil, nicotinic acid, clofibrate, fenofibrate |
| V | Low fat, low carbohydrate, low alcohol; high protein | Gemfibrozil, nicotinic acid, clofibrate, fenofibrate |
Action
HMG-CoA Reductase Inhibitors or Statins
The HMG-CoA reductase inhibitors are the first choice drugs used to treat hyperlipidemia. They are the most costly drugs for treating hyperlipidemia, but patients also tolerate them best, and they are highly effective at lowering LDL levels. The ability of the six drugs in this class to lower LDL levels can be roughly ranked in the following order, with the most powerful drug first: rosuvastatin, atorvastatin, simvastatin, pravastatin, lovastatin, and fluvastatin. Adverse effects are similar for all six of these agents. A switch from one drug to another may be needed if adverse reactions occur. Liver function tests (LFTs) should be monitored in patients taking these products.
Fibric Acid Derivatives
Gemfibrozil and fenofibrate are the preferred drugs of this class because they are more effective and have fewer adverse effects compared with some other drugs. Both are highly effective at lowering triglycerides and increasing HDL levels, but have little effect on lowering LDL levels. Gemfibrozil and fenofibrate are well tolerated but can cause liver toxicity and cholelithiasis (gallstones).
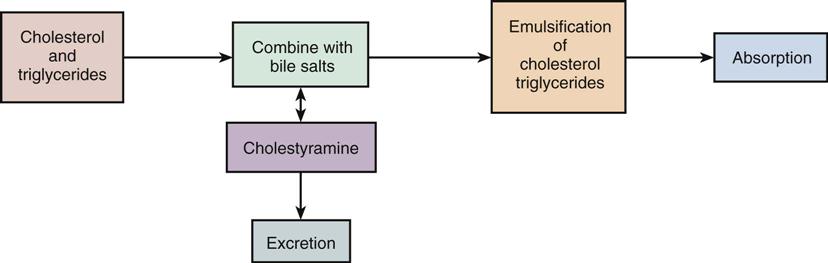
Bile Acid Sequestrants
These drugs increase cholesterol excretion and reduce LDL levels. They do this by forming an insoluble compound with bile salts and thus increasing bile loss through the feces (stool). This loss of bile, which would normally be recycled through the liver and bowel, causes increased oxidation of cholesterol to form bile. This results in a decrease in LDL plasma levels and a decrease in serum cholesterol levels (Figure 15-8). These drugs are usually used to treat type II hyperlipoproteinemia and are mostly used for lowering LDL levels. They are the only antihyperlipidemics that increase triglyceride levels. Patients may not be willing to use these drugs because of adverse GI effects such as constipation, bloating, and nausea. Both of these resin agent drugs are equally effective. Because they remain in the bowel and are not absorbed, there is no need to do tests to watch for adverse effects. They may also bind to other drugs and interfere with their absorption.
Niacin or Nicotinic Acid
Niacin is one of the most effective antihyperlipidemics at lowering triglyceride levels and increasing HDL levels and is similar to the bile acid sequestrants in its ability to lower LDL levels. The main limit to the use of niacin is its adverse effect of flushing (red color in the face and neck), although patients generally develop an ability to tolerate this problem with continued use. Flushing occurs shortly after the drug is taken and can be reduced by taking aspirin (30 minutes before) and increasing the niacin dosage very slowly over 3 to 4 weeks from 500 to 1000 mg three times daily. Niacin reduces glucose tolerance and may cause hyperuricemia (high uric acid levels), so it should be used with caution in patients with diabetes or gout. It remains the cheapest antihyperlipidemic and is probably underused in practice.
Selective Cholesterol Absorption Inhibitors
Ezetimibe is the first agent in this new category of drugs. This drug stays in the intestinal wall and acts on the intestinal epithelial cells to partially limit the absorption of cholesterol from food and from other sources in the body.
Adverse Reactions
All these medications may affect liver function, and the physician will be monitoring LFTs regularly. Also be aware of the following:
Drug Interactions
Because these drugs act by binding, giving the drug with other medications may cause those drugs to be bound to the product. Cholestyramine, colestipol, and gemfibrozil may make warfarin anticoagulants more effective. Therefore, the health care provider should make sure the patient knows when to take the medications and the nurse should help the patient remember that they can’t all be taken at the same time.
Normal absorption of fat-soluble vitamins may be reduced with bile acid sequestrants, and the patient may show symptoms of vitamin deficiency if the dosage is at a high level or the drugs are taken for a long time. Watch for bleeding problems that may result from hypoprothrombinemia caused by vitamin K deficiency. Normal fat digestion may be disturbed. Some patients, especially very young or small patients, are more likely to develop hyperchloremic acidosis because of the chloride anion exchange.
These drugs delay or reduce the absorption of many important drugs and hormones. If the patient has been placed on a regular dose of any of these drugs, and then bile acid sequestrant therapy is discontinued, toxic levels of the other drugs may develop. This is especially important to consider in connection with digitalis therapy. These products may also produce mild increases of common electrolytes measured in the blood.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including any allergies, other medications that are being taken that may lead to drug interactions, diet, other things the patient has done to try to reduce cholesterol levels, and the possibility of pregnancy.
n Diagnosis
Does this patient have other problems that will interfere with this therapy? Does the patient have a family history that causes anxiety about early death? Does the patient have problems with exercise, diet, or stress that make it more difficult to follow the treatment plan?
n Planning
Encourage weight reduction when necessary, because obesity increases the risk of cardiovascular damage. The patient must be taught about the long-term nature of this disease and the need for lifelong diet changes. The nurse’s ability to work with the patient, win confidence, be aware of reactions, and provide encouragement will be important in gaining compliance with diet, medication, and lifestyle changes that may save the patient’s life. Frequent return visits to the health care provider will be necessary, so the nurse may have many chances to offer support and reinforcement.
n Implementation
If antihyperlipidemic drugs are taken for a long period, extra or supplemental oral or intramuscular doses of vitamins A, D, and K may be needed.
Table 15-6 provides a summary of antihyperlipidemics.
![]() Table 15-6
Table 15-6
| GENERIC NAME | TRADE NAME |
| HMG-CoA Reductase Inhibitors—“Statins” | |
| atorvastatin Ca |
Lipitor |
| fluvastatin | Lescol |
| lovastatin | Mevacor |
| pravastatin | Pravachol |
| rosuvastatin | Crestor |
| simvastatin | Zocor |
| Fibric Acid Derivatives | |
| gemfibrozil | Lopid |
| fenofibrate | Tricor, Lipofen |
| Bile Acid Sequestrants | |
| cholestyramine | Questran, Prevalite |
| colestipol | Colestid |
| colesevelam | Welchol |
| Niacin | |
| Nicotinic acid (niacin) | Niaspan, Niacor, Niac |
| Selective Cholesterol Absorption Inhibitors | |
| ezetimibe | Zetia |
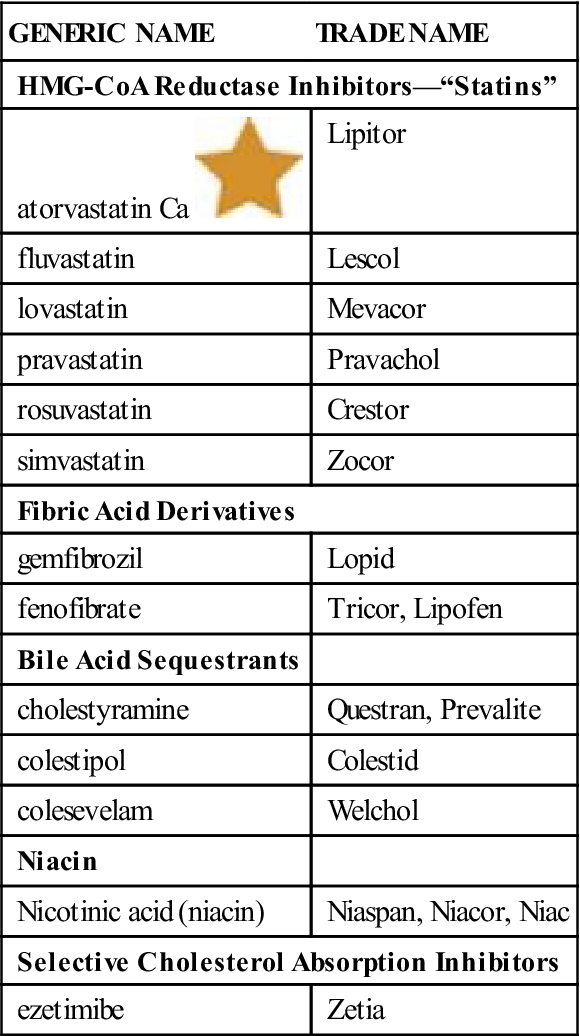
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Statin medications are often taken in the evening as the body makes higher amounts of cholesterol at night. Atorvastatin and rosuvastatin can be taken at any time of the day.
n Evaluation
If the patient takes high doses of niacin it may cause liver damage or gout. Instruct the patient to watch for any symptoms of these problems.
n Patient and Family Teaching
Tell the patient and family the following:
Cardiotonics
Overview 
Cardiotonics are drugs that have a positive inotropic action that make the heart beat stronger and slower. Cardiotonics that make composed of the cardiac glycosides (glycosides are sugar-containing substances made from plants); the phosphodiesterase inhibitors; and dobutamine, which is used occasionally in end-stage heart failure to increase myocardial contractility in a dose-dependent manner. The major cardiac glycoside is the digitalis preparation digoxin that has been used for many years.
Action
All cardiotonics have the following two actions:
The overall result of these two actions is to increase the cardiac output. This is important in hearts that have become weakened and ineffective in pumping because of age or disease and where chronic heart failure has developed.
The normal heart pumps oxygenated blood from the left ventricle out through the body. If the heart is weak, less oxygenated blood can be pumped out with each contraction or beat of the heart.
