CASE 141


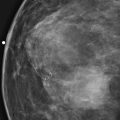
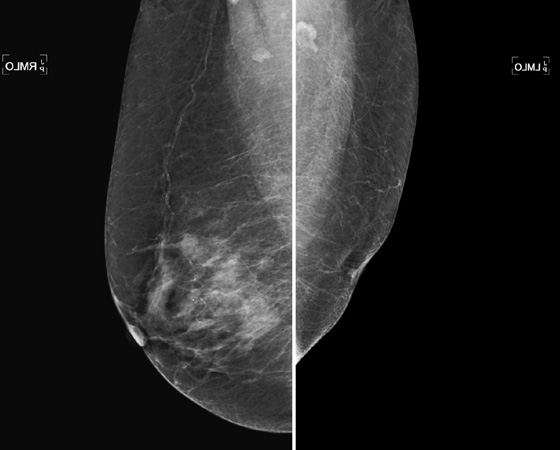
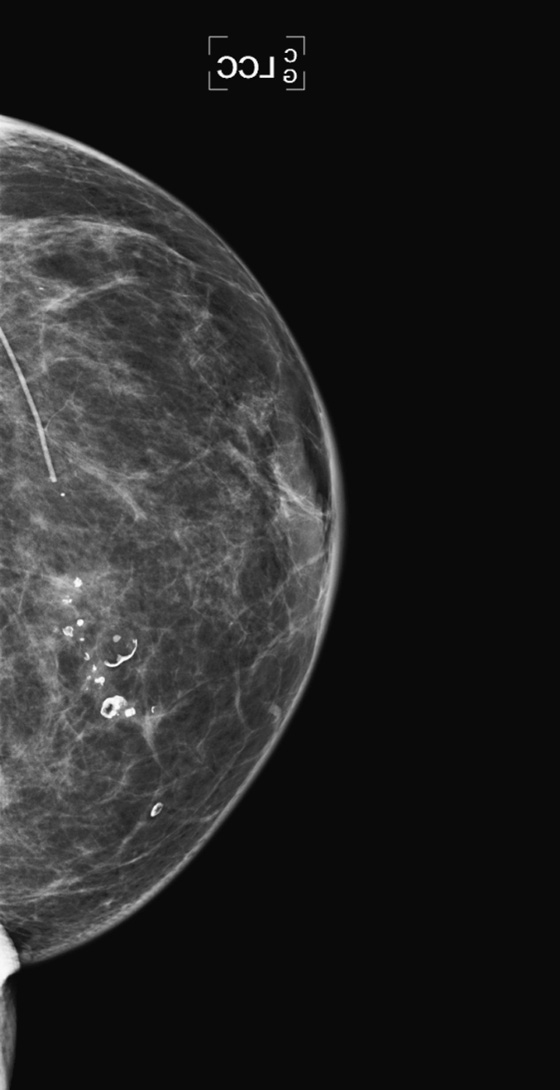
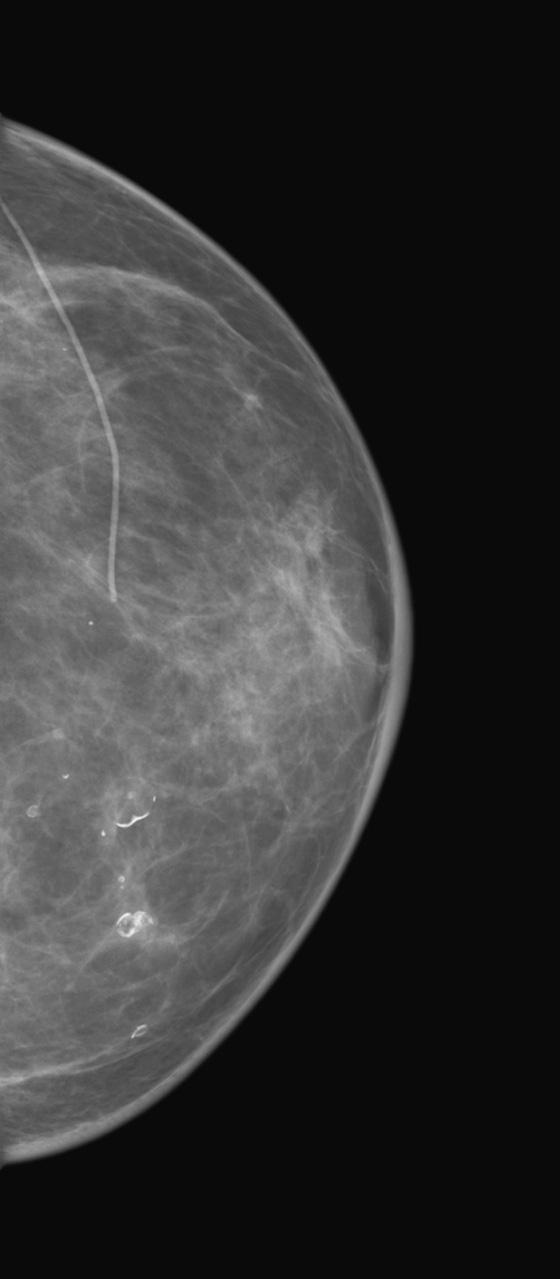
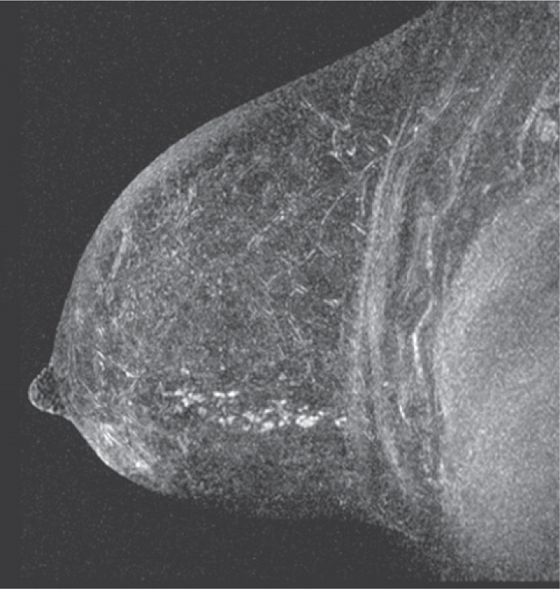
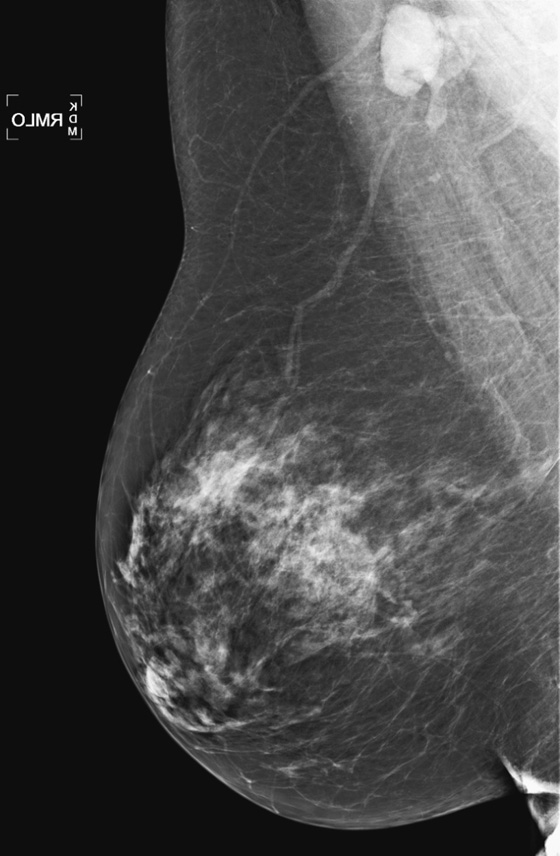
History: A 47-year-old woman presents with a palpable cordlike area in the axillary tail of the left breast. The first figure is the right mediolateral oblique (MLO) view from her mammogram 1 year earlier, when she was asymptomatic. The second figure is the right MLO view from the mammogram taken on the day she presented with her concern.
1. What is the differential diagnosis for the mammogram taken at presentation? (Choose all that apply.)
C. Varicose vein in the breast
D. Superficial thrombophlebitis in the left breast
2. What is the next imaging exam to establish the diagnosis?
A. Perform spot compression views.
B. Perform ultrasound of the palpable concern.
C. Perform MRI to evaluate for abnormal enhancement.
D. Perform magnification views to check for microcalcifications.
3. What would an ultrasound exam show?
A. A dilated, tubular, beaded vein with absence of blood flow
4. What are the clinical signs of this disease?
A. The skin typically is normal.
B. There may be a palpable cord.
