CASE 145

History: A patient presents with cyanosis.
1. What should be included in the differential diagnosis in a patient with cyanosis and increased pulmonary vascularity? (Choose all that apply.)
A. Transposition of the great arteries
B. Total anomalous pulmonary venous connection
C. Double-outlet right ventricle
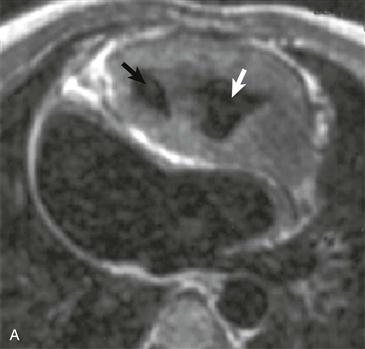
2. What structure is indicated by the black arrow in Fig. A?
3. What structure is indicated by the white arrow in Fig. A?
4. What is the most likely diagnosis?
A. Transposition of the great arteries
B. Total anomalous pulmonary venous connection
ANSWERS
Reference
Reddy GP, Higgins CB. Magnetic resonance imaging of congenital heart disease: evaluation of morphology and function. Semin Roentgenol. 2003;38(4):342–351.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 322–324.
Comment
Anatomy and Associated Anomalies
Double-outlet right ventricle is a rare admixture lesion that causes shunt vascularity and cyanosis. Atrial and ventricular septal defects usually coexist with this anomaly, and about 75% of patients have some degree of pulmonic stenosis or atresia. Several coronary artery anomalies may coexist with double-outlet right ventricle, including anomalous origin of the right coronary artery from the left coronary artery, anomalous origin of the left anterior descending coronary artery from the right coronary artery, and duplication of the left anterior descending coronary artery.
Imaging
Radiographs typically show shunt vascularity and cardiomegaly. The diagnosis is made by ascertaining that both great arteries arise from a muscular infundibulum, indicating a right ventricular origin. In most patients, the aorta is to the right of the main pulmonary artery (so-called D-malposition). The diagnosis can be made with echocardiography in most patients. MRI readily demonstrates the pathologic anatomy and is helpful in making the diagnosis of double-outlet right ventricle (Figs. A and B) in equivocal or confusing cases. MRI also accurately depicts the size and orientation of the ventricular septal defect, which guides surgical management.
Treatment
The major goal of treatment is to restore biventricular function, and surgery is usually performed before the first birthday. The surgical approach varies depending on the orientation of the ventricular septal defect. Complications of surgery include subaortic stenosis, severe pulmonic regurgitation with right ventricular dysfunction, and pulmonic outflow tract obstruction. These complications vary depending on the surgical approach.