When cardiac output (the amount of blood pumped out with each heartbeat × the heart beat) decreases, other organs are affected. For example, the brain reacts to receiving less blood by making us feel dizzy, drowsy, or less alert. The lungs are not as effective and the patient may have a productive cough or feel short of breath. The kidneys become less effective at removing waste products, electrolytes, and extra water from the bloodstream. This extra fluid may then pool in the spaces between cells or organs or in other dependent tissues like the hands and feet (edema). The patient may have rapid weight gain because of this fluid. Sometimes the heartbeat itself becomes irregular or too fast. As the body attempts to deal with these changes, over time, the heart may enlarge, develop murmurs or abnormal heart sounds, and the blood pressure may increase or a more rapid heart rate or rhythm may develop. These actions may place further strain on the heart. We call these symptoms of weak or inadequate heart muscle actions chronic or congestive heart failure (CHF) (Table 15-7). The specific therapy for heart failure depends on the severity of the problem causing the failure.
Table 15-7
Symptoms of Congestive or Chronic Heart Failure
| ORGAN AFFECTED | SYMPTOMS |
| Brain | Dizzy, less alert |
| Heart | Enlarged heart, murmurs or abnormal heart sounds, dysrhythmias |
| Lungs | Productive cough, shortness of breath |
| Kidneys | Edema of tissues of hands and feet |
| General | Rapid weight gain, weakness, lethargy (sleepiness) |
Heart failure may also be seen in patients who have had heart attacks or who have high blood pressure or diabetes. Cardiac glycosides have been used to treat heart failure and dysrhythmias for many years. Phosphodiesterase inhibitors (that prevent the inactivation of the intracellular cAMP and cGMP) are used in very ill patients and dobutamine (a beta 1 adrenergic stimulant) is used occasionally. Now angiotensin-converting enzyme (ACE) inhibitors have become the preferred drugs for treating heart failure and protecting the kidneys from damage. Diuretics are also used to relieve symptoms of heart failure by reducing blood volume. Beta-adrenergic blockers are also used in combination with other drugs to slow the progression of heart failure. These other products are discussed in the section on antihypertensive agents. Cardiac glycosides are the drugs that licensed practical and vocational nurses need to know the most about.
Increasing the Strength of Myocardial Contraction
The first action of the cardiotonic drugs is to increase the strength of each heartbeat or the force of the contraction. The stronger heartbeat pumps more blood and increases the cardiac output. This effect of the drug is called a positive inotropic action. As more blood reaches the brain, lungs, kidneys, and other tissues, the signs of inadequate heart action decrease or go away (Figures 15-9 and 15-10).
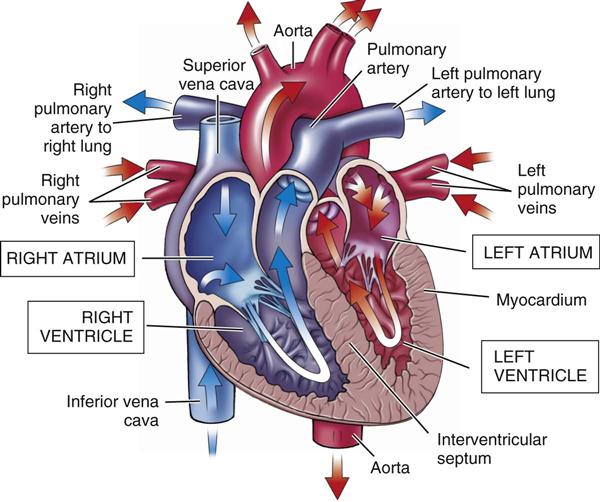
Slowing Heart Rate
The second action of the cardiotonic drugs is to slow the heartbeat. They do this by: (1) slowing down the rate at which the pacemaker in the SA node begins the electrical cycle; and (2) by slowing the rate at which that information is passed through the rest of the heart. (See the discussion of cardiac conduction in the “Antidysrhythmics” section of this chapter.)
Uses
Cardiotonics are used to treat heart failure and rapid or irregular heartbeats such as atrial fibrillation, atrial flutter, and (sometimes outside the hospital) frequent premature ventricular contractions or paroxysmal atrial tachycardia.
Adverse Reactions
Cardiotonics are very powerful and can act as poisons on the heart. Thus a patient taking this drug must be closely watched. Phosphodiesterase inhibitors and dobutamine are given to critically ill hospitalized patients who are always carefully monitored. Older adult patients frequently use digitalis, and they are at particular risk of problems if they use it with other drugs.
Many things may happen that make even a safe dose of digitalis harmful to a patient. When a patient begins to show toxic or harmful reactions from too much medication, digitalis toxicity has developed. The symptoms of digitalis toxicity may begin slowly and are often easy to overlook. These symptoms include dysrhythmias (such as bradycardia, bigeminal VPCs, AV Node block, excessive fatigue, confusion, blurred vision, yellow-green vision, anorexia, nausea, and vomiting) and other vague symptoms.
Treatment of digitalis toxicity begins by stopping the drug and beginning treatment of symptoms, as needed.
Drug Interactions
Beta-adrenergic blocking agents, calcium gluconate, calcium chloride, succinylcholine, and verapamil increase both the therapeutic and the toxic effects of cardiotonics.
Cholestyramine reduces the therapeutic effects.
Any medication that changes the electrolyte balance may also lead to digitalis toxicity.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Before beginning the medication, check the patient for the following:
n Diagnosis
What other problems does this patient have that interfere with therapy? Is the patient overweight? Anxious? Unwilling to accept having cardiac problems?
n Planning
Know about two different types of dosages for patients taking digoxin: 1) the initial digitalizing dose (or loading dose); and 2) maintenance (regular daily) doses. More frequent and higher digitalizing doses are given when a patient begins taking digoxin so that a specific level of medication can be reached in the blood. When the amount of drug in the patient’s blood reaches the desired level, smaller maintenance doses are given once a day to maintain the blood level. How fast the desired drug level is reached is based on the dosage, the diagnosis of the patient, and many other factors.
n Implementation
Before giving each dose of a cardiotonic drug, the apical pulse rate (using a stethoscope and listening to the chest) should be taken for 60 seconds. In an adult, if the apical pulse rate is less than 60, the medication should not be given until the nurse has discussed the low rate with the health care provider and the provider has decided whether it should be given. If there are any symptoms of digitalis toxicity or if the patient’s condition has worsened since the last time the medication was given, the nurse notifies someone in authority if they believe that the dose should not be given, so that a decision might be made.
Table 15-8 gives a summary of cardiotonic medications.
![]() Table 15-8
Table 15-8
| GENERIC NAME | TRADE NAME | USES | SERIOUS ADVERSE REACTIONS |
| Cardioglycoside: | |||
| digoxin |
Lanoxin | Atrial flutter, atrial fibrillation, PAT, CHF | Digitalis toxicity (see text) |
| Phosphodiesterase Inhibitors | |||
| inamrinone | Amrinone | For the short-term management of CHF patients who can be closely monitored and have not responded to digitalis | Ectopic activity of the heart, GI distress, hypersensitivity (allergy) reactions, and hepatotoxicity (damage to the liver) |
| milrinone | Primacor | CHF—short term | Ventricular dysrhythmias |
| Miscellaneous Product | |||
| dobutamine | Beta-1 selective inotrope. Short-term treatment of cardiac decompensation | Ectopic activity, hypotension, tachycardia, and hypertension | |
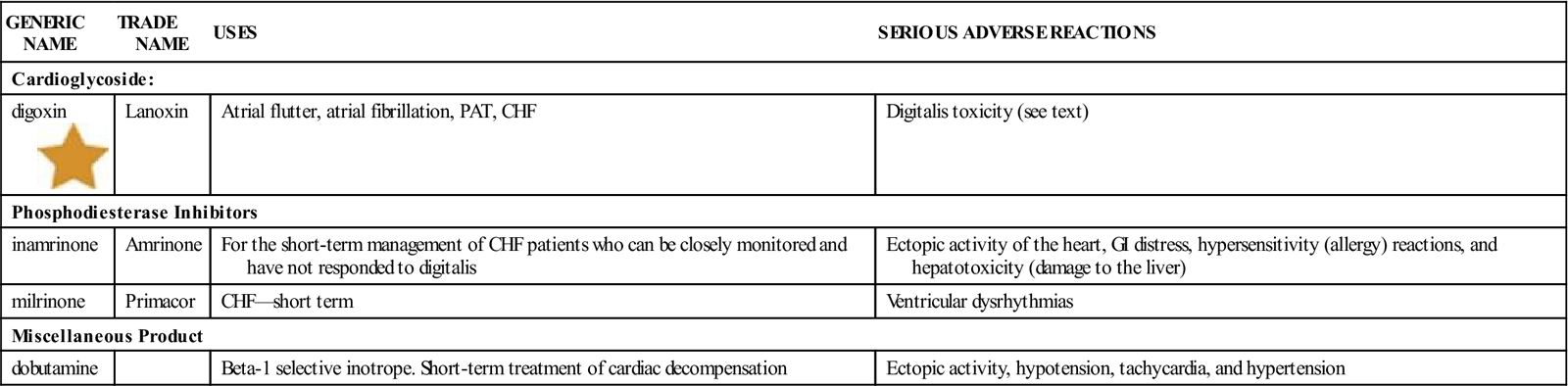
CHF, Congestive heart failure; GI, gastrointestinal; PAT, paroxysmal atrial tachycardia.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
A big risk for patients taking a cardioglycoside is the chance they will get too much drug and have digitalis toxicity. Changes from the first time the patient is seen should be written down in the patient record. Vital signs, including daily weights, are very important to record. Patients with other lung, GI, kidney, or central nervous system (CNS) problems, patients taking many other medications (especially diuretics and electrolytes), and confused patients who are not eating or drinking well are all at risk for digitalis toxicity.
The nurse is alert to any changes in the patient that may suggest the patient has developed digitalis toxicity. The earliest symptom of digitalis toxicity is often extreme fatigue. Almost 100% of patients also experience anorexia. Other signs include nausea and vomiting, difficulty with reading (which may appear as visual alterations such as green and yellow vision, double vision, blurred vision, or seeing spots or halos), headaches, dizziness, weakness, confusion, depression, increased nervousness, and diarrhea. Digitalis toxicity may cause life-threatening dysrhythmias, such as bradycardia, tachycardia, and irregular rhythms.