C. The finding is usually in the lower outer quadrant of the breast.
D. Both breasts are typically involved.
ANSWERS
CASE 141
Mondor’s Disease
1. C and D
2. B
3. A
4. B
Reference
Conant EF, Wilkes AN, Mendelson EB, Feig SA. Superficial thrombophlebitis of the breast (Mondor’s disease): mammographic findings. AJR Am J Roentgenol. 1993;160:1201–1203.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:399.
Comment
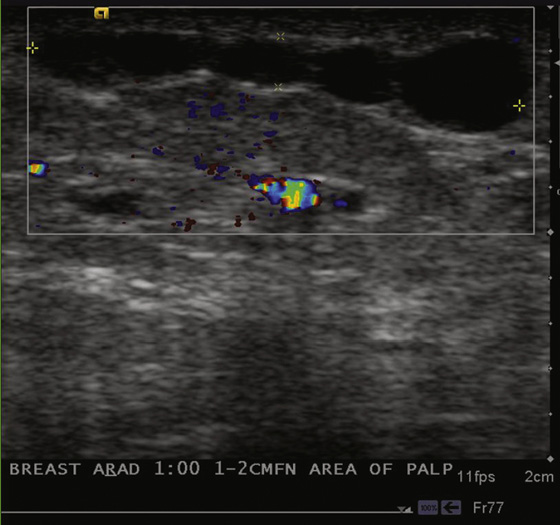
Mondor’s disease is a focal, superficial thrombosis of a vein in the breast. It is typically in the upper outer quadrant or axillary tail of the breast, and it has a characteristic appearance, as is seen in the images presented in this patient (see the figures). When this typical beaded appearance is seen, the diagnosis is usually not in question. The patient can present with a tender, palpable cord in her upper outer quadrant. There can be skin dimpling along the cord, caused by retraction of the thrombosed vein. This condition can be associated with trauma, including surgery and needle biopsy, or with dehydration, but it can also be idiopathic. Because it is rarely associated with ipsilateral breast cancer, care should be taken to examine the mammogram, and the patient, for any sign of concomitant malignancy.
