CASE 149
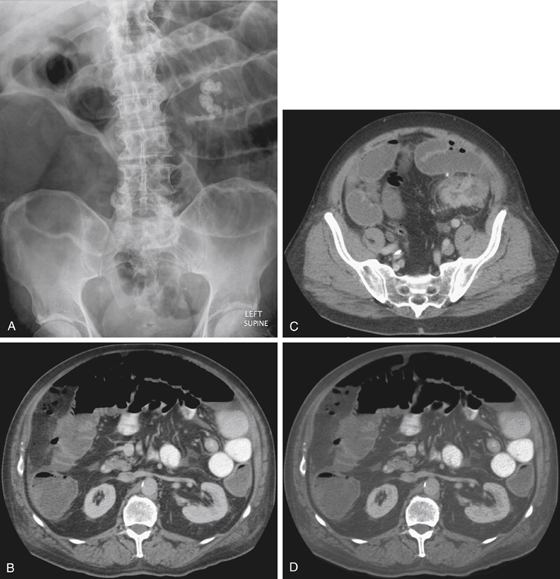
History: A 68-year-old man with 5 months of constipation now presents with 3 days of acute lower abdominal pain and distention.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. Which of the following complications of colon cancer is most frequently observed?
3. Sigmoid diverticulitis and carcinoma can appear similar on CT scan. Which feature favors a diagnosis of carcinoma?
A. Engorgement of pericolonic vessels
B. Fluid in the mesenteric root
4. To differentiate colonic perforation that is caused by cancer from perforation caused by various benign conditions, which of the following features is most suggestive of malignancy?
A. Irregular thickening of the colonic wall
B. Focal defect in the colon wall
ANSWERS
CASE 149
Left-Sided Colonic Cancer Obstruction with Perforation
1. B and C
2. C
3. C
4. A
References
Horton KM, Abrams RA, Fishman EK. Spiral CT of colon cancer: imaging features and role in management. Radiographics. 2000;20(2):419–430.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 302.
Comment
The general thinking regarding the clinical differences in right versus left colonic carcinomas relates to the following factors:
• The wider right-sided lumen and relatively thinner wall of the left colon
• The fact that one of the main physiologic functions of the colon is water reabsorption
Most right-sided lesions can grow quite large and still not be obstructive. Most left-sided lesions manifest with rectal bleeding. The lumen of the left side is smaller and water absorption has resulted in stool formation, and as a result a left-sided lesion often manifests as an obstructive process such as seen on the CT images in this case (see figures).
However, a slowly growing indolent lesion of the left colon may manifest as an exception to the rule. Because of slow growth, the luminal contours of the lesions are affected by the fecal stream and develop a “flap valve” configuration. As a result, such patients may be shown to have complete retrograde obstruction to the flow of barium, with no evidence of antegrade obstruction (i.e., dilated fluid-filled loops of bowel, air-fluid levels). This situation addresses the age-old issue of “should I stop the barium flow when I encounter an incomplete colonic obstruction?” The answer is clear. If there is evidence of antegrade obstruction, one should cease the barium flow immediately. Putting barium on the proximal side of an obstructing lesion can complicate the situation. However, if there is no evidence of antegrade obstruction on plain images of the abdomen, one can continue to examine the proximal colon without fear of causing harm.