The health care provider will order blood tests to measure the serum blood digitalis level. The serum level of digoxin that is needed to help the patient (be therapeutic) is 0.5 to 2 ng/mL (nanograms per milliliter), and the toxic serum level is 2.5 ng/mL. Digoxin has a rapid onset and a short length of action.
Episodes of digitalis toxicity may be treated with digoxin immune Fab (Digibind), which has antigen-binding fragments that come from specific antidigoxin antibodies. This product may save lives, but it requires careful monitoring of the patient’s vital signs and potassium levels and special plans for slowly reducing the amount of drug that is given to avoid causing other life-threatening events.
n Patient and Family Teaching
The patient usually continues to take this medication after discharge from the hospital. Tell the family and patient the following:
Antihypertensives, Diuretics, and Other Drugs Affecting the Urinary Tract
Overview
Hypertension is a disorder in which the patient’s blood pressure is elevated above normal values for his or her age. Research has shown that blood pressures of more than 140/90 mm Hg are associated with accelerated vascular damage of the heart, the brain, and the kidneys, leading to an increased risk of early death. Lowering the blood pressure to less than 120/90 mm Hg has been demonstrated to dramatically reduce the chance of MI, stroke, and other target organ damage. Primary hypertension (or essential hypertension) accounts for 80% to 90% of all cases of high blood pressure, but in most cases the cause is unknown. In some cases, high blood pressure results from another disease or other problem and is then called secondary hypertension.
Approximately 40 million people in the United States have hypertension, a disorder that cannot be cured but can be controlled. Risk factors for hypertension include increasing age, black race, male sex, family history of hypertension, obesity, diabetes mellitus, hypercholesterolemia, smoking, and previous history of vascular disease.
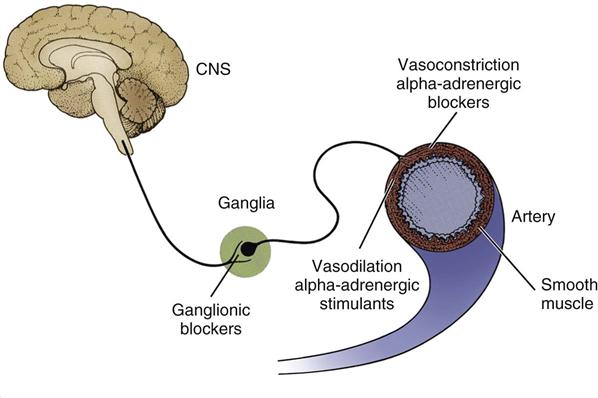
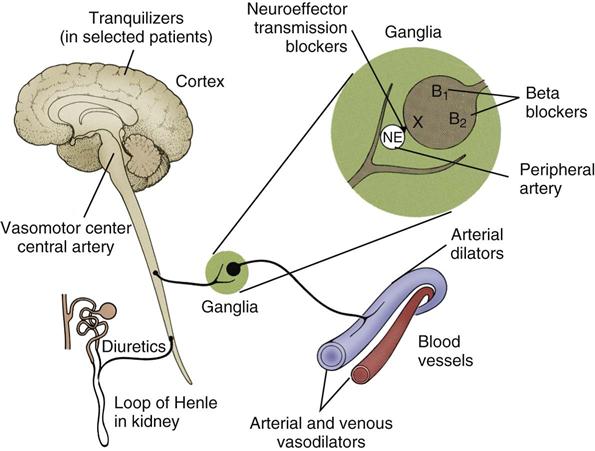
Action
Many types of drugs are available to treat hypertension. The drug selected for use depends on the severity of the disease. The drugs act at many sites in the body and through several different ways (Figure 15-11). These drugs fall roughly into the following five main categories:
Because each of these five drug categories works in a different manner and is also useful in treating problems other than hypertension, the action of each drug category is discussed separately. Figure 15-9 shows the different places where these antihypertensive medications may act.
Many of these drugs can be mixed together to produce a new combination drug with many actions. Some of these products combine potassium-sparing and potassium-losing drugs. These drugs may be good for some patients (they do not need to take so many pills), but the ability to increase or decrease one of the drugs in the combination product to meet the specific needs of a patient is lost.
Diuretics 
The action of all diuretics is to increase fluid loss from the body. Diuretics have been the main drugs used in antihypertensive therapy for the past 40 years and they are the first-line drugs used in many patients who have mild to moderate hypertension. They are popular because they work quite well, are quite safe, are well tolerated, and are not very expensive. Diuretics may be classed into four related groups: thiazides (for example, chlorothiazide and hydrochlorothiazide), the thiazide-like sulfonamides (for example, metolazone, and indapamide), loop diuretics (for example, furosemide and bumetanide), and the potassium-sparing diuretics (for example, amiloride, triamterene, and spironolactone). The most-effective diuretics are those that work at the loop of Henle.
Thiazides and Sulfonamide Diuretics.
Thiazides and sulfonamide diuretics are the most commonly used class of diuretics and they have similar actions. They work to prevent the reabsorption of sodium and chloride through direct action on the end of the ascending loop and the beginning of the distal tubule of the loop of Henle in the distal kidney tubule (Figure 15-12). They act to block sodium and chloride reabsorption and slightly limit carbonic anhydrase. Their long half-life may lead to the loss of large amounts of potassium.
The thiazides also act directly to dilate the smooth muscles in the arterioles, the smallest vessels in the arterial system. Because the arterioles are made larger, the heart does not have to pump so hard to get blood into them. This helps keep blood pressure lower. Thiazides also work to promote reabsorption of calcium, which may make them good for use in older adults with osteoporosis.
Loop Diuretics.
Loop diuretics act by blocking active transport of chloride, sodium, and potassium in the thick ascending loop of Henle. They are very effective drugs. These drugs often work well in patients with very low glomerular filtration rates, because they are so efficient in limiting the reabsorption of sodium. The peak diuretic effect is much greater for loop diuretics than that seen with any other type of diuretic. They are often used in patients with kidney disease and to treat CHF, cirrhosis of the liver, and kidney diseases in which a powerful diuretic is required.
Potassium-Sparing Diuretics.
Potassium-sparing diuretics increase the excretion of water and sodium, but save potassium. These drugs act by binding at receptor sites in the distal renal tubular cell nucleus, resulting in changes in the creation of proteins that affect the exchange of sodium and potassium. These drugs are used in patients with kidney disease, in older adult patients with poor kidney function who have hypokalemia, or in those patients with the risk for having hypokalemia, often because of treatment with other medications such as digitalis. (Refer to Figure 15-12 for a review of the different parts of the kidney nephron.)
Adrenergic Inhibitors
Adrenergic inhibitors are also divided into five different categories of drugs:
2. Central adrenergic inhibitors
3. Peripheral adrenergic antagonists (most of these drugs are now off the market in the United States)
The sympathetic nervous system relies on two adrenergic neurohormones or neurotransmitters, epinephrine and norepinephrine, to send its messages. These adrenergic inhibitors occupy the adrenergic receptors so that the neurohormones cannot make contact with the receptors, thus preventing stimulation. Adrenergic nerve fibers have either alpha or beta receptors. Thus the blocking can be of alpha, beta, or both alpha and beta receptor sites. If the medication blocks all adrenergic receptor sites, we say it is nonselective in its blocking. Alpha receptor blockers are an important drug group.
Beta Blockers.
Beta blockers are classed into two groups: nonselective and selective beta antagonists. The nonselective agents block both beta1 and beta2 sites. The selective beta1 blocking agents stop the action of the beta1 receptors of the heart, but they have less influence on the beta2 receptors of the bronchi in the lung. There are no selective beta2 inhibitors.
Nonselective beta blockers: (1) reduce the heart rate and the force of contraction, (2) prevent renin release, and (3) slow the outflow of sympathetic nervous system messages from the brainstem to the vasomotor center telling the body to narrow the blood vessels and increase the heart rate. Because these drugs block both beta1 and beta2 impulses, they have a wide range of side effects.
Central Adrenergic Inhibitors.
Central adrenergic inhibitors stimulate peripheral alpha-adrenergic receptors. They cause brief vasoconstriction and then stimulate the presynaptic alpha2-adrenergic receptors in the centers in the brainstem that coordinate cardiovascular function. As a result of this, the total number of sympathetic nervous system messages from the brain is decreased, leading to vascular relaxation and lower blood pressure.
Peripheral Adrenergic Antagonists.
Peripheral adrenergic antagonists work as adrenergic neuron blocking agents that prevent sympathetic nervous system vasoconstriction by limiting norepinephrine release from storage sites in the neurons and by using up all the norepinephrine at nerve endings. When vascular smooth muscle is relaxed, total peripheral resistance to blood flow is decreased. Because of the many side effects of these drugs, most have been removed from the market in the United States.
Alpha1-Adrenergic Inhibitors.
Alpha1-adrenergic inhibitors work through selective blocking of postsynaptic alpha-adrenergic receptor sites, leading to a lowering of peripheral vascular resistance and blood pressure. Both arterioles and venules are dilated by this relaxation of the arteriolar and venous smooth muscles.
Labetalol hydrochloride has a combination of alpha- and beta-adrenergic blocker action. It works as selective alpha1-adrenergic blocker, but is also a nonselective beta-adrenergic blocker.