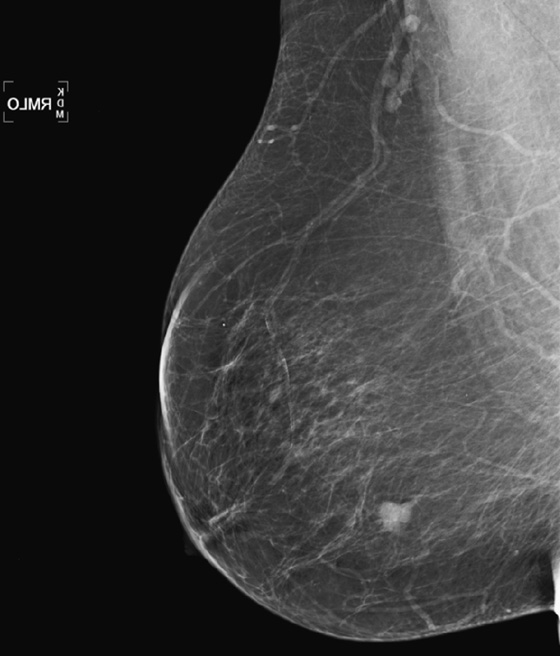
Ultrasound is useful in the diagnosis. When the ultrasound is targeted to the patient’s palpable cord, the dilated vein, with a beaded contour, will be seen. Color flow Doppler will demonstrate the absence of flow in this thrombosed vein (see the figures). Low-level echoes of thrombus within the vein may be seen.
The condition is self-limited and resolves spontaneously or with the application of warm compresses. This is a benign condition and, in the absence of the rare associated malignancy, would be categorized as a Breast Imaging Reporting and Data System (BI-RADS) 2.
CASE 142

History: A 54-year-old woman with a personal history of Hodgkin’s disease and mantle radiation 25 years ago.
1. What is the differential diagnosis of the imaging findings on the one sagittal subtraction image on her MRI? (Choose all that apply.)
A. Newly developing invasive cancer
D. Ductal carcinoma in situ (DCIS)
2. What is your recommendation?
A. Continue routine annual screening with mammogram and MRI.
D. Perform targeted ultrasound of the area of abnormality to see if this represents a cyst.
3. What constitutes a high-risk population?
A. Women who have a personal history of breast cancer
B. Women who have greater than 20% to 25% lifetime risk of breast cancer
C. Women who are extremely anxious about breast cancer
D. Women with a personal history of cervical cancer
4. What is pretest probability in interpreting breast cancer on imaging?
A. The likelihood that a patient will survive her disease
B. The likelihood that a woman will have a routine screening mammogram
C. The likelihood that an imaging finding represents cancer in a certain population
D. The likelihood that the patient will reject advice to have a biopsy
ANSWERS
CASE 142
Screening High-Risk Women
1. A, B, C, and D
2. B
3. B
4. C
References
Berg WA. Tailored supplemental screening for breast cancer: what now and what next?. AJR Am J Roentgenol. 2009;192:390–399.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:268.
Comment
In 2007, the American Cancer Society (ACS) published guidelines for screening high-risk women. The ACS advised adding MRI as an adjunct to mammography to increase the detection of early cancer in this population. They recommended MRI in addition to mammography in women who carried a lifetime risk of at least 20% to 25%. An individual woman’s risk of breast cancer can be assessed with risk models such as the BRCAPRO, Tyrer-Cuzick, or BOADICEA models. Multiple trials of women at very high risk found that adding MRI to mammography significantly increased detection of cancer: mammography found only 36% of cancers present, whereas performing MRI in addition increased detection to nearly 93%.
Patients who are at very high risk include those who carry the BRCA1 or BRCA2 mutations; those with several first-degree relatives (mother, father, sister, brother, daughter, son) with breast cancer, particularly diagnosed at a young age; those who were treated with mantle radiation between the ages of 18 and 30 years, with the incidence of breast cancer beginning 8 years after treatment; and those who have Li-Fraumeni or Cowden’s syndrome.
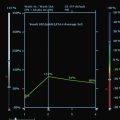
The presence of increased risk factors affects the pretest probability of the lesion, which is the probability that cancer is present in a certain population before the results of the biopsy are known. In this case, the lesion was tiny (see the figure), and morphology and enhancement characteristics were not particularly worrisome. However, the patient’s high-risk status (prior mantle radiation) changes the likelihood that a new mass, however benign in appearance, is malignant. Thus, rather than 6-month follow-up, a biopsy was recommended. The MR-guided biopsy result was DCIS, nuclear grade III.
