CHAPTER 143
Plexopathy—Brachial
Erik Ensrud, MD; John C. King, MD; John D. Alfonso, MD
Definition
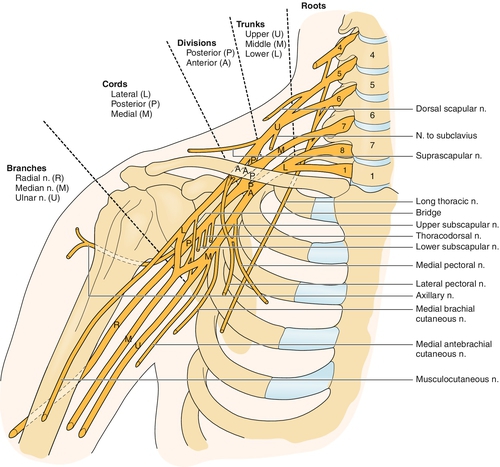
Brachial plexopathy is the pathologic dysfunction of the brachial plexus, a complex peripheral nerve structure in the proximal upper extremity. The brachial plexus starts just outside the spinal cord in the lower neck and extends to the axilla. The total average brachial plexus length is approximately 6 inches [1]. The plexus is divided into five sections: roots, trunks, divisions, cords, and branches or terminal nerves. The spinal nerves C5 through T1 classically supply anterior primary rami of the nerve roots, which then form the plexus. Variations in nerve root supply that involve other nerve roots are said to be expanded. When the C4 nerve root also supplies the brachial plexus and T1 contribution is minimal, the plexus is called prefixed. When the T2 nerve root supplies the brachial plexus and C5 contribution is minimal, the plexus is said to be postfixed [2]. The nerve roots combine to form the trunks behind the clavicle. There are three trunks, the upper, middle, and lower. The upper is formed from the C5 and C6 nerve roots, the middle is a continuation of C7, and the lower is formed from C8 and T1. The trunks then divide behind the clavicle into anterior and posterior divisions. Just inferior to the clavicle, the divisions coalesce into cords. The cords travel along the axillary artery, just inferior to the clavicle, and are named for their spatial relationship to the artery. The posterior cord is formed from the union of the three posterior divisions. The lateral cord is formed by the union of the anterior divisions of the upper and middle trunks. The medial cord is the continuation of the anterior division of the lower trunk. Nerve branches are the most distal elements of the brachial plexus and are the major nerves of the upper extremity. These branches begin in the distal axilla and other than the median nerve, which is formed by contributions from the medial and lateral cords, are continuations of the cords. There are also numerous peripheral nerves that arise directly from the roots, trunks, and cords (Fig. 143.1).
Brachial plexopathy can be due to wide-ranging causes, including idiopathic, iatrogenic, autoimmune, traumatic, neoplastic, and hereditary. It can occur in any age group; but other than when it is secondary to obstetric trauma, it usually occurs from the ages of 30 to 70 years. Men are affected two to three times as often as are women, and the reason is likely due to their more frequent participation in vigorous athletic activities that can lead to trauma. About half of the cases have no identified precipitating event; in others, brachial plexopathy follows an antecedent infection, trauma, surgery, or immunization.
Symptoms
Brachial plexopathy can result in symptoms of pain, weakness, and numbness, both at the level of the brachial plexus and distally in the supplied upper extremity. The area of pain and other symptoms correlates with the portion of the brachial plexus involved and the specific nerve elements from that area. Depending on the cause of the plexopathy, symptom onset can range from sudden to insidious. Because of the complex muscle suspension of the shoulder joint, chronic brachial plexopathy may result in glenohumeral subluxation and instability due to stretching of the shoulder capsule. Brachial plexopathy usually does not cause prominent neck pain. Some brachial plexopathies may occur bilaterally and therefore cause symptoms in both upper extremities.