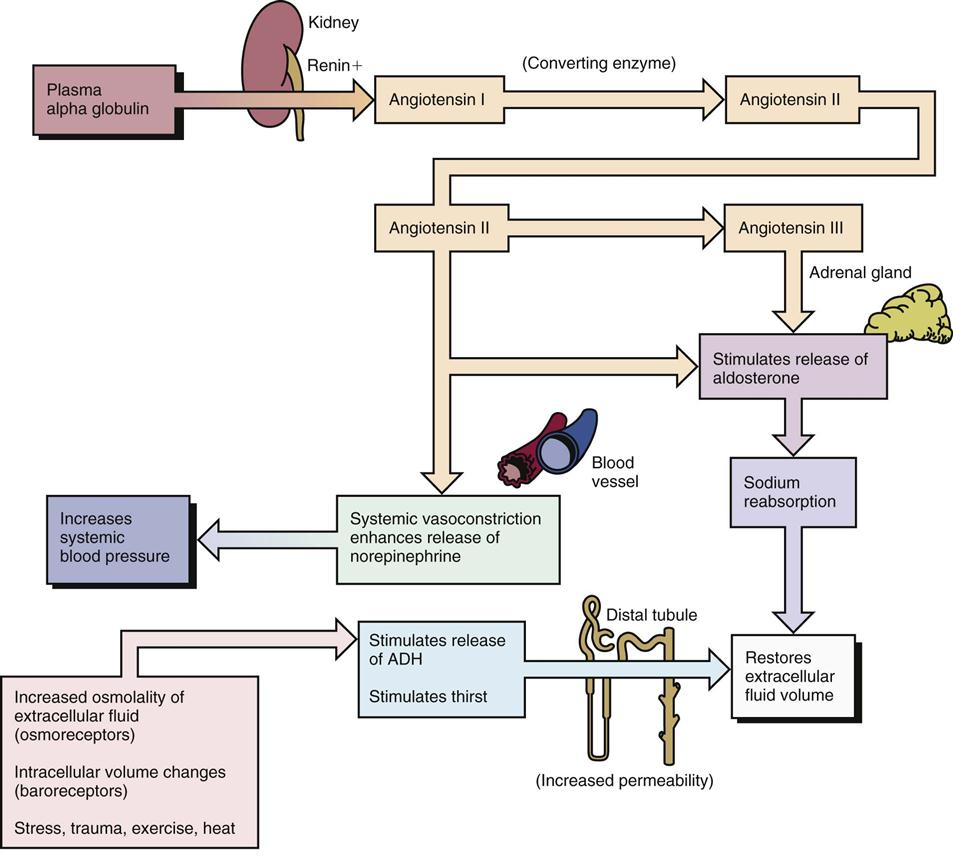
Renin-Angiotensin—Converting Enzyme Inhibitors and Angiotensin II Receptor Antagonists
When the juxtaglomerular apparatus of the kidneys is stimulated, renin is released into the bloodstream to produce angiotensin I. Angiotensin I is then changed to angiotensin II in the liver and the lungs by ACE. Angiotensin II is a powerful vasoconstrictor that acts on the adrenal cortex to increase aldosterone secretion. If a patient is in shock, this renin-angiotensin reaction is important in saving sodium and water to keep the blood pressure up, but at other times, it may help lead to the high blood pressure found in hypertension. Figure 15-13 shows a review of the renin-angiotensin system. It is also known that angiotensin-converting enzymes also form chemicals called angiotensin III and IV that also have weak inhibitor function and play a minor role in this process.
Although we do not know everything about the action of ACE inhibitors, they are thought to stop the change of angiotensin I to angiotensin II by preventing the action of ACE in the plasma and vascular endothelium. There may be other complex actions of these drugs that also help reduce blood pressure. ACE inhibitors are not to be given to pregnant women in the second and third trimesters.
Angiotensin II receptor antagonists block the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the angiotensin receptor found in many tissues. ACE inhibitors often produce a cough in patients. Angiotensin II antagonists do not produce cough.
Vasodilators
Vasodilators reduce systolic and diastolic blood pressure by direct relaxation of arteriolar smooth muscle, thus lowering peripheral vascular resistance. The exact way these drugs work is not known, but they appear to block calcium from moving through the cell membrane.
Calcium Channel Blocking Agents
Calcium channel blocking agents selectively limit the passage of extracellular calcium ions through specific ion channels of the cell membrane in cardiac, vascular, and smooth muscle cells. This causes a lowered peripheral vascular resistance and a fall in systolic and diastolic blood pressure. These drugs are now commonly used to decrease blood pressure.
Uses
Antihypertensives and diuretics (Table 15-9) are used alone or in combination to decrease elevated systolic and diastolic blood pressure. Blood pressure may be defined as pressure of the blood against the walls of the various vessels. The blood pressure is highest at the moment the ventricles contract (systole), because the heart has to push very hard to get the blood out into the circulation. This is called systolic pressure. Pressure during ventricular relaxation is known as diastolic pressure and is the pressure at the lowest part of the cardiac cycle. These pressures are written as a fraction, with the systolic as the numerator (the number on top of the fraction) and the diastolic as the denominator (the number on the bottom of the fraction). Respected clinical studies suggest that it is beneficial to use a combination of diet, drug therapy, and reduction of risk factors to treat hypertension. The therapeutic goal in the hypertensive patient is to reduce the blood pressure to normal or near normal with few adverse effects. Reduction of both systolic and diastolic pressure has been associated with decreased risk of damage to the vascular tissues of the heart, kidneys, brain, eyes, and other organs, or end-organ damage.
![]() Table 15-9
Table 15-9
| MEDICATION CATEGORY AND GENERIC NAME | TRADE NAME |
| Diuretics | |
| Thiazide and Related Sulfonamide Diuretics | |
| chlorothiazide | Diuril |
| hydrochlorothiazide | HydroDIRUIL, Microzide |
| chlorthalidone | Hygroton |
| indapamide | Lozol |
| metolazone, | Zaroxolyn Mykrox |
| Loop Diuretics | |
| bumetanide | Bumex |
| furosemide | Lasix |
| torsemide | Demadex |
| Potassium-Sparing Agents | |
| amiloride | Midamor |
| spironolactone | Aldactone |
| triamterene | Dyrenium |
| Adrenergic Inhibitors | |
| Central Adrenergic Inhibitors | |
| clonidine | Catapres, Duraclon |
| guanabenz | Wytensin |
| methyldopa | Aldomet |
| Alpha1-Adrenergic Blockers | |
| doxazosin | Cardura |
| prazosin | Minipress |
| terazosin | Hytrin |
| Beta-Adrenergic Blockers | |
| atenolol | Tenormin |
| betaxolol | Kerlone |
| bisoprolol | Zebeta |
| metoprolol | Lopressor, Toprol XL |
| nadolol | Corgard |
| propranolol) | Inderal |
| Combined Alpha- and Beta-Adrenergic Blocker | |
| carvedilol | Coreg |
| labetalol | Normodyne, Trandate |
| Vasodilators | |
| hydralazine | Apresoline |
| minoxidil | Loniten |
| Ace Inhibitors | |
| benazepril | Lotensin |
| captopril | Capoten |
| enalapril | Vasotec |
| fosinopril | Monopril |
| lisinopril | Zestril |
| moexipril | Univasc |
| perindopril | Aceon |
| quinapril | Accupril |
| ramipril | Altace |
| trandolapril | Mavik |
| Angiotensin II Receptor Antagonists or Blockers | |
| candesartan | Atacand |
| irbesartan | Avapro |
| losartan | Cozaar |
| valsartan | Diovan |
| Calcium Channel Blocking Agents | |
| amlodipine | Norvasc |
| diltiazem | Cardizem |
| eprosartan | Teveten |
| felodipine | Plendil |
| isradipine | DynaCirc |
| nicardipine | Cardene |
| nifedipine | Procardia |
| nisoldipine | Nisocor, Sular |
| olmesartan | Benicar |
| telmisartan | Micardis |
| verapamil | Calan |
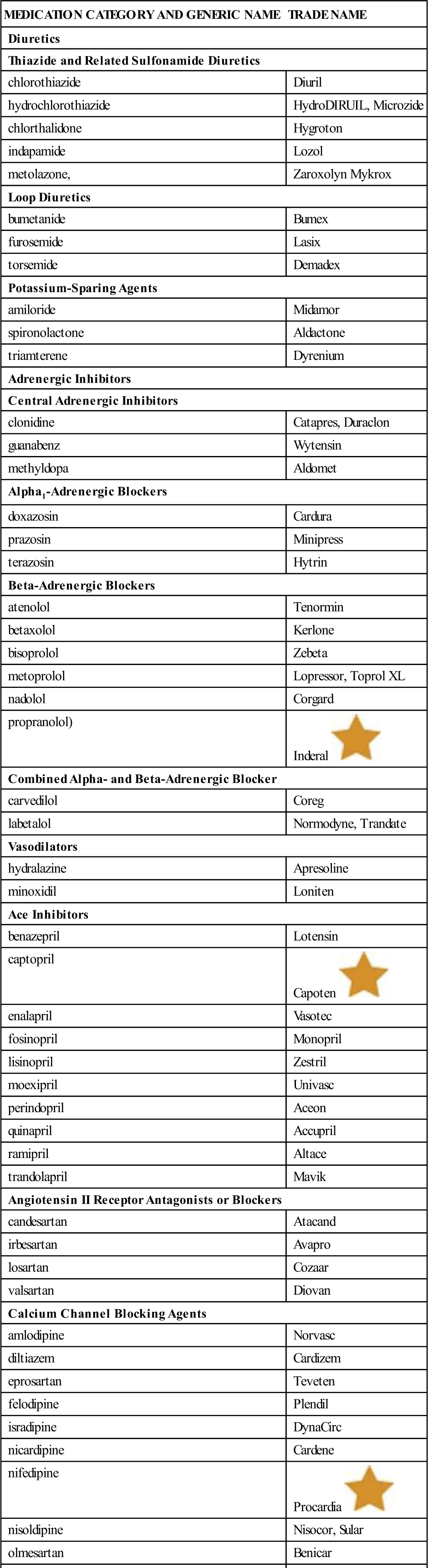
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
The patient with hypertension may have no symptoms or may complain of not feeling well in general. Headaches, frequently associated with hypertension, are often produced by stress, tension, or other reasons, rather than being related to high blood pressure, unless very severe blood pressure elevations are present. In cases of secondary hypertension, there may be reports of getting up at night to go to the bathroom (nocturia), history of renal trauma (producing renal artery stenosis), or a family history of hypertension.
