CASE 142

History: A 38-year-old woman presents with dyspepsia.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the key vascular finding on CT that suggests midgut malrotation?
A. Relationship between the superior mesenteric artery and vein
B. Left-sided inferior vena cava
D. Persistent vitelline artery
3. What is the most common presentation of symptomatic midgut malrotation?
A. Newborn less than 1 month old with acute vomiting
B. Child less than 1 year old with abdominal pain
C. Child more than 1 year old with intermittent vomiting
4. Malrotation is associated with heterotaxy and various other congenital abnormalities. What is the leading cause of death in these patients?
D. Absence of the pancreatic uncinate process
ANSWERS
CASE 142
Midgut Malrotation
1. A and D
2. A
3. A
4. C
References
Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26(5):1485–1500.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 146.
Comment
The human gut herniates into the umbilicus at about 6 weeks of intrauterine life. This herniation results in 270 degrees of counterclockwise rotation around the superior mesenteric artery before reentering the coelomic cavity at 12 weeks. The process can be faulty in about 1 in 500 live births with failure of achieving the full 270 degrees, resulting in degrees of malrotation abnormality.
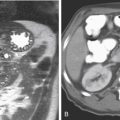
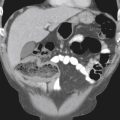
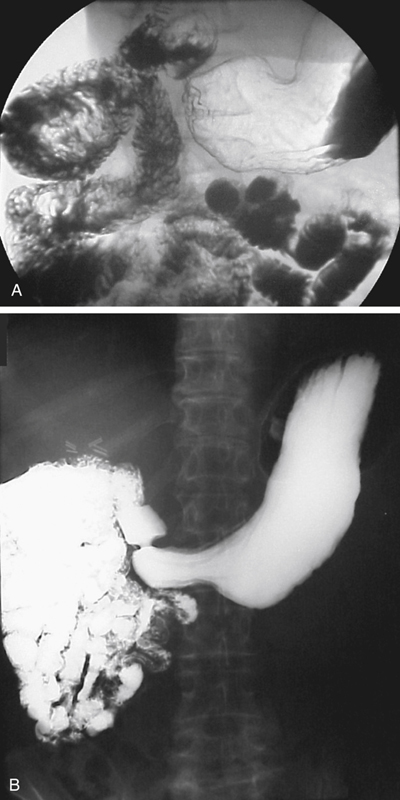
In adults, midgut malrotation often is an incidental finding. The colon is usually found on the left. The small bowel is on the right, and the positions of the superior mesenteric artery and superior mesenteric vein are reversed. In addition, the position of the ligament of Treitz can be located in the midline or the right upper abdomen. About 60% of all symptomatic midgut malrotations are diagnosed by 1 year of age. A barium upper GI study is still the fastest and most inexpensive method of diagnosis (see figures). In some adults, vague symptoms, such as low-grade chronic recurrent abdominal pain and symptoms suggestive of malabsorption, may be present that bring the patient to a diagnostic work-up.