Physical Examination
The physical examination of the brachial plexus for brachial plexopathy must be thorough because of the complexity of its structure and function. The shoulder girdle and entire extremity need to be exposed during examination to allow close inspection of muscle bulk and fasciculations. Assessment of atrophy of muscles is often assisted by side-to-side comparisons. Muscle strength examination needs to be thorough and to include proximal muscles not commonly tested, such as infraspinatus, supraspinatus, rhomboids, and serratus anterior. Sensory testing also must be thorough, with both dermatomal and peripheral nerve sensory distributions examined. A musculoskeletal examination of the shoulder joint is helpful; joint disease can be both a possible primary cause of pain and a secondary effect of plexopathy. Shoulder range of motion and signs of tendinosis as well as reflexes and any muscle atrophy need to be assessed. The lack of pain exacerbation with neck movement and multiroot distribution of sensory or motor deficits can help distinguish brachial plexopathy from cervical radiculopathy, which more commonly affects a single root [3]. It is often not possible to determine the exact location of a brachial plexus lesion from physical examination, but the examination is usually helpful in focusing electrodiagnostic and radiologic testing.
Functional Limitations
Depending on whether the brachial plexopathy involves the upper plexus, lower plexus, or entire plexus, the proximal shoulder muscles, the distal muscles involved in fine finger movements, or the entire extremity can be weak or numb. Activities of daily living, such as dressing, feeding, and grooming, can be significantly affected. These impairments can result in disabilities in many activities, including computer use, writing, and driving. Brachial plexopathy secondary to birth trauma may subsequently cause difficulty for children and teens with sports and other recreational activity.
Diagnostic Studies
Electromyography (EMG) can be helpful in localizing the pathologic area in brachial plexopathy as well as in determining the severity of axonal injury and the potential for recovery. However, many brachial plexopathies cannot be definitely localized by EMG because of subtle findings encountered with incomplete nerve injury and the complexity of plexus-related innervation. The nerve conduction and needle EMG assessment is best directed by both symptoms and physical examination findings. Both nerve conduction studies and needle EMG are required for complete assessment. Sensory nerve conduction studies can help in localization by the pattern of abnormalities seen and in judging injury severity based on reductions of amplitudes or absence of potentials. The nerve conduction study may not detect abnormality if the lesion is mild in severity or too recent to allow axonal degeneration.
The following five basic sensory nerve conduction studies are suggested as a screen for brachial plexus evaluation: lateral antebrachial cutaneous, median recording from the thumb, median recording from the index finger, superficial radial, and ulnar recording from the little finger [2]. The presence of fibrillation potentials in EMG is particularly sensitive for motor axon loss and helps localize the site of lesions. The choice of muscles sampled on EMG is usually focused on the area of interest, but other areas are also included for the exclusion of wider disease. It is important to include paraspinal muscles of the relevant areas to investigate the possibility of radiculopathy (paraspinals are supplied by the posterior primary rami of the nerve roots, which do not supply the brachial plexus). EMG evaluation of the brachial plexus is complex and best performed by experienced electromyographers.
Radiologic studies of the plexus are helpful to evaluate the severity of trauma, presence of mass lesions, and inflammation of the brachial plexus nerve elements [4]. Magnetic resonance imaging (MRI) has become the study of choice in evaluation of traumatic brachial plexus injuries [5]. More than 80% of traumatic nerve root avulsions will show pseudomeningoceles, which are tears in the meningeal sheath surrounding the nerve roots that allow extravasation of cerebrospinal fluid into nearby tissues. They appear bright on T2-weighted images. MRI is also the most useful study for evaluation of other causes of brachial plexopathy, such as tumors, both secondary and primary [6]. An early MRI sign in Pancoast tumor is obliteration of the interscalene fat pad, which is best visualized on coronal T1-weighted MRI [7]. Inflammatory changes in the brachial plexus may be visualized with MRI, including brachial neuralgic amyotrophy [8].
Computed tomography myelography is increasingly becoming the study of choice in the preoperative evaluation of infants with obstetric brachial plexopathy, given its usefulness in identifying nerve root avulsion, which affects operative interventions [9,10].
Musculoskeletal ultrasonography has been used in the evaluation of suspected neoplastic brachial plexopathy. Sonography may identify the neoplastic lesion as a hypoechoic mass or present evidence consistent with a compressive lesion, such as segmental neuronal swelling of the involved portion of the brachial plexus [11].
Chest radiographs are valuable for the evaluation of diaphragmatic paralysis in traumatic brachial plexopathy, which usually indicates an irreparable lesion of the brachial plexus [12].