CASE 143
History: An asymptomatic 60-year-old woman presents for routine screening mammogram.
1. What is the differential diagnosis in this patient with asymmetric breast size? (Choose all that apply.)
A. The breast bud was removed when the patient was a child.
B. This is a normal variant, with one breast smaller than the other.
C. Poor technique was applied, with one breast poorly positioned.
D. Poland’s syndrome should be considered.
2. What is the clinical significance of asymmetric breast size?
B. It is not significant if it is long standing and the patient is asymptomatic.
C. The larger breast is typically the normal breast.
D. The smaller breast is typically the normal breast.
3. If this is a baseline mammogram, and you have no clinical history of palpable mass, what is the next best step?
A. Obtain a history from the patient regarding her experience with breast size asymmetry.
C. Recommend short-interval follow-up.
D. Recommend surgical consultation.
4. What is Poland’s syndrome?
A. It is breast hypoplasia in women from Poland.
B. Only affecting women, it usually includes hypoplasia of pectoral muscle.
C. It is a relatively common congenital defect of known origin.
D. It is a rare congenital abnormality affecting the chest and arm on one side.
ANSWERS
CASE 143
Asymmetric Size of Breasts
1. B, C, and D
2. B
3. A
4. D
References
Samuels TH. Poland’s syndrome: a mammographic presentation. AJR Am J Roentgenol. 1996;166:347–348.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:408.
Comment
Breast asymmetry is usually considered a benign condition, although several features must be established to consider it benign. The condition should be of long standing. The patient herself is usually the best source for this information. The mammogram should be normal, with no evidence of developing mass or developing asymmetric tissue. If there are no prior mammograms for review, and one breast is denser or has skin thickening, further evaluation with ultrasound, physical exam, and perhaps MRI is indicated. The possibility of invasive lobular cancer, infection, or diffuse involvement of the breast with lymphoma must be considered.
History of prior breast cancer, with lumpectomy and radiation therapy, would cause a decrease in the size of the affected breast, so that history must be obtained. Benign surgery, particularly of a large volume of tissue, would cause breast asymmetry. The asymmetry can occur after pregnancy and breast-feeding, with one breast decreasing in size after pregnancy and lactation and the other breast failing to do so.
There are inherited conditions in which one breast may be smaller. One such condition is Poland’s syndrome, which also may include unilateral absence of the pectoralis muscle. There may also be arm abnormalities on the ipsilateral side, as well as rib anomalies. There is also developmental hypomastia, which is not associated with other anomalies or syndromes.
This patient did not have any other anomalies, and the asymmetry was of long standing, possibly related to size change after lactation.
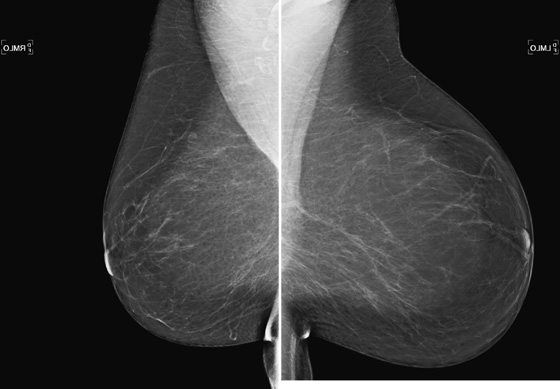
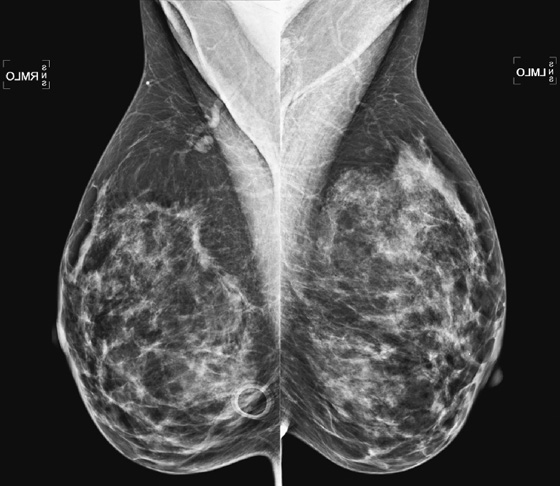
One author has published a series showing an increase in breast cancer in patients who have asymmetric breast size. However, in the absence of other mammographic findings, additional evaluation is not needed. Typically, if the asymmetry is stable and there is no mammographic abnormality (as in the figure), then this condition is given a Breast Imaging Reporting and Data System (BI-RADS) score of 1, and routine mammography is recommended.
CASE 144
History: A 48-year-old asymptomatic woman presents for a routine mammogram.
