CHAPTER 148
Pressure Ulcers
Chester H. Ho, MD; Kath Bogie, DPhil
Definition
A pressure ulcer is a localized injury to the skin or underlying tissue, usually over a bone prominence, as a result of pressure or pressure in combination with shear [1]. The development of pressure ulcers due to tissue breakdown and cell necrosis is a significant problem for many patients, including the elderly and those with impaired mobility or paralysis. Pressure ulcers are associated with significant morbidity and even mortality; they can cause pain as well as decreased activities of daily living and quality of life [2]. Therefore this is a pertinent issue for many patients in rehabilitation. Furthermore, they are extremely costly; the burden on the U.S. health care system has recently been estimated at $6 to $15 billion per year [3].
Tissue breakdown is referred to by many terms, including decubitus ulcers, pressure sores, ischemic sores, and bedsores. The term pressure ulcer is the most accurate nomenclature to describe both the cause and nature of chronic, nonhealing wounds due primarily to excessive applied pressure. This term is used throughout the chapter.
The incidence of pressure ulcers among patients in acute care hospitals ranges from 1% to 33%, with prevalence rates of 3% to 69% [4,5]. Higher rates have been associated with increasing age and duration of hospital stay in the elderly [6]. In those with spinal cord injury, individuals with paraplegia are more likely to be rehospitalized because of pressure ulcers [7]. The prevalence of pressure ulcers on admission to skilled nursing facilities ranges between 10% and 26% [8,9]. A multicenter study of pressure ulcer incidence in spinal cord injury conducted across the U.S. Model Spinal Cord Injury System [10] found a significant trend toward increasing pressure ulcer prevalence more recently; the most recent period covered by this study was 2002. A consideration of the risk factors in pressure ulcer development is of vital importance because they contribute to the formulation of treatment and rehabilitation strategies. There are many factors that can lead to the development of pressure ulcers. These can be generally classified as intrinsic factors, which are related to the clinical and physiologic profile of the individual, and extrinsic factors, which are primarily attributed to the external environment (Table 148.1). These intrinsic and extrinsic factors can overlap. They highlight the complex nature of the development of pressure ulcers and are indicative of the need for a holistic and systematic approach to prevent their formation.
Table 148.1
Risk Factors in Pressure Ulcer Development
| Extrinsic Factors | Intrinsic Factors |
| Applied pressure | Reduced or absent sensation |
| Surface shear | Impaired mobility |
| Local microenvironment | Decreased blood flow |
| Muscle atrophy | |
| Poor nutrition | |
| Systemic diseases (e.g., diabetes) | |
| Altered mental status |
Intrinsic Risk Factors
Intrinsic risk factors in pressure ulcer development are related to the conditions of the individual patient. Decreased muscle activity and paralysis lead to loss of muscle bulk, thus reducing soft tissue coverage over the bone prominences of the pelvic and other anatomic regions. As muscle bulk decreases, regional vascularity diminishes and the proportion of avascular fatty tissue increases. Loss of normal muscle tone leads to abnormal responses to environmental stimuli, such as applied pressure, thus increasing the risk for blood flow to become compromised.
Furthermore, motor paralysis will directly affect a person’s ability to respond unconsciously to potential noxious stimuli (e.g., fidgeting while sitting or turning while asleep). Reduced mobility also profoundly alters the individual’s ability to consciously perform postural maneuvers necessary to relieve prolonged applied pressure, from weight shifting while sitting to walking. The loss or reduction of mobility may be further complicated by sensory impairment, leading to the absence or alteration of normal perception of environmental stimuli, such as pain or temperature. Patients with impaired sensation or proprioception are at increased risk for pressure ulcer development because they cannot sense the warning signals that precede tissue damage.
The malnourished patient is at increased risk for pressure ulcer development and will also have an impaired response to healing. Normal tissue integrity depends on correct nitrogen balance and vitamin intake. Protein depletion will lead to decreased perfusion and impaired immune response. The presence of an exuding pressure ulcer will cause massive protein loss, and the patient will move into increasingly negative nitrogen balance. The severity of a pressure ulcer can be directly related to the degree of hypoalbuminemia [11]. Fluid balance must also be considered in conjunction with nutritional status because dehydration will decrease cellular nutrient delivery.