Differential Diagnosis
Etiology of Brachial Plexopathy
It is helpful to approach the differential diagnosis of brachial plexopathy by the common causes in the different anatomic regions where the brachial plexus is affected. The anatomic areas of interest are the supraclavicular, retroclavicular, and infraclavicular. There are also causes of brachial plexopathy that tend to produce more diffuse plexus injury.
Supraclavicular
Birth Trauma
Lateral deviation of the head and neck to free the infant’s shoulder, during both vaginal delivery and cesarean section, can lead to stretch injury of the upper brachial plexus. Such injuries can also occur from in utero causes, including compression of the fetal shoulder by the maternal symphysis pubis or sacral promontory, as well as by uterine anomalies that result in abnormally elevated intrauterine pressures [13]. The incidence of brachial plexopathy from birth trauma is 0.4 to 4 per 1000 live births [14]. It is called Erb palsy when the C5-C6 nerve roots are affected, resulting primarily in proximal arm weakness. When the C8-T1 roots are affected, the results are hand weakness, called Klumpke paralysis.
Trauma
Most commonly, trauma involves the upper plexus and is especially seen with closed traction, as in “burner” or “stinger” sports injuries (sudden separation of the shoulder and head due to contact) and pressure from backpack straps (“rucksack palsy”). The roots can be stretched but remain continuous, tear, or avulse from the spinal cord as possibilities. More direct trauma, such as from a stab wound or gunshot wound, can affect any portion of the plexus, but the supraclavicular portion is the most susceptible.
Intraoperative Arm Malpositioning
Postoperative brachial plexopathy may result from malpositioning of the arm during surgery [15].
Pancoast Syndrome
An apical lung tumor (usually small cell carcinoma) can extend into the supraclavicular brachial plexus, often being manifested with shoulder pain [16].
Neurogenic Thoracic Outlet
This syndrome is a rare condition in which a fibrous band extends from the lower cervical spine (cervical rib or transverse process) to the first rib. The T1 fibers are deflected and injured further by this fibrous band more than the C8 fibers are.
Infraclavicular
Postirradiation
Radiation therapy directed at the axillary lymph nodes can result in brachial plexopathy, which can occur months to years after radiation therapy. EMG studies may reveal evidence of conduction block and classic myokymia.
Metastatic Lymphadenopathy
A secondary neoplastic injury is usually due to compression from enlargement of involved axillary lymph nodes.
Regional Blocks
Infraclavicular brachial plexus injury has been identified as a complication of axillary regional blocks [17].
Heterotopic Ossification
The growing mass of heterotopic ossification about the shoulder can envelop and compromise the brachial plexus [18]. In midclavicular fractures, brachial plexopathy can be secondary to the initial trauma and also result from the development of heterotopic ossification [18].
Retroclavicular
Midclavicular Fractures
In midclavicular fractures, brachial plexopathy can be secondary to the initial trauma but also can result late from exuberant callus compression of the brachial plexus [18]. Retroclavicular brachial plexopathy, however, is rare and most often occurs in the context of wider spread plexopathy.
Diffuse Localization
Neuralgic Amyotrophy
Also called Parsonage-Turner syndrome, brachial amyotrophy, idiopathic shoulder girdle neuropathy [19], and brachial plexitis, neuralgic amyotrophy is a well-described syndrome of idiopathic monophasic brachial plexopathy that was well characterized by a large case series [20]. The initial symptom is onset during a few hours of severe continuous proximal upper extremity pain, which occurred in 90% of patients in this case series. After the onset of pain, weakness of the extremity usually develops within 2 weeks. Whereas sensory symptoms in the affected extremity are usually less pronounced than pain and weakness, they occur in 70% of patients. Pain decreases first, with an average pain duration of 28 days. Motor recovery begins within 6 months in most patients and with significant functional improvement; but in this case series, more than 70% of patients still had at least mild weakness detected on thorough strength examination at 3 years after weakness onset. Neuralgic amyotrophy can involve any part of the brachial plexus but tends to affect the upper plexus; 49% of patients have shoulder–proximal arm involvement.
Hereditary Neuralgic Amyotrophy
This is a similar condition but with a known genetic etiology, which is often autosomal dominant but is genetically heterogeneous.