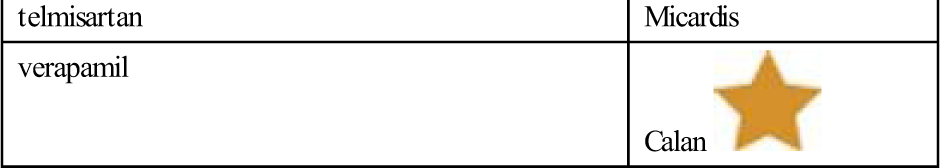
Hypertension is classified according to the stages listed in Table 15-10. The choice of antihypertensive drug depends on many factors: how severe the hypertension is, the presence of compelling indications (other diseases for which a specific class of antihypertensives has been shown to improve the patient’s condition), the use of other drugs, and the patient’s willingness to accept the mild but unavoidable side effects that may develop.
Table 15-10
Classification and Management of Blood Pressure for Adults
| INITIAL DRUG THERAPY | ||||
| BP CLASS | SYSTOLIC BP (mm HG) | DIASTOLIC BP (mm HG) | WITHOUT COMPELLING INDICATION | WITH COMPELLING INDICATION |
| Normal | <120 | and <80 | None indicated | Drugs for compelling indications |
| Prehypertension | 120-139 | or 80-89 | ||
| Stage 1 HTN | 140-159 | or 90-99 | Thiazide-type diuretics for most; ACEI, ARB, BB, CCB, or combination may be considered | Drug(s) for compelling indications |
| Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) | ||||
| Stage 2 HTN | >160 | or >100 | Two-drug combination for months (usually thiazide-type diuretic and ACEI or ARB or BB or CCB) | As needed |
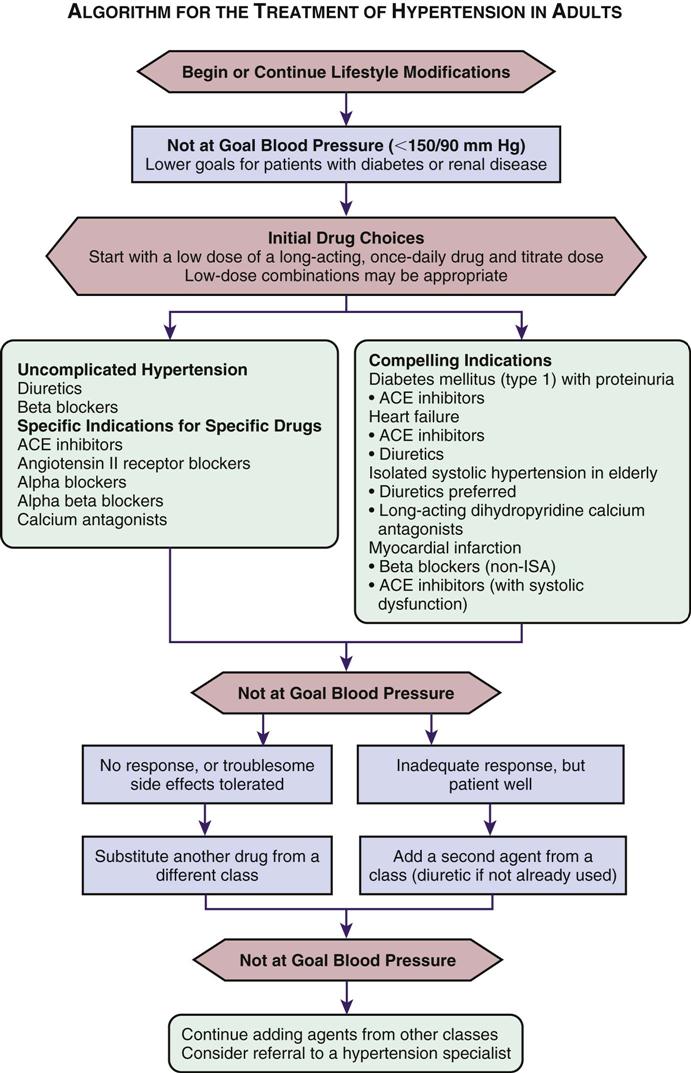
The Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure has indicated how the antihypertensive drugs should be used for initial therapy and when and what additional drugs are to be used (Table 15-11). The treatment plan starts with lifestyle modifications, then a single mild agent, gradually increasing the dosage, and then adding drugs from other drug categories to bring the diastolic blood pressure under control. The drug effects are balanced in this approach to take advantage of different kinds of drug action. (See treatment algorhythm, Figure 15-14).
Table 15-11
Management of Hypertension Based on Risk Stratification
| BLOOD PRESSURE STAGES (MM HG) | RISK GROUP A (NO RISK FACTORS AND NO TOD/CCD) | RISK GROUP B (AT LEAST ONE RISK FACTOR, NOT INCLUDING DM; NO TOD/CCD) | RISK GROUP C (TOD/CCD AND/OR DM, WITH OR WITHOUT OTHER RISK FACTORS) |
| High-normal (130-139/85-89) | Lifestyle modification* | Lifestyle modification | Drug therapy† |
| Stage 1 (140-159/90-99) | Lifestyle modification (up to 12 mo) | Lifestyle modification (up to 6 mo) | Drug therapy |
| Stages 2 and 3 (>160/>100) | Drug therapy | Drug therapy | Drug therapy |
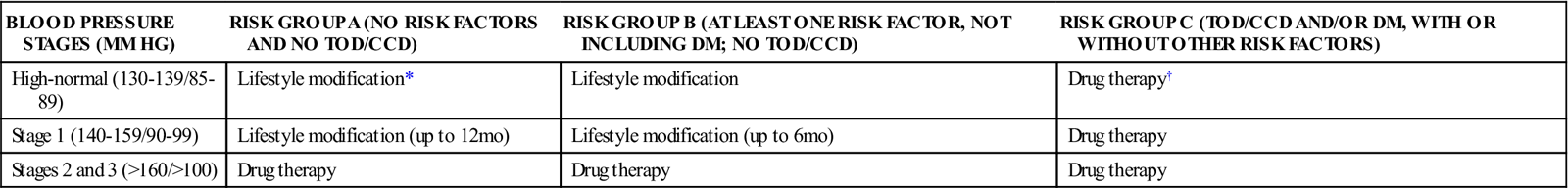
DM, Diabetes mellitus; TOD/CCD, target organ damage/clinical cardiovascular disease.
*Should be adjunctive therapy for all patients recommended for pharmacologic therapy.
†For those patients with heart failure, renal insufficiency, or diabetes.
Stage I: Lifestyle Changes
Before starting drug therapy for patients with hypertension, a lot of effort should be made to help patients reduce their risk factors. Lifestyle changes to help patients lose weight; increase physical activity; and reduce fat, salt, and calories in the diet are helpful in lowering blood pressure. Behavior change to assist them to stop smoking and reduce alcohol intake is also important.
Stage II: Drug Therapy
The drug of choice in starting antihypertensive therapy is an oral thiazide—or thiazide-like sulfonamide drug—or an adrenergic beta blocker. Other drugs are added if needed, based on how the patient responds to the first drug. Most thiazides or beta blockers are effective when given once a day. The drug is started at a low dosage and increased as needed until the maximum dose is reached. In many cases, one of the drugs by itself will reduce the diastolic blood pressure to the desired level. Because these drugs commonly produce hypokalemia, a potassium supplement may also be required. Loop diuretics are used when hypertension is severe and the blood pressure must come down quickly. An antiadrenergic agent may be added to the treatment plan if the maximum doses of diuretics or beta blockers fail to lower the blood pressure to the desired level. These two categories of drugs work well together to bring down blood pressure and lower the chance of side effects, and they are better than using an antiadrenergic agent alone. There are a variety of antiadrenergic drugs, so the patient can try different combinations to find the ones that work best. The patient should move on to the next level of drug treatment only if a drug regimen fails to adequately control blood pressure. It should be noted that beta blockers seem to be less effective in black and much older adult patients. Captopril is another drug that seems to be less effective in black patients.
Other drugs that might be added to the therapeutic plan are vasodilators. Vasodilators are most effective when used with a beta-adrenergic blocking agent to control the rapid heartbeat that often results from lowering peripheral resistance.
There has been a lot of research on antihypertensive drugs in therapy in recent years; new drugs have entered the market and more research findings have been published. Some drugs are particularly helpful in certain conditions. Refer to Table 15-12 for drugs used in other diseases.
![]() Table 15-12
Table 15-12
Antihypertensive Drug Classes used in other Diseases
| COMPELLING INDICATION | DIURETIC | BETA BLOCKER | ANGIOTENSIN-CONVERTING ENZYME INHIBITOR | ALPHA RECEPTOR BLOCKER | CALCIUM CHANNEL BLOCKER | ALDOSTERONE ANTAGONIST |
| Heart failure | X | X | X | X | X | |
| Post MI | X | X | X | |||
| High risk for CAD | X | X | X | X | ||
| Diabetes | X | X | X | X | X | |
| Chronic kidney disease | X | X | ||||
| Recurrent stroke prevention | X | X |
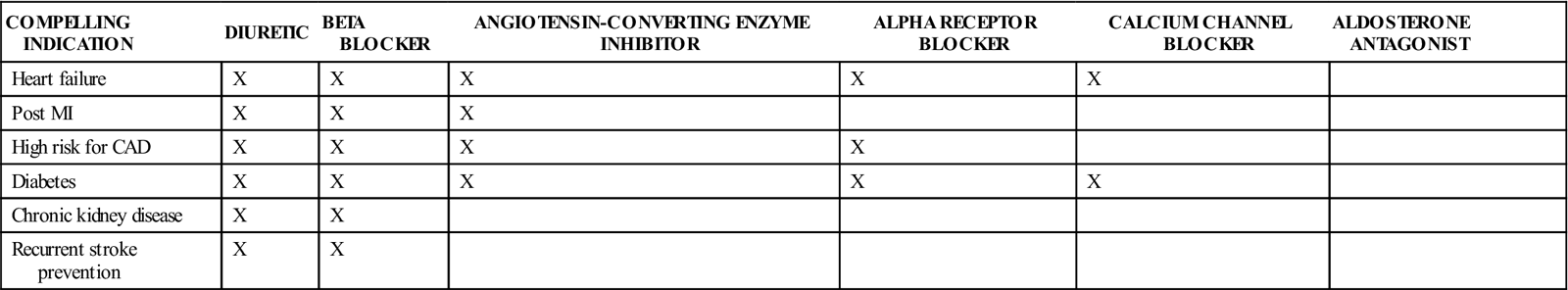
CAD, Coronary artery disease; MI, myocardial infarction.