Patients with systemic diseases may be at higher risk of pressure ulcers. For instance, those with renal disease and diabetes may be more prone to pressure ulcer formation because of their peripheral vascular status. The cognitive and mental status of an individual may also affect the ability to perform pressure relief for at-risk body areas, hence potentially increasing the risk of pressure ulcer formation.
Bowel and bladder incontinence causing excessive local moisture may alter the microenvironment of the skin surface, making it more susceptible to maceration and skin breakdown.
Extrinsic Risk Factors
The primary extrinsic risk factor is external applied pressure. Body tissues can support high levels of hydrostatic pressure, such as in deep sea diving. When pressure is the same in all directions, there is no resulting tissue damage. However, nonuniform applied pressures cause tissue distortion, leading to localized tissue damage. This will occur when a patient is in contact with an external load-supporting device, such as a bed or wheelchair. The pressure at the interface between the patient and the support surface must be maintained at a level such that the local blood supply and lymphatic circulation are not impaired. This threshold varies between individuals, and a specialized support system is often required in high-risk individuals, such as acute spinal cord–injured patients.
Any external load that can cause tissue distortion is also likely to cause shear stresses. When only shear forces are present, slipping occurs, and tissue damage will be minimized. However, shear and normal applied loads generally tend to occur together. The normal applied load required to occlude blood flow can be halved when shear forces are also present [12]. Significant clinical problems can arise from propping patients up in bed at angles of less than 90 degrees. In contrast, in the side-lying position, it has been found that blood flow is severely impaired by fully lying on the trochanteric region; but at a partial, 30-degree side-lying position, blood flow is maintained [13].
Symptoms
The primary symptoms of a pressure ulcer are due to an area of persistent tissue breakdown involving the skin and underlying tissues. The patients may complain of an open area in the skin, drainage, bleeding, odor, fever, and pain. The severity of pressure ulcers has traditionally been characterized by the extent of breakdown, as described by a staging system.
Physical Examination
Physical examination for a pressure ulcer starts with an overall assessment of the risk factors of the individual and his or her environment. During general examination, evaluation of overall strength, muscle tone, spasticity, range of motion, and presence of contractures is important. Abnormalities in these areas can contribute to both the development and the persistence of pressure ulcers. In addition, it is important to note whether the individual is malnourished, anemic, incontinent of feces or urine, cognitively impaired, or immobile from medical conditions such as stroke or spinal cord injury as well as whether appropriate pressure-relieving surfaces for seating and sleeping have been used. The Braden Scale is a commonly used nursing risk assessment tool to determine whether an individual is at risk for pressure ulcer development [14]. An individual with a score of 18 or lower is found to be at risk. A systematic approach to the examination of the pressure ulcer is necessary to provide accurate assessment and monitoring of the pressure ulcer. The following parameters are to be noted:
• Size of the pressure ulcer (length to be measured as the maximum measurement craniocaudally; width as the maximum measurement from side to side; depth to be measured at the deepest part of the wound perpendicular to the skin surface)
• Staging of the ulcer
• Presence of undermining or tunneling
• Ulcer bed appearance
• Presence of necrotic materials, slough, eschar, fibrous tissues
• Presence of rolled wound edges
• Presence and amount of drainage (exudate versus transudate)
• Presence of foul odor
• Health of the periulcer tissues, including any surrounding erythema, maceration, edema, or associated fungal infection
Staging of pressure ulcers describes the extent of tissue breakdown at initial examination. There have been multiple staging systems for pressure ulcers. The National Pressure Ulcer Advisory Panel (NPUAP) and European Pressure Ulcer Advisory Panel (EPUAP) have agreed on the following staging system [1].
In addition, the EPUAP/NPUAP recommends use of the following categories/stages.
This staging system can be used only for initial description of the wound. It cannot be used for repeated assessments or reverse staging, primarily because it is not a physiologic description and cannot characterize what is happening in a healing wound. Reepithelialization will occur before lost muscle, subcutaneous fat, or dermis is replaced, resulting in mistakes when healed wounds are staged again.