1. What should be included in the differential diagnosis for this mammogram? (Choose all that apply.)
B. Removal of left breast bud when the patient was a child
C. Left breast that was badly burned in adulthood
2. What injury can cause this condition?
A. Biopsy of the rudimentary nipple-areolar complex
B. Radiation to the breast in adulthood
C. Motor vehicle accident with seat belt trauma in a teen
D. Reduction mammoplasty in a young adult
3. What is premature thelarche?
A. Development of breast tissue before puberty
B. Onset of menstruation earlier than age 8
C. Presence of accessory nipples
4. What BI-RADS (Breast Imaging Reporting and Data System) score would you give this case if you had no prior films for comparison?
A. BI-RADS 0—need additional evaluation
B. BI-RADS 4—suspicious, recommend biopsy
C. BI-RADS 3—probably benign, recommend short-interval follow-up
ANSWERS
CASE 144
Breast Bud Removed
1. B and D
2. A
3. A
4. D
References
Bland KI. Copeland EM. In: The Breast. 2nd ed Philadelphia: Saunders; 1998:214.
Chautard EA, Freire-Maia N. Poland’s syndrome. Br Med J. 1971;4(5790):812.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:150.
Comment
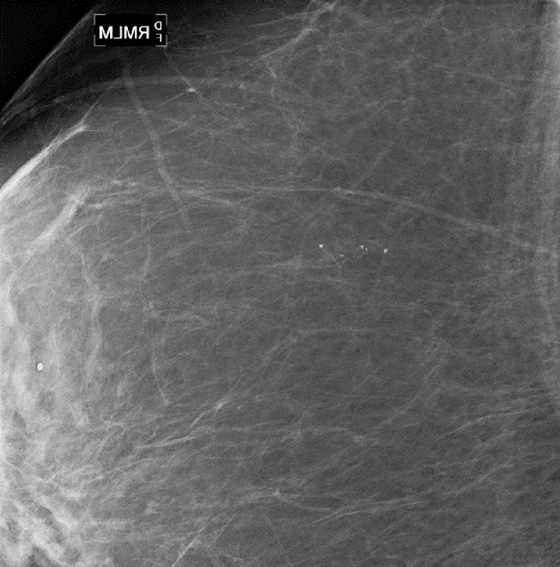
The patient in this case had surgery as a young child for a congenital heart abnormality. The incision was made at the fourth intercostal interspace and interrupted the anlage for the ipsilateral breast (the breast bud). This iatrogenic injury to the breast resulted in removal of the breast bud and in failure of development of the normal ducts and lobules of that breast. The contralateral breast developed normally (see the figure).
Premature thelarche is the enlargement of the breasts before sexual maturation and is usually seen at age 6 months to 2 years. The enlargement can be unilateral, and the prematurely enlarging breast can be removed because of suspicion for malignancy (although the actual chance of this is vanishingly small) or abscess. When the breast bud is removed, the breast fails to develop. Radiation to the chest may cause the same result.
If the pectoralis muscle is also missing or there are other anomalies of the chest or ipsilateral arm, a congenital syndrome may be present. Poland’s syndrome is the most well-known congenital syndrome; patients present with variable features that are always unilateral and can include absence of the pectoralis muscles, absence of breasts, rib anomalies, and brachysyndactyly.
CASE 145

History: An 80-year-old patient has a new mass on mammogram.
1. What is the differential diagnosis for this mammogram? (Choose all that apply.)
2. What is the next stage of the work-up?
A. Spot compression views and ultrasound
B. No work-up needed for this benign-appearing mass
3. What is a complicated cyst on ultrasound?
A. A cyst that has been aspirated
B. A cyst that contains debris but has a thin wall
D. A cyst that recurs after aspiration
4. What is a complex cyst on ultrasound?
A. A cyst that contains internal echoes, thick septations, or a mass
D. A cyst with low-level internal echoes
ANSWERS
CASE 145
Complex Cyst
1. A, B, and C
2. A
3. B
4. A
References
Berg WA Campassi. CI. Ioffe OB: Cystic lesions of the breast: sonographic-pathologic correlation. Radiology. 2003;227(1):183–191.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:159.
Comment
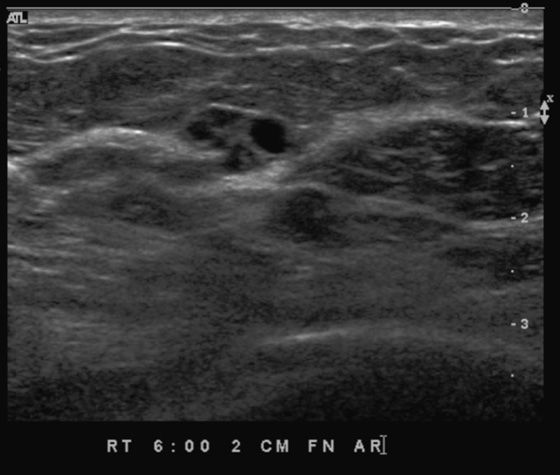
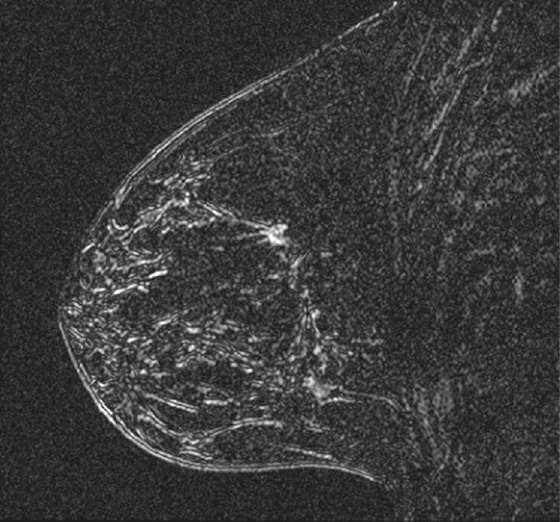
A new mass is detected in the lower right breast in an 80-year-old, asymptomatic patient. On mammogram, the mass does not have completely smooth borders (see the figures). To further evaluate this new finding, the patient must be recalled for an additional view (spot compression) and ultrasound. Any new mammographic finding in the elderly must be viewed with suspicion because the malignancy rate is high, and typically the elderly breast is quiescent, not forming new benign masses or cysts, as is common in younger patients.
