CASE 145
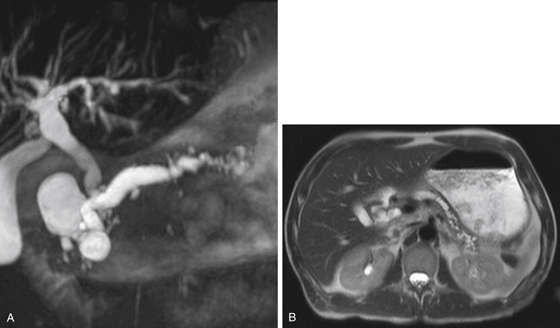
History: A 49-year-old man with chronic alcoholic pancreatitis presents with increasing right upper quadrant pain. Liver function tests show increased bilirubin.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the tumor most commonly diagnosed in association with dilation of the pancreatic duct?
A. Glucagonoma of the pancreaticoduodenal groove
B. Ductal adenocarcinoma of the pancreatic head
C. Ampullary duodenal adenocarcinoma
D. Intraductal papillary mucinous tumor
3. What is the significance of signal poor filling defects within a dilated pancreatic duct on magnetic resonance cholangiopancreatography (MRCP)?
4. Which statement regarding imaging of chronic pancreatitis is true?
ANSWERS
CASE 145
MRCP of Chronic Pancreatitis
1. C and D
2. B
3. C
4. B
References
Matos C, Winant C, Deviere J. Magnetic resonance pancreatography. Abdom Imaging. 2001;26(3):243–253.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 158.
Comment
The considerable controversy regarding the role of MRCP in the work-up of biliary and pancreatic lesions can be summed up with this straightforward question: Will MRCP replace ERCP? The question begs an answer, in that any noninvasive diagnostic procedure that has the potential to replace an invasive procedure and achieve the same results is a straightforward patient care issue. ERCP is currently considered the gold standard for diagnosis of biliary obstruction and some pancreatic processes. However, ERCP carries with it the same risks of bowel perforation as routine endoscopy.
MRCP is often used after failed ERCP or in patients who might not tolerate ERCP. However, this situation may change. No patient preparation is required for MRCP, usually no sedation is necessary, and contraindications of MRCP are fewer than ERCP. Because of all this, studies to compare the sensitivity and specificity of the two techniques are ongoing. The initial results suggest that MRCP is a comparable examination for diagnostic purposes to ERCP without many of the associated risks (see figures). However, ERCP can also be an interventional procedure (e.g., used to place a stent or remove a stone) and will remain an important part of biliary-pancreatic medicine.