Care must also be taken in the evaluation of the skin of patients with darkly pigmented skin. Sprigle and colleagues [15] found that erythema in subjects with dark skin is more likely to be nonblanching and to have poor resilience. This indicates that clinicians should use persistence of erythema rather than blanching status to judge incipient pressure ulcers. The staging system defined here includes both visual and nonvisual indicators in the definition of a stage I ulcer, in part to address this issue.
All pressure ulcers are associated with some degree of bacterial colonization, which may or may not lead to local wound infection. The presence of bacterial biofilms in the wound bed may be both a cause and effect of delayed healing [16,17]. Biofilms are typically polymicrobial and are not detected by routine clinical microbiology. They may inhibit healing even in the absence of clinical signs of infection [18]. The possible clinical signs and symptoms of local infection include increasing pain in the wound; erythema, edema, and heat of the periwound area; foul odor; and purulent drainage [19]. Individuals with spinal cord injury may not have intact sensation; in such cases, infected wounds are painless but can cause systemic responses, such as autonomic dysreflexia.
Pressure ulcers also frequently exhibit wound drainage. However, this drainage is not necessarily due to wound infection, and unless it is clinically indicated, routine wound swab culture may not be warranted because this would give a false-positive result. On the other hand, in some cases, increased volumes of exudate may indicate wound infection. Systemic infection may develop if the initial local wound infection is not adequately treated. In such cases, patients may exhibit fever, malaise, and chills. Cellulitis, osteomyelitis, and bacteremia may also develop.
Manual measurement of the wounds by length, width, and depth is the conventional method, but there is poor interrater reliability and the actual surface area of the wound is not known. Electronic technologies allow more accurate documentation and measurements of the surface areas; for instance, the Visitrak device allows easy measurement of wound surface area by a tracing method (Fig. 148.1) [20]. Newer digital stereophotogrammetry systems, such as the LifeViz (Quantificare, San Mateo, Calif) (Fig. 148.2) and Silhouette (ARANZ Medical Ltd, New Zealand) systems, can also provide three-dimensional wound geometry (Fig. 148.3).



Once a pressure ulcer develops, it must be examined regularly for treatment progress to be monitored. At the minimum, weekly assessments should be performed to ensure that the treatment plan is having the desired effect. The NPUAP Pressure Ulcer Scale for Healing (PUSH Tool) has been developed as a clinical tool to monitor changes in pressure ulcer status over time [21]. It takes into account the length and width, exudate amount, and tissue type, forming a composite score that can be tracked over time. The Bates-Jensen Wound Assessment Tool is a more comprehensive tool that takes into account 12 parameters, including periwound tissue and epithelialization status [22]. These tools have been validated and are used in clinical practice.
Once they are evaluated, it is critically important for pressure ulcers to be clearly documented in medical records. In the United States, accurate identification and documentation of pressure ulcers are required for reimbursement in addition to provision of appropriate patient care. Gunningberg and Ehrenberg [23] found that pressure ulcer prevalence determined by audit of clinical records is less than 50% of the rate found when the patient’s skin is examined. Electronic point-of-care wound documentation has the potential to improve wound management with easy-to-use information technology [24]. Dahlstrom and colleagues [25] reported that education on pressure ulcer documentation improved the quality of pressure ulcer documentation by clinical staff. Unfortunately, the same study showed that the implementation of electronic medical records for nursing notes can have a detrimental impact on pressure ulcer documentation in the longer term. This highlights the importance of accurate wound documentation with well-designed templates in the electronic medical record together with ongoing quality improvement.
Functional Limitations
If a pressure ulcer develops, functional limitations are generally exacerbated. For example, the mobility status of a wheelchair user who develops an ischial region pressure ulcer may be affected because treatment can potentially require prolonged periods of total bed rest. Less obvious is a hemiplegic patient who always rolls and pivots to one side to get out of bed; if a greater trochanter pressure ulcer develops on the side that is aggravated by the pressure, shear, and friction of getting out of bed, either that individual will be limited in being able to get out of bed independently or a new technique must be explored.