The ultrasound image is shown. Spot compression views in this patient are not shown, but the mass looked essentially unchanged from the standard images. The ultrasound exam demonstrates a mass that has anechoic areas, as well as thick septations. It is consistent with a complex cyst. Although most complex cysts are benign, there is a higher risk of malignancy in the complex cyst. Suspicious features must be sought, and the cyst must be judged by the most suspicious feature seen. Suspicious features include thick internal septations, mural nodules, fibrovascular stalk, and microlobulated margins. If any of these is seen, biopsy is indicated. Color flow Doppler is useful in determining the presence of blood flow within the cyst, either within the stalk, in the septations, or in the intracystic nodule. When blood flow is seen within the complex cyst, biopsy is indicated.
In two series, complex cysts with these features were malignant 23% to 31% of the time. In the majority of cases, these complex cysts are fibrocystic change, intraductal or intracystic papilloma, or atypical hyperplasia, either ductal or lobular. When malignant, the complex cyst can be ductal carcinoma in situ (DCIS) or infiltrating cancer, either ductal or lobular.
The last figure shows another complex cyst in a different patient, also malignant on needle biopsy.
CASE 146
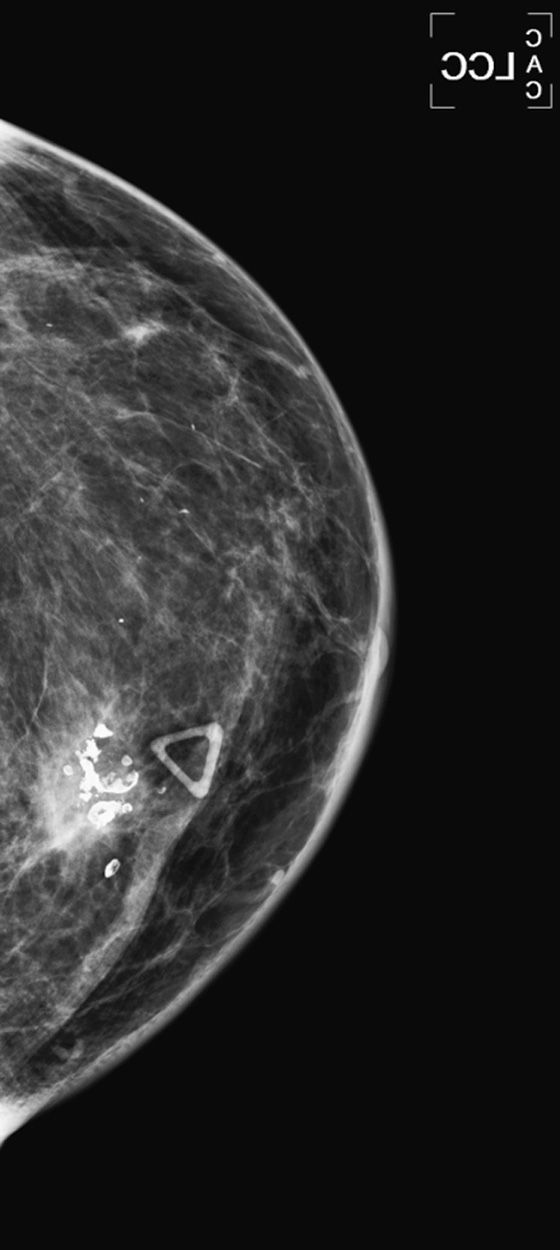
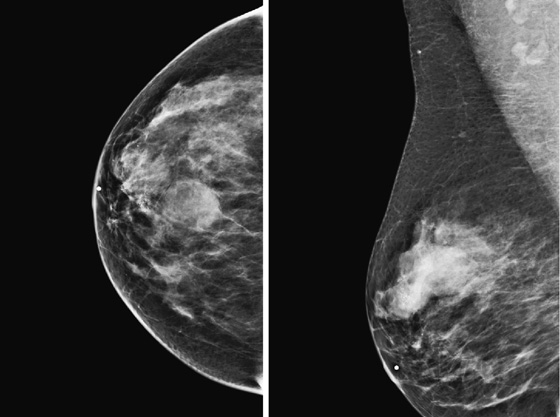
History: A 59-year-old woman presents with a palpable concern in her medial left breast. She had a benign excisional surgical biopsy 5 years ago. Left craniocaudal (CC) views from the current exam, as well as from 3 years ago and 2 years ago, are shown.