Diabetic Cervical Radiculoplexus Neuropathy
Distinct from neuralgic amyotrophy is the recently described diabetic cervical radiculoplexus neuropathy [21]. This condition is associated with type 2 diabetes mellitus. Patients initially develop pain in the upper limb, often acutely, followed later by weakness and sensory changes, such as paresthesias, dysesthesias, or numbness. Associated autonomic symptoms (orthostasis, sudomotor changes) are common, as is weight loss. Electrodiagnosis reveals predominantly axonal neuropathy, whereas biopsy findings of involved nerves show axonal degeneration, ischemic injury, and perivascular inflammation. The condition is typically monophasic with improvement, but 21% of patients demonstrated recurrence [21].
Primary Neoplastic Peripheral Nerve Tumors
Local primary peripheral nerve tumors can cause brachial plexopathies that occur anywhere in the brachial plexus but are rare and usually benign. Benign tumors are typically nerve sheath tumors, either schwannomas or neurofibromas (associated with neurofibromatosis type 1), and cause painless sensory loss and weakness [2]. In contrast, malignant peripheral nerve tumors in the brachial plexus tend to be painful [22,23].
Treatment
Initial
The treatment of brachial plexopathy needs to be customized to the individual patient and the cause of the brachial plexopathy. Pain can be the most disabling symptom but is usually effectively treated with neuropathic pain medications, such as gabapentin and tricyclic antidepressants, and analgesics, such as tramadol and opiates in cases of severe pain. Dosing is usually at the higher end of accepted ranges (such as gabapentin at 600 mg three times daily or more) secondary to the pain severity of acute plexopathy, although duration of therapy may be brief. Levetiracetam has been used successfully to reduce refractory brachial plexopathy pain and to decrease opioid need [24].
Rehabilitation
When the muscles of the shoulder girdle are involved, therapy focused on positioning and shoulder range of motion can prevent secondary complications, such as adhesive capsulitis [25]. Directed exercise can be beneficial, with the caveat that exercise of muscles with neurogenic weakness from brachial plexus lesions to full exhaustion may be counterproductive on the basis of findings in exercise in patients with peripheral neuropathy [26]. Occupational therapy is often indicated when weakness from brachial plexopathy results in loss of function. Adaptive aids can be helpful when they are indicated, such as a shoulder sling to help reduce imbalance from proximal arm weakness from brachial plexopathy. Vocational rehabilitation may be indicated when the resultant disability from weakness affects the patient’s ability to perform in the job setting.
Procedures
Brachial plexus blocks are rarely used but are possible for the treatment of severe pain from metastatic brachial plexopathy or severe acute brachial plexopathy. Increasingly, botulinum toxin injections, combined with surgery, serial casting, and physical and occupational therapy, are used to treat and to prevent shoulder and forearm pronation contractures as well as to optimize elbow range of motion in infants with obstetric brachial plexus injury [27]. However, botulinum use in this scenario has yet to be tested by randomized controlled trials.
Surgery
Surgery is an option in cases of traumatic plexopathy but has variable results. Surgical techniques such as nerve grafting, free muscle transfer, neurolysis, and neurotization are used. Surgeons who use these techniques frequently differ considerably in their approach to them, making conclusions about their efficacy difficult. Surgery is an option in brachial plexus birth injuries, usually when persistent severe motor deficits are present after 3 to 8 months of age. A case series found improvement in surgically treated patients on a shoulder motion scale [28]. The location of injury affects selection of patients for surgery and surgical outcome. For example, postganglionic nerve root avulsion injuries may do better with earlier surgery [29]. Preganglionic avulsions are difficult to repair, but direct implantation into the spinal cord may help some patients [30].
Potential Disease Complications
Weakness from brachial plexopathy can result in joint instability or in joint and musculotendinous contractures of upper extremity joints. Complex regional pain syndrome may follow brachial plexopathy [31]. Secondary depression can be due to pain and loss of function. Insensate limbs are at risk for trauma neglect, infection, and amputation.
Potential Treatment Complications
Stretching and range of motion exercises for avoidance or treatment of contractures can acutely exacerbate neuropathic pain. Care to avoid shoulder impingement during range of motion exercises is important because of weak rotator cuff muscles. Insensate limbs become more susceptible to heat injuries, such as by hot packs or therapeutic ultrasound. Medicines used for brachial plexopathy pain can have side effects, which are specific to the particular medicine used. Surgery for brachial plexopathy may result in nerve or vascular injury.