The development and location of a pressure ulcer may sometimes give an indication of changes in the patient’s activity level. For example, an active wheelchair user may develop an ischial region pressure ulcer from sitting for long periods without adequate pressure relief. However, if that same individual presented with a trochanteric pressure ulcer, most likely due to lying in bed for long periods, the clinician would question whether the patient is not getting up and about for physical or mental health reasons that may need further exploration. Changes in body mass should also be evaluated to determine whether the wheelchair and cushion are still appropriate; if a patient gains weight, the wheelchair and cushion can become too narrow, and increased pressures may develop at the greater trochanteric areas because of impingement.
The development of a pressure ulcer will affect many aspects of a patient’s daily living activities. Patients in active rehabilitation programs may not be able to participate in therapy; independent mobility and transfers will be restricted, and it may not be possible for appropriate bracing or orthotics to be worn.
Diagnostic Studies
It is well accepted that malnutrition is linked to both the development of pressure ulcers and their ability to heal. A nutritional assessment that indicates malnutrition is a serum albumin level of less than 3.5 g/L, total protein level of less than 6.4 g/dL, or body weight decreased by more than 15% since the prior assessment. Prealbumin has a short half-life of only 2 or 3 days. Prealbumin concentration is an even more sensitive measure than serum albumin level and should be obtained in the determination of acute response to nutritional intervention. A nutritional assessment should be repeated every 12 weeks [10]. It has been proposed that the Mini Nutritional Assessment tool may be a reliable questionnaire-based approach to obtain repeated evaluations in the elderly [26].
Anemia is another important factor that may affect pressure ulcer healing. Therefore, appropriate management of anemia may positively influence the healing of pressure ulcers.
Once a patient has a pressure ulcer, the determination of whether bacterial infection, underlying osteomyelitis, related abscess, or sinus tracks are hindering the healing process becomes important. There are many studies that can help us determine the diagnosis of osteomyelitis. High serum erythrocyte sedimentation rate and C-reactive protein level, although nonspecific, may be an indication of osteomyelitis. Plain radiography of the underlying bone, computed tomography, bone scan, and magnetic resonance imaging can all be used to better assess the underlying and surrounding tissue and bones for possible associated complications. The proper imaging for each patient depends on the history and desired focus of the study. The most definitive and yet most invasive diagnostic study is bone biopsy. This can be done either bedside with a needle or in the interventional radiology suite or the operating room. Culture of the bone biopsy specimen will give the most accurate microbiologic diagnosis of the underlying osteomyelitis, allowing use of the most specific antimicrobial agent for treatment. Routine swab culture of the wounds is not recommended because all wounds are colonized with bacteria; such cultures will only bring about false-positive results, leading to unnecessary and inappropriate antimicrobial treatments.
Matrix metalloproteinases are produced by the wound and inflammatory cells during normal wound healing. However, when they are present in excessive quantities, they have a negative effect on wound healing [27]. Therefore, regulation of excessive matrix metalloproteinases through local treatments such as collagen-based dressings may facilitate healing [28]. Bedside diagnostic testing has been developed to determine protease activity in the wound to facilitate the [29].
Treatment
Initial
Unfortunately, pressure ulcers remain one of the most common reasons for readmission to the hospital for many patients with impaired mobility. The patient with a major pressure ulcer will require an average of 180 days of nursing time. Allman and colleagues [30] found that development of a nosocomial pressure ulcer was associated with significant and substantial increases in both hospital costs and length of stay in a group of patients admitted to the hospital with reduced mobility due to a primary diagnosis of hip fracture. Xakellis and Frantz [31] found that the cost of treating pressure ulcers was greatly increased when a patient required hospitalization. Therefore prevention is key to the management of pressure ulcers.