Modified from National Heart, Lung, and Blood Institutes, National High Blood Pressure Education Program: The Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, Bethesda, MD, 2003, National Institutes of Health.
Adverse Reactions
Each category and each drug has many important adverse reactions. Hypokalemia and drowsiness are commonly seen, and many drugs produce impotence in men. Table 15-13 provides a list of the most common adverse reactions to the antihypertensive and diuretic drugs. For example, prazosin may cause severe syncope after the first dose, so the patient should take the first dose when someone else can be there. Potassium chloride (KCl) tablets may be irritating to the mouth and stomach if not taken with food. Antacids may help reduce this irritation.
![]() Table 15-13
Table 15-13
Adverse Drug Effects of Antihypertensive and Diuretic Drugs
| MEDICATION | SIDE EFFECTS | PRECAUTIONS |
| Diuretics | ||
| Alpha-adrenergic blockers | “First-dose” syncope with prazosin; postural hypotension, weakness, palpitations, dizziness | Use cautiously in older adult patients because of hypotension. |
| Beta-adrenergic blockers | Bradycardia, insomnia, fatigue, sexual dysfunction, bizarre dreams, decreased HDL cholesterol | Not for use in patients with asthma, COPD, CHF, heart block, and sick sinus syndrome. Used with caution in patients with diabetes and peripheral vascular disease. |
| Central-acting adrenergic blockers | Drowsiness, fatigue, sexual dysfunction, dry mouth | Clonidine and guanabenz may produce rebound hypertension if abruptly stopped. Methyldopa may cause liver damage and a positive direct Coombs test. |
| Combined alpha- and beta-adrenergic blockers | Nausea, fatigue, dizziness, asthma, headache | Not for use in sick sinus syndrome or heart block; used with caution in CHF, bronchial asthma, COPD, and diabetes mellitus. |
| Loop diuretics | Same as for thiazides | Effective in chronic renal failure; caution with hypokalemia and hyperuricemia; may cause hyponatremia, especially in older adults. |
| Peripheral-acting adrenergic inhibitors | Sexual dysfunction, nasal congestion, postural hypotension, diarrhea, lethargy | Used very cautiously in older adult patients because of hypotension. Rauwolfia and reserpine are not to be given to patients with a history of mental depression. |
| Potassium-sparing agents | Hyperkalemia, sexual dysfunction, gynecomastia, mastodynia | Monitor fluid and electrolytes. |
| Thiazides and thiazide-related sulfonamides | Hypokalemia, hyperuricemia, glucose intolerance, hypercholesterolemia, sexual dysfunction | May be ineffective in renal failure; hypokalemia increases digitalis toxicity; hyperuricemia may precipitate acute gout. |
| Vasodilators | ||
| Vasodilators | Headache, tachycardia, fluid retention | May produce angina in patients with coronary artery disease. |
| Hydralazine may produce positive ANA | Lupuslike syndrome may occur with higher doses of hydralazine. | |
| Minoxidil may produce abnormal growth of hair, ascites (intraperitoneal pooling of large amount of fluid) | May cause or aggravate pleural and pericardial effusions. | |
| Angiotensin-Converting Enzyme Inhibitors | ||
| ACE inhibitors | Hyperkalemia, nonproductive cough (frequent) | Can cause neutropenia with autoimmune-collagen disorders. May cause proteinuria or reversible acute renal failure in patients with bilateral renal artery stenosis. |
| Calcium Channel Blocking Agents | ||
| Calcium channel blockers | Headache, hypotension, nausea, dizziness, flushing, edema, constipation | Used with caution in patients with CHF or heart block; do not administer immediately after MI. |
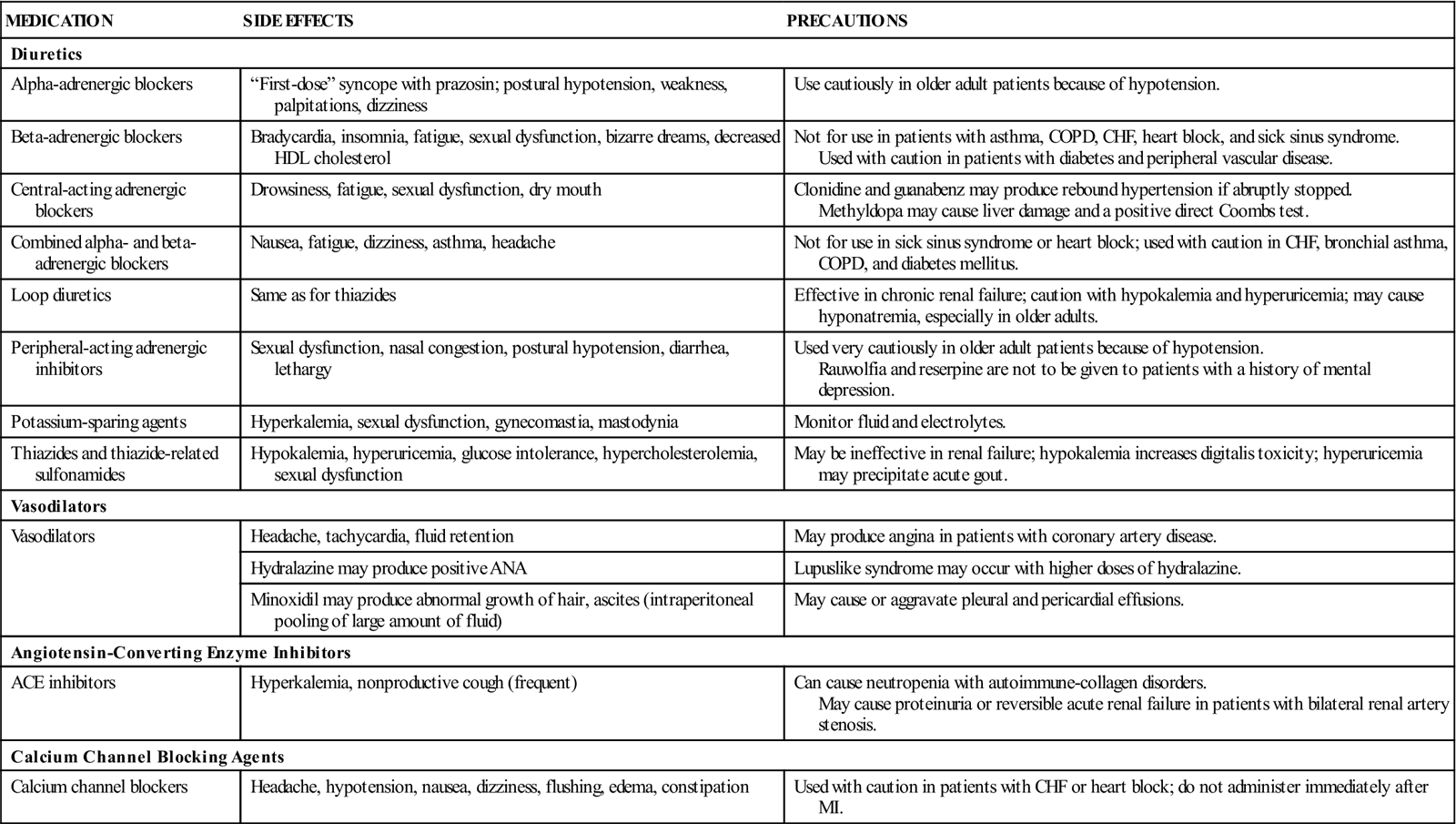
Drug Interactions
Frequently a patient with high blood pressure has to take many different medicines because other medical problems exist. All of the antihypertensive drugs may have drug interactions. The nurse checks each drug the patient is taking; interactive effects that lower the blood pressure too much or make the blood pressure go even higher can occur.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient. Although the cause for most high blood pressure is unknown, the health care provider will look for any disease that might also cause hypertension, such as Cushing disease, Addison disease, renal artery stenosis, coarctation of the aorta, or pheochromocytoma. The nurse will want to ask about whether the patient has other diseases, allergies, or medications that may affect antihypertensives and diuretics.
The number of drug side effects and problems that occur when hypertension is not treated effectively is high, and good record keeping is important in learning if the patient is getting well.
n Diagnosis
Does the patient understand that high blood pressure medication may need to be taken for the rest of his or her life? Does the patient understand that to reduce high blood pressure, lifestyle changes may be as important as medication? What factors does the patient have that will make therapy difficult?
n Planning
Because there is no cure for high blood pressure, a lot of patient teaching and education is needed to help the patient understand what is happening and cooperate with successful treatment. Although taking the medication is important, it is also important to work on other things in the patient’s life, such as removing risk factors and changing the diet.
n Implementation
Many patients with hypertension do not feel sick, so they have a hard time being compliant with the treatment regimen. High blood pressure is a “silent disease” because it has no symptoms. Because patients may only have symptoms as a result of side effects from their medication, they may not want to take drugs. It is important to teach patients about what is really happening to them to help them understand their disease.
The high cost of antihypertensive drugs and the desire of patients to have control over their therapy lead many of them to explore the use of herbal medications to lower blood pressure. The Complementary and Alternative Therapies box describes some of the more common herbal products patients may use. Little standardized research has been done to discover whether herbal products are safe or effective.
Patients taking diuretics should avoid caffeinated beverages as the diuretic effect of caffeine plus their medications may cause them to become dehydrated.
Encourage patients to lose weight, lower sodium intake, avoid stress and emotional pressures, develop regular and reasonable exercise routines, and have hobbies or activities that make them feel good about themselves (improve self-esteem). Remind them that taking their medications is only a small part of the total treatment plan.