1. What is the differential diagnosis of the palpable finding on the current left CC view? (Choose all that apply.)
D. Ductal carcinoma in situ (DCIS)
2. Is this mammographic appearance consistent with fat necrosis?
A. No, fat necrosis does not appear as a spiculated mass.
B. No, fat necrosis must have an oil cyst with rim calcifications.
C. Yes, this is consistent with fibrosis increasing at an area of fat necrosis.
D. No, fat necrosis effect decreases with time.
3. What is the next step in evaluation?
A. A 6-month follow-up mammogram
B. Image-guided needle core biopsy
D. A return in 1 month to see if findings are related to trauma
4. If needle core biopsy is done, and histology is fat necrosis, what is the management?
A. This appearance is nonconcordant with that histology, and surgery must be performed.
B. This appearance is concordant with that histology, and the lesion can be followed.
C. This is nonconcordant with fat necrosis appearance; recommend repeat image-guided biopsy.
D. Histology is concordant, but the patient must have surgery to remove the lesion.
ANSWERS
CASE 146
Fat Necrosis in an Unusual Presentation
1. A, B, and D
2. C
3. B
4. B
Reference
Taboada JL, Stephens TW, Krishnamurthy S, et al. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192:815–825.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:109.
Comment
A 59-year-old woman presents with a palpable mass. She had a benign excisional biopsy of the breast 5 years ago. The work-up starts with a mammogram (the first figure shows a single view from this exam) demonstrating a spiculated mass in the medial right breast, corresponding to the palpable concern. When the mammogram is compared with the woman’s previous mammograms, the spiculated mass has developed (see the figures). The work-up may then continue with an ultrasound exam to further evaluate the palpable and imaging abnormality (not shown). In this case, the mass was hypoechoic, with irregular margins and shadowing on ultrasound. The mammographic, ultrasound, and clinical findings are all consistent with malignancy. However, on review of the prior mammograms, elements of fat necrosis are seen, with fat lucency and rim calcifications, which coarsen in the interval between the two prior exams. The spiculated mass develops in the area of fat necrosis.
Fat necrosis has many appearances, depending on the histologic features of the injury. Fat cells (adipocytes) degenerate, forming a pocket of fat or oil (oil cyst). This is associated with hemorrhage, and degenerated red blood cells conglomerate in the area of necrotic adipocytes. Histiocytes and multinucleated giant cells infiltrate. Hemosiderin is deposited, and fibrosis develops. Varying degrees of these elements are seen in the individual area of fat necrosis. When an oil cyst is present on mammogram with rim-type calcifications, the appearance is pathognomonic for fat necrosis. However, when fibrosis develops or predominates, the spiculated appearance of fibrosis overlaps with the appearance of malignancy, and biopsy is needed.
Because needle core biopsy is a sampling procedure, sampling can be incomplete. If the diagnosis is a specific benign histology, such as fat necrosis in an area where fat necrosis was previously seen, as in this case, you may place the patient into a short-interval follow-up category, Breast Imaging Reporting and Data System (BI-RADS) 3. You may also seek a surgical opinion, although surgical excision is not mandatory. This patient consulted with her surgeon, who elected to follow. No excision was performed.
CASE 147


History: A 25-year-old woman has a palpable lump in the inferior left breast, which she reports has increased in size in the last 6 months.
1. What is the differential diagnosis, based on the ultrasound images presented? (Choose all that apply.)
C. Infiltrating ductal or lobular carcinoma
2. What are the ultrasound features of this mass that suggest benign etiology?
A. Angular margins, parallel alignment
B. Hypoechoic, oval, smooth margins
C. Angular margins, abrupt interface
D. Parallel alignment, oval shape, abrupt interface with surrounding tissue
3. What are the ultrasound features of this mass that suggest malignancy?
A. Angular margins, some posterior shadowing
B. Vertical alignment, angular margins
C. Angular margins, thick echogenic halo
D. Oval shape, smooth margins, abrupt interface
4. Needle core biopsy yields histology of fibroadenoma. What is the next step?
A. Result is concordant, follow in 1 year.
B. Result is concordant, ask patient to monitor growth of mass and return if it increases in size.
C. Result is concordant, recommend surgery because of young age.
D. Result is noncorcordant, recommend surgical consultation.
ANSWERS
CASE 147
Nonconcordant Biopsy
1. B and C
2. D
3. A
4. D
References
Mendelson EB, Baum JK, Berg WA, et al: BI-RADS: Ultrasound. In: D’Orsi CJ, Mendelson EB, Ikeda DM, et al: Breast Imaging Reporting and Data System: ACR BI-RADS—Breast Imaging Atlas, Reston, VA: American College of Radiology, 2003
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:163. 229
Comment
The ultrasound images of this young woman with a rapidly enlarging mass show a hypoechoic mass with irregular margins and an abrupt interface with the surrounding tissue. The mass is parallel to the skin surface (see the figures). The images shown are taken in radial and antiradial orientation, which is important in documenting the lesion.