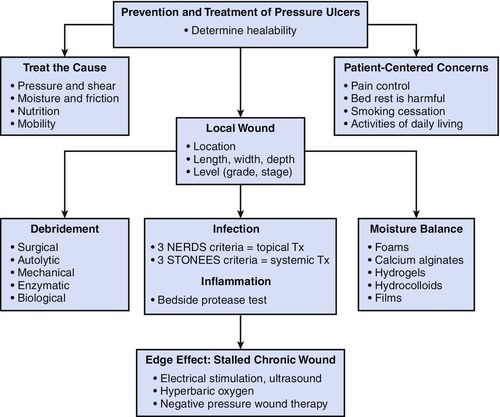
Both the NPUAP/EPUAP [32] and the Consortium for Spinal Cord Medicine [33] have issued comprehensive clinical guidelines for the prevention and treatment of pressure ulcers. Prevention of pressure ulcers aims to address the risk factors listed before. Once a pressure ulcer develops, therapy must focus on local management of the ulcer and systemic treatment of the factors that may affect the healing rate while concurrently addressing factors that led to ulcer formation. Local management of the pressure ulcer should follow the TIME framework for wound bed preparation: tissue (nonviable or deficient) management, inflammation (and infection control), moisture (imbalance), and edge (nonadvancing or undermined) [34]. This framework systematically addresses wound bed preparation to optimize healing conditions. Following this framework, nonviable tissue will be débrided. Inflammation or infection will be addressed by appropriate methods, such as the use of an antimicrobial dressing (e.g., silver dressing). Moisture imbalance will be addressed by the retention or removal of fluid by appropriate dressings. Nonadvancing edges will be addressed by the use of débridement, skin grafts, biologic agents, or adjunctive therapies. Figure 148.4 demonstrates the paradigm modified from Sibbald and coworkers [35]; it provides a helpful guideline for chronic wound preparation for treatment.
Wound irrigation with normal saline must be done with adequate pressure to be effective for wound cleaning and mechanical débridement; the pressure of 4 to 15 psi has been found to be safe and nontraumatic to the wound bed. This can be achieved with an appropriate syringe or a pulsatile lavage [36] device that produces irrigation pressure within this recommended range.
With regard to systemic treatments, positioning should be evaluated in both the lying and seated positions. Patients should be positioned to avoid direct pressure and shearing force on the ulcer area (see the section on extrinsic factors). Immobile patients in bed should be turned on a scheduled basis, at least every 2 hours. If necessary, pillows or foam wedges should be used to help patients maintain a position that keeps the ulcer area pressure free. Multiple mattresses and overlays are available, depending on the patient, extent and location of the pressure ulcer, and goals of therapy. For the individuals who can tolerate lying prone, use of a prone cart allows the patient to be out of bed but avoids any pressure on the sacral area. Sitting should be avoided if pressure cannot be relieved from the ulcer area in the sitting position.
The comorbid conditions shown to delay ulcer healing are peripheral vascular disease, diabetes mellitus, immune deficiencies, collagen vascular diseases, malignant neoplasms, psychosis, smoking, and depression. Identification and treatment of these conditions in patients with pressure ulcers are important.
If malnutrition is a factor, aggressive nutritional supplementation or support should be instituted to place the patient into a positive nitrogen balance. Nutritional support should occur if it is likely to change the patient’s prognosis. Supplemental arginine, vitamin C, and zinc have been shown to enhance the rate of pressure ulcer healing in patients with low serum albumin and zinc levels and elevated C-reactive protein concentration [37].
Pain should also be addressed and treated appropriately. Some pain may be eliminated or controlled by covering the wound and appropriate positioning. If the pain persists, analgesia is provided as needed during manipulations of the wound and for chronic wound pain.
Within 1 to 2 weeks of the initiation of treatment, partial-thickness pressure ulcers should show signs of healing. Full-thickness ulcers should show reduction in size after 2 to 4 weeks of treatment. This should be determined with some caution; pressure ulcers often appear to be initially larger after treatment because of the effect of débridement and cleaning, exposing the real extent of ulceration. There also appears to be a proportion of pressure ulcers that develop as the result of deep tissue damage, at the interface between the soft tissues and the bone rather than at the skin surface. These ulcers will often progress to full-thickness ulcers even when appropriate intervention is provided and should be treated more aggressively.