When taking loop or thiazide diuretics, the patient should eat or drink more potassium-rich foods such as citrus fruits; bananas; potatoes; dark, leafy vegetables; and nuts. If the patient is taking a potassium-sparing diuretics, he or she should avoid excessive quantities of these foods.
n Evaluation
In addition to taking the patient’s blood pressure, a good eye examination can tell if the patient’s hypertension is well controlled. The blood vessels of the eye can be seen by looking through the pupil into the eye with an ophthalmoscope. By examining the fundus of the eye, it is possible to tell whether the blood pressure has been high, even if it is low when the patient is seen. Many parts of the body are damaged by high blood pressure: the heart, the lungs, the eyes, and the kidneys. Ask if the patient has any complaints that might suggest problems in any of these areas (end-organ damage). Ask about side effects the antihypertensive medication might be producing. Men should always be asked about their sexual functioning, because impotence is often caused by these medications, and they may not share this information unless asked. They may not even realize sexual problems may be related to their medication.
n Patient and Family Teaching
Tell the patient and family the following:
Other Nondiuretic Drugs Useful in Treating Urinary Problems
Overview
There are many problems that might produce urinary tract symptoms. Drugs used for these problems usually involve giving relief for symptoms. These include drugs used to treat urinary incontinence (wetting) and benign prostatic hyperplasia (BPH) and drugs for urinary tract analgesia (pain relief) and urinary tract infections.
Action and Uses
Drugs for Urinary Incontinence
Urinary incontinence is when patients wet themselves or leak urine, and this problem may have many causes. Medications used in treating this problem include some anticholinergics and antispasmodics, alpha-adrenergic agonists, estrogens, cholinergic agonists, and alpha-adrenergic antagonists. The anticholinergic agents stop contraction of the bladder and decrease the response of some of the bladder muscles. Antispasmodic drugs have a direct action on smooth muscle relaxation. Estrogen used either orally or vaginally may help restore urethral mucosa and increase vascularity, tone, and the ability of the urethral muscle to respond.
Benign Prostatic Hyperplasia
BPH is a noncancerous growth of the prostate gland frequently seen as men age; if this gland becomes large enough, it can cause voiding problems because the prostate puts pressure on the bladder and urinary sphincter. Drugs used in the management of BPH are the alpha1-adrenergic receptor blockers (these have already been discussed for the treatment of hypertension). Tamsulosin (Flomax) is an alpha-adrenergic receptor blocker used only for the treatment of symptoms of BPH. Finasteride is also used for treatment of BPH. Use of these products either reduces the urgency to urinate or shrinks the prostate so that urine can pass more easily.
Short-Term Analgesia
Phenazopyridine is a drug used to control pain in the urinary tract, usually from acute urinary tract infection. The agent may also be ordered following procedures on the urinary tract such as a cystoscopy or biopsy. This product is effective for only a couple of hours and so will require repeated administration.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn the history of the urinary problem to make certain the patient’s symptoms are recorded correctly. The patient may be nervous about discussing these problems.
n Diagnosis
Find out the reason why the medication is being given. Are the symptoms because of another problem, or do they represent the major problem? (Is there other gynecologic or genitourinary disease present?) Read any medical records kept by the patient about urinary incontinence or voiding problems. This may be helpful in learning the cause of the symptoms.
n Planning
Teach the patient about what has caused the problem and how the medication will help.
n Implementation
Sometimes the patient is asked to keep a bladder diary. If so, explain clearly how to keep the records about wetting accidents and why. Give the patient a lot of support so they will be compliant.
Drug action and uses, adverse effects, drug interactions, and important patient teaching points are given in Table 15-14.
![]() Table 15-14
Table 15-14
Miscellaneous Nondiuretic Drugs Used to Treat Urinary Problems
| MEDICATION | ACTION AND USES | ADVERSE EFFECTS | DRUG INTERACTIONS | NURSING IMPLICATIONS AND PATIENT TEACHING |
| Drugs for Urinary Incontinence | ||||
| Anticholinergics/Antispasmodics | ||||
| flavoxate (Urispas) | Antispasmodic action for dysuria, nocturia, urgency, suprapubic pain, frequency, incontinence caused by detrusor instability, and hyperreflexia | Headache, confusion, nervousness, nausea, vomiting | Enhances anticholinergic effects of other anticholinergic drugs | Discuss anticholinergic effects with older patients, as they may pose a problem. |
| oxybutynin chloride (Ditropan) | Used to relieve symptoms associated with detrusor instability, hyperreflexia, or involuntary bladder contractions | Drowsiness, dry mouth, blurred vision, constipation; may aggravate symptoms of heart disease, hyperthyroidism, GI problems | May increase digoxin serum concentrations; may decrease action of haloperidol and enhance development of tardive dyskinesia (repeated involuntary muscle movements); avoid alcohol | Requires careful patient teaching concerning response and side effects; monitor clinical effectiveness through use of a bladder diary documenting voiding activity. |
| propantheline (Pro-Banthine) | Treats involuntary ureteral and bladder contractions by competitively blocking action of acetylcholine at postganglionic parasympathetic receptor sites | Dry mouth, constipation, urinary retention | Increases effect of narcotic analgesics, class I antidysrhythmics, antihistamines, phenothiazines, TCAs, corticosteroids, CNS depressants, beta blockers, amoxapine | Side effects more often seen and may cause problems in older patients. |
| tolterodine (Detrol) | For urinary frequency, urgency, and urge incontinence caused by bladder overactivity | Less dry mouth than with oxybutynin; dyspepsia, headache, constipation, dry eyes | None noted | Tolterodine should be avoided by patients with glaucoma, ulcerative colitis, megacolon, GI or urinary obstruction; should be used with care by individuals with BPH. |
| Cholinergic Agonist | ||||
| bethanechol chloride | Used in nonobstructive urinary retention | Hypotension, dizziness, flushing, sweating | With other cholinergics, additive cholinergic effects and toxicity may occur | Dosage highly individualized. |
| Drugs for Benign Prostatic Hyperplasia | ||||
| Alpha-Adrenergic Antagonists | ||||
| finasteride (Proscar) | Treats symptoms of BPH | Impotence, decreased libido, decreased volume of ejaculate, breast tenderness and enlargement, hypersensitivity reactions, including lip swelling and skin rash | None noted | May be taken with or without food; 6-12 mo of therapy may be required to assess response. |
| tamsulosin (Flomax) | Treats symptoms of BPH by selective inhibition of alpha1A receptors | Postural hypotension, dizziness, somnolence, rhinitis, diarrhea, abnormal ejaculation | Potentiates other alpha-adrenergic blocking agents | Take at the same time every day, approximately  hr after eating; may take 2-4 wk before response is seen. hr after eating; may take 2-4 wk before response is seen. |
| terazosin | Treats hypertension and provides superior action in treating BPH | Angina, blurred vision, constipation, diarrhea, orthostatic hypotension, syncope May have first-dose response of acute postural hypotension. |
May reduce antihypertensive effects if given with NSAIDs. Antihypertensive effects of other drugs may result in acute postural hypotension. | Monitor for exaggerated hypotensive effects, particularly in geriatric patients or those with renal impairment. |
| Drug for Urinary Tract Analgesia | ||||
| Phenazopyridine (Pyridium) | Symptomatic relief of pain, burning, urgency, frequency associated with UTI | Headaches, rash, vertigo, GI disturbance, anaphylactic (shock)-like reactions | None noted | Stains the urine orange or red and may stain fabrics; notify doctor if jaundice (yellow color of skin or eyes) develops; available OTC. |
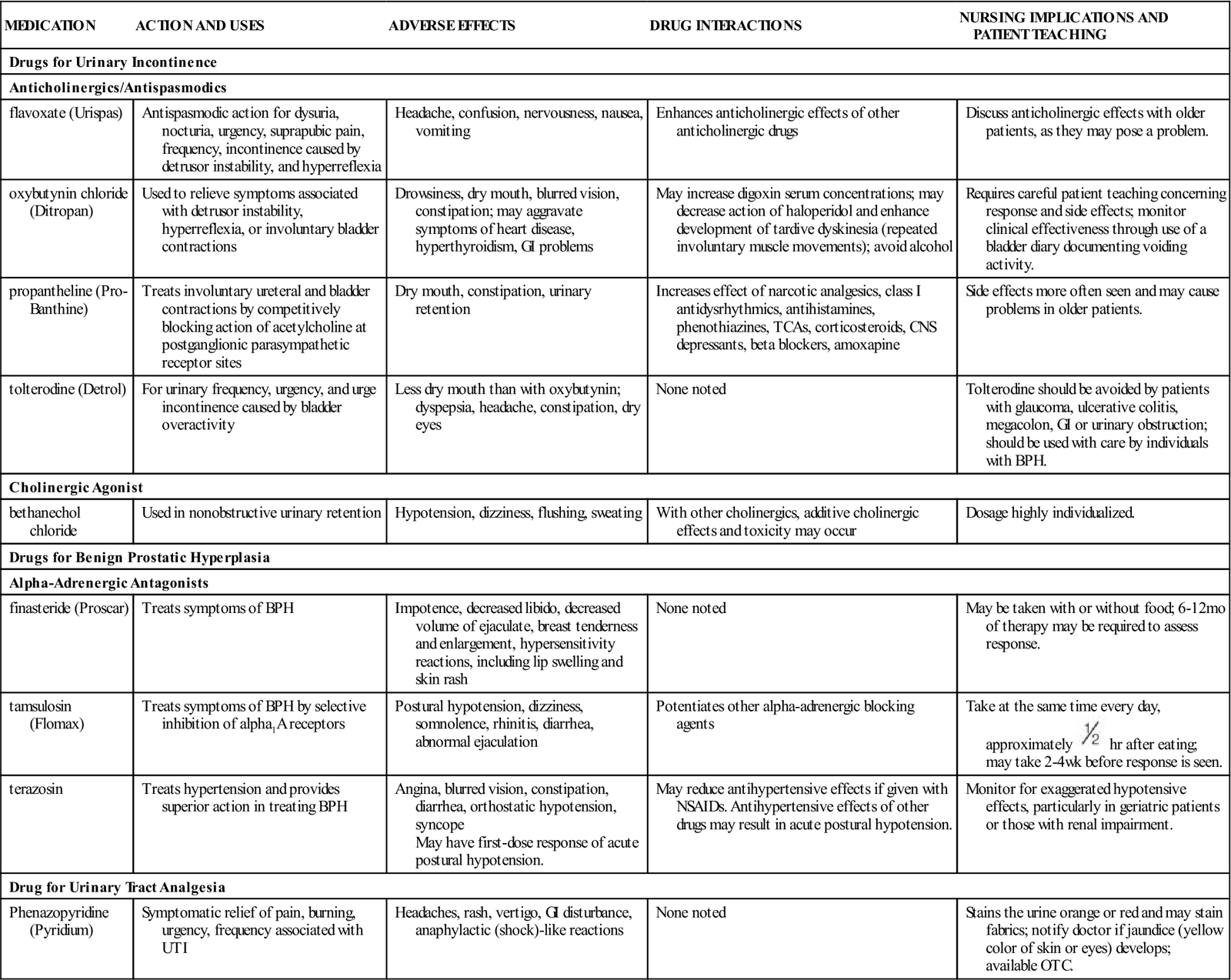
n Evaluation
All of these medications should reduce symptoms. Explain to patients how they will know when the medication is working. For medications related to BPH, explain that treatment may be required for weeks or months before symptoms go away.