With this in mind, if the ulcer is truly not healing, the different aspects of the treatment plan previously outlined should be reviewed. In addition, biophysical therapies, such as electrical stimulation, ultrasound, hyperbaric oxygenation [38], or negative pressure wound therapy, should be considered together with the possible need for surgical intervention for stage III and stage IV ulcers that are recalcitrant to standard therapy. Electrical stimulation has been shown in multiple studies to improve the rate and degree of healing when it is used in addition to standard interventions on recalcitrant ulcers [32]. Negative pressure wound therapy, such as vacuum-assisted closure, may also be useful for the appropriate wounds. The guidelines for the use of vacuum-assisted closure are as follows [39]:
• There is no untreated, underlying osteomyelitis.
• The wound is free of fistulas to internal organs or body cavities.
• The wound has not decreased in size for 2 to 4 weeks, despite the use of best practices.
• The wound has been sufficiently débrided.
• The wound has not decreased in size by more than 30% 4 weeks after major débridement.
Many different therapeutic modalities for the treatment of pressure ulcers are being investigated, such as growth factors and tissue-engineered skin substitutes. Basic science research continues to increase our understanding of the chronic wound pathogenesis and can guide the development of clinical interventions. Clinical research in the field of wound treatment is broadening the options for both the treatment and prevention of wounds through many different pathways.
Rehabilitation
Many of the major factors that increase susceptibility to pressure ulcer development are interrelated intrinsic changes in body characteristics and functional abilities. In many conditions, these changes are irreversible. Nutritional status can be altered by adequate diet, but a complete spinal cord injury is permanent. Clinical approaches to pressure ulcer prevention generally focus on extrinsic factors that can be changed. These include educational methods, device-oriented methods, and comprehensive systems of preventive care. These approaches to pressure ulcer prevention are complementary and should be reviewed periodically.
It is critically important during initial rehabilitation that every patient and caregiver be thoroughly educated in the causes of pressure ulcers and what they should do to prevent them. Skills to be learned include the ability to carry out a pressure relief regimen, both through postural changes, when possible, and through the provision of appropriate equipment (e.g., cushions, wheelchairs, mattresses). The need for routine skin inspection and care must also be emphasized, with particular regard to pressure areas such as the ischii, sacrum, greater trochanters, heels, and occiput. Increased care contact time is associated with reduced pressure ulcer incidence, although automated pressure relief systems can also provide an effective intervention during inpatient rehabilitation. Turning every 2 hours while in bed is a commonly accepted practice, but the evidence to support this turning frequency is still lacking. After initial rehabilitation, the at-risk patient must maintain a high level of skin care at all times to prevent the occurrence of pressure ulcers.
The provision of appropriate equipment for postural support and pressure relief, such as mattresses and wheelchair seating cushions, is an important component of rehabilitation. For a patient with impaired mobility who is being discharged to the community or to long-term care, this requires the selection of a wheelchair seating system, including both a wheelchair and a support cushion, to meet his or her individualized requirements. An inappropriate seating system can lead to poor posture, reduce functional abilities, and isolate the user from the environment. All these factors can in turn exacerbate the risk for pressure ulcer development in the rehabilitating patient.
Seating requirements of each patient must be thoroughly assessed during acute rehabilitation and when he or she presents with a pressure ulcer so that appropriate seating and other support surfaces can be recommended. Special seating and cushions are available to help distribute weight off of a pressure ulcer. Cushions can be divided into four categories: foam, viscoelastic foam, gel, and fluid flotation. Which cushion is best for a patient depends on pressure evaluation, lifestyle, postural stability, continence, and cost [40]. Pressure mapping can be a useful component in the objective determination of the interactions between the seating surface and the skin, helping the clinician to choose the most appropriate seating surface with the best pressure-relieving properties. Pressure relief maneuvers should be done every 15 minutes while the patient is sitting to prevent the development of ischial region pressure ulcers.
Tertiary prevention of pressure ulcers seeks to decrease the number of patients who exhibit chronic recurrence of tissue breakdown. Device-oriented prevention techniques continue to be developed and refined. Active pressure relief mattresses often incorporate temperature sensors to control the microenvironment, and this type of technology is now starting to be applied in wheelchair cushions. Wheelchair cushions that can dynamically alter pressure distribution at the seating interface may provide a method for pressure ulcer prevention in individuals with compromised mobility. Advances in system components have increased the reliability and robustness of these cushions, although they remain relatively expensive. Advanced technologies and new pharmacologic approaches are being explored that can affect the intrinsic clinical status of at-risk patients. The long-term application of implanted electrical stimulation devices offers a unique means to alter the intrinsic characteristics of paralyzed muscle, leading to sustained improvements in regional tissue health [41]. The use of anabolic steroids has also been investigated for both the treatment and prevention of pressure ulcers in the population with spinal cord injury [42].
In addition to altering the intrinsic susceptibility of at-risk patients, the incidence of pressure ulcers may be decreased by ensuring effective delivery of care and education by a multidisciplinary clinical team, at all stages of rehabilitation. A survey of the prevalence of pressure ulcers in 5000 hospitalized patients throughout Europe, carried out by the EPUAP [43], indicated that clinical expertise and standard treatment guidelines are not in themselves sufficient. They should be considered the starting point for effective prevention of pressure ulcers, rather than the endpoint. Personalized interactive programs have the potential to decrease readmission rates for high-risk individuals. An increase in the involvement of the patient in his or her care whenever possible may also decrease susceptibility to pressure ulcer development.
Outpatients at risk for pressure ulcers, such as residents of long-term care facilities, often have restricted ease of community mobility that limits both their desire and ability to access clinical expertise. Telemedicine represents a relatively new model for health care delivery that can eliminate or greatly reduce the need for transportation of the patient and improve standard of care.
Procedures
Débridement of necrotic tissue from the wound is essential for healing to occur. Débridement can be accomplished by several different approaches. Sharp débridement is performed by a qualified clinician who uses a scalpel either at the bedside or in surgery. Mechanical débridement is commonly done with wet to dry dressings changed two or three times a day. Autolytic débridement permits the enzymes in the wound to dissolve the necrotic tissue by covering of the wound with a moisture-retentive dressing. Last, enzymatic débridement uses exogenous enzymes in commercial preparations, such as papain, to dissolve the necrotic tissue. The determination of débridement method depends on the condition of the wound. Sharp débridement is often performed when there is a large amount of necrotic material; for instance, the presence of eschar tissue often leads to sharp débridement. This will allow efficient removal of necrotic materials from the wound. However, for chronic wounds that do not have easily removable necrotic tissues (e.g., adherent, yellow, necrotic tissues at the base of the wound), enzymatic débridement through the use of collagenase may be the method of choice, allowing nontraumatic débridement of the wound.
Surgery
A variety of surgical options are available to close stage III and stage IV pressure ulcers that do not heal by conservative means. Possible surgeries are as follows: direct closure, split- or full-thickness skin grafts, skin flaps, musculocutaneous flaps, and free flaps. The type of surgical repair depends on the location of the ulcer, the primary diagnosis of the patient, the comorbid conditions, and the goals of treatment. The long-term outcomes of surgical intervention are variable [44]. Predictors of surgical success correlate with the compliance of the patient with postoperative bed rest as well as preoperative risk factors for wound healing.
Potential Disease Complications
The following complications are associated with pressure ulcers: bacteremia, osteomyelitis, cellulitis, amyloidosis, endocarditis, heterotopic bone formation, perineal-urethral fistula, pseudoaneurysm, septic arthritis, sinus track or abscess, and squamous cell carcinoma in the ulcer.
Potential Treatment Complications
Failure to heal and recurrence of pressure ulcers are potential treatment complications. The need to maintain pressure relief over the area of the ulcer may lead to the formation of another pressure ulcer in a different location. Asymmetric sitting posture due to unilateral removal of necrotic bone may cause pressure ulcer development.
Prolonged bed rest and reduced activity levels will decondition the patient and may lead to or exacerbate other comorbidities. Increased pain may occur with dressing changes and sharp or mechanical débridement. Surgical complications of infection, bleeding, and wound dehiscence are possible.