n Patient and Family Teaching
Fluid and Electrolytes
Overview
Strong pumping of the heart, good circulation through the vessels, and the full removal of by-products through the urinary system are all needed to keep the body’s fluid and electrolyte balance. Lack of body fluid may be due to inadequate intake, excess loss, or both. This imbalance may be treated by administration of fluids and electrolyte mixtures. The kidneys play the major role in how much fluid is present in the body and the number and types of electrolytes, acids, and bases. The kidneys work to make adjustments in fluid and electrolytes all the time. If the kidneys do not work properly, major changes may occur in fluids and electrolytes that may affect the body’s ability to work.
Action and Uses
Patients taking diuretics should avoid caffeinated beverages as the diuretic effect of caffeine plus their medications may cause them to become dehydrated. There are two types of IV replacement fluids: (1) Crystalloid mixtures made of fluid and electrolyte mixtures that may be composed of water and calories in the form of carbohydrates, or with minerals and electrolytes such as sodium, potassium, chloride, calcium, and phosphorus. These solutions travel in the blood and then enter cells and tissue. As they replace missing fluid or electrolytes they help the kidneys so urine is produced. (2) Colloids such as plasma or volume expanders. These products contain large molecules or proteins that remain suspended in the blood and do not cross cell membranes but act to draw water molecules from the cells and tissues into the blood vessels as they increase osmotic pressure.
Many fluid and electrolyte solutions are given when oral food intake has been stopped or to prevent dehydration (loss of a large amount of water from the body tissues, along with loss of electrolytes), especially in patients with diarrhea. Causes of dehydration include vomiting, bowel obstruction (which causes a pooling of fluid and electrolytes), diarrhea, and fever (which increases the use of fluid and electrolytes). The body attempts to adjust to the reduced circulating volume by pulling in first extracellular fluid and then intracellular fluid. This causes an imbalance of both fluid and electrolytes that must be corrected.
Fluid and electrolytes may be given either orally or parenterally to prevent dehydration when oral intake is briefly halted and to replace moderate losses of fluids and electrolytes (Table 15-15 and Box 15-1).
Table 15-15
Fluid and Electrolytes for Oral Administration
| PRODUCT | COMMENTS AND DOSAGE |
| Oral Electrolyte Solutions | |
| Pedialyte | Dosage should be based on water requirements calculated on the basis of total body surface area for infants and young children. A general guide uses 1500 mL/m2 for maintenance during illness and 2400 mL/m2 for maintenance and replacement of mild to moderate fluid losses (as in diarrhea or vomiting). Replacement in mild to moderate fluid losses: Children 5-10 years of age: 1-2 quarts/day Older children and adults: 2-3 quarts/day |
| Salt Substitutes | |
| Adolph’s salt substitute Morton salt substitute Neocurtasal NoSalt Nu-Salt |
OTC preparations that can be used in both cooked and uncooked foods to make food more palatable for patients with sodium restrictions. These potassium chloride preparations come in a salt shaker dispenser and are used in amounts slightly less than normal amounts of NaCl. NOTE: Contraindicated in patients with severe kidney disease or oliguria. Long-term use may require iodine supplements in some patients. |
| sodium bicarbonate | Used as gastric, systemic, and urinary alkalinizer. May relieve symptoms of occasional overeating and indigestion. Usual adult dose 325 mg to 2 g 2-4 times daily. Daily maximum intake should not exceed 16 g. |
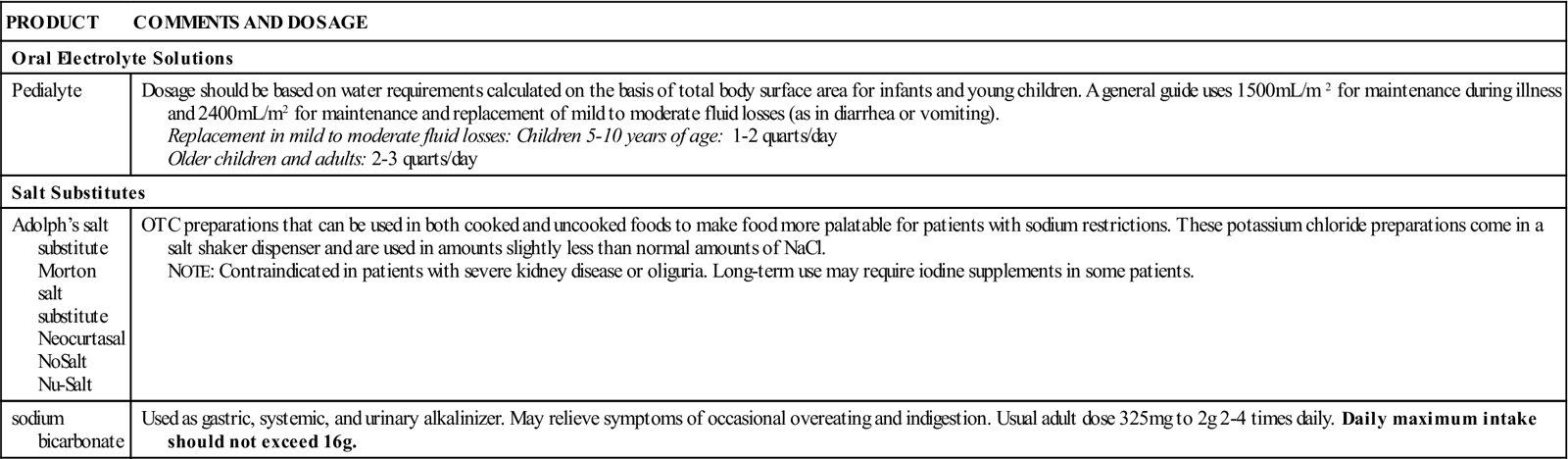
The healthy body is able to make constant changes in kidney function, breathing, and heart rate, to keep it healthy. When the body is seriously ill, these balancing tasks do not occur well. Not only does the body need fluid, but a careful balance between acid and base must be maintained when patients are very ill. The amount of acid and base or alkalinity in the body is measured by its pH. Blood or body fluids that measure above 7.0 are called basic or alkaline. Those that measure below 7.0 are called acidic. The normal body pH is 7.35 to 7.45—a very narrow range. Movement either higher or lower than this pH range poses a threat to life. If the body pH is abnormally high or low, the cause must be identified and treated as soon as possible through use of IV fluids. If it is not restored to the normal range, the body will go into acidosis with severe CNS depression or coma, or into CNS stimulation and convulsions with alkalosis. Neither extreme will allow the patient to live. If the patient is acidotic, sodium bicarbonate may be added to the fluid to help the patient achieve homeostasis, or the right balance. If the patient is alkalotic, ammonium chloride or sodium chloride with KCl may be added to fluids. So electrolytes are very important in keeping this balance.
Electrolytes are small, inorganic molecules with either a positive or negative charge. Positive charged molecules are called cations; negatively charged molecules are called anions. Laboratory testing will help determine what electrolytes need to be given and how much. Electrolyte solutions are especially useful in managing dehydration in infants caused by diarrhea.
Potassium is the major cation inside the cell. The normal range of potassium in the body is very small and even minor excess (hyperkalemia) or loss (hypokalemia) may cause serious problems. KCl solutions are given to correct hypokalemia. Sodium is the major electrolyte in the extracellular fluid. If there is an excess of sodium (hypernatremia) in the blood because it is not removed by the kidneys, IV fluids such as 5% dextrose with water may be given. Some diuretics also help remove sodium through the kidneys. If there is a lack of sodium (hyponatremia), it may be treated with solutions that include sodium chloride.
See Box 15-1 for a listing of the most common colloid and crystalloid products.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Patients who are dehydrated need fluids. Water alone is often not adequate. Signs of dehydration include weight loss, dry skin, lack of sweat, dry mucous membranes, decreased urinary output, hypotension, tachycardia, and increased respirations. In infants, dehydration may also include sunken fontanelles and loss of skin turgor (strength and mass). Fluid and electrolytes are also required in the comatose or acutely ill patient who is unable to take oral substances for a long time.
Oral fluids are contraindicated when the patient has severe or continuing diarrhea or other major fluid loss that requires IV replacement or has vomiting that cannot be stopped. They should not be used in patients with intestinal obstruction or bowel perforation (opening), decreased renal function, or when the homeostatic mechanism of the body is damaged. IV fluids with replacement electrolytes are required.
The prescribed amount of fluid and electrolytes should be ordered by the health care provider and should not be exceeded. If the patient is still thirsty after taking the recommended dose, extra fluids in the form of water or other fluids that do not contain electrolytes might be ordered.