There is an American College of Radiology (ACR) lexicon for the description of ultrasound findings, which includes descriptors for masses. It is helpful to use the language of the lexicon to aid communication to the referring physician and between imaging centers. Mass descriptors should include shape (oval, round, or irregular), mass orientation (parallel or vertical), mass margin (circumscribed or not circumscribed), lesion boundary (abrupt or echogenic halo), internal echogenicity, and posterior acoustic features (shadowing or enhancement).
This mass is oval and is parallel to the skin, with an abrupt interface. These features are consistent with benign mass. However, the margins are not circumscribed. When margins are not circumscribed, they can be defined as microlobulated, indistinct, angular, or spiculated (increasing level of suspicion). This mass has microlobulated and angular margins. The decision to biopsy and the Breast Imaging Reporting and Data System (BI-RADS) code given to the mass should be based on the most suspicious feature, so this should be assigned a BI-RADS 4. Core biopsy was performed with a 10-gauge, vacuum-assisted biopsy device, and histology was fibroadenoma.
The biopsy result is felt to be nonconcordant with the imaging findings. When this occurs, further action is needed. The patient should be referred to a surgeon for consideration of excising the mass. This mass was excised, and the histology on excisional biopsy was fibroadenoma.
CASE 148
History: A 51-year-old woman presents with a complaint of dimpling in her right upper outer breast. Mammogram, ultrasound, and ultrasound-guided needle core biopsy are performed.
1. What should be included in the differential diagnosis based on the mammogram? (Choose all that apply.)
A. Architectural distortion from prior surgery in the right breast
B. Architectural distortion caused by malignant mass in the right breast
C. Radial scar in the right breast
D. Suspicious microcalcifications in the right upper outer breast
2. The tissue diagnosis of the right upper outer breast mass is invasive lobular carcinoma (ILC). What is the next best imaging examination?
C. MRI of the ipsilateral breast only
D. MRI of the contralateral breast only
3. What is the one best diagnosis based on the MRI examination of the left breast?
B. Pseudoangiomatous stromal hyperplasia (PASH)
4. What is the next step in management of the left breast?
A. The patient should be encouraged to undergo bilateral mastectomy.
ANSWERS
CASE 148
Contralateral Breast Screening with MRI
1. A, B, and C
2. B
3. A
4. D
References
Dedes KJ, Fink D. Clinical presentation and surgical management of invasive lobular carcinoma of the breast. Breast Dis. 2009;30:31–37.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:265. 104
Comment
This 51-year-old woman noted dimpling in her right breast and underwent mammography and ultrasound. Subsequent biopsy of the mass, seen best on ultrasound, showed ILC. MRI was recommended to establish the extent of disease in this woman with heterogeneously dense breast tissue.
ILC has a variable appearance on imaging, including mammography, ultrasound, and MRI. On mammography, ILC may appear as a noncalcified mass, with ill-defined or spiculated margins. Because its growth pattern is infiltrative, a focal mass may not be present at all. This carcinoma may cause only distortion, may be completely occult, or may be seen only on one view. ILC accounts for less than 10% of all breast cancers but is more commonly associated with bilateral disease and multicentric and multifocal disease (additional malignancy in the same breast) than is the more common invasive ductal carcinoma. In the ACRIN trial of MRI of the contralateral breast in women with breast cancer, occult contralateral cancer was identified in 6% of women with ILC versus 3% of women with invasive ductal carcinoma.
In this patient, MRI showed only one mass in the ipsilateral breast. In the contralateral breast, clumped enhancement was seen to extend posteriorly in a segmental distribution. No mammographic calcifications are present in this location. MRI-guided biopsy of two sites in the left breast yielded a diagnosis of ductal carcinoma in situ in both sites; this represents occult breast cancer in the contralateral breast, not suspected clinically or mammographically.
The mammographic sensitivity for detecting ILC is reported to be 34% to 81%, inversely related to breast density. MRI is reportedly 93% to 96% sensitive for the detection of ILC. Women with a diagnosis of ILC and dense breasts should consider undergoing bilateral breast MRI.
CASE 149


History: A 64-year-old woman whose left breast cancer was diagnosed in 2002 developed radiation-induced angiosarcoma of the left breast in 2009 and underwent left mastectomy. She now presents for routine annual evaluation of the remaining right breast.
1. What should be included in the differential diagnosis of the right mediolateral oblique view presented? (Choose all that apply.)
A. Enlarged right axillary node, suspicious for metastatic breast cancer
B. Enlarged right axillary node, possible metastatic angiosarcoma
C. Sebaceous cyst in the right axilla
D. Enlarged right axillary node, most likely lymphoma
2. What is RIS?
A. Sarcoma that occurs immediately after the treatment of the breast with external beam radiation
B. Sarcoma related to the type of breast cancer, more common in invasive lobular carcinoma
C. Sarcoma that develops in the radiation field years after treatment
D. An indolent process that is a complication of radiation therapy
3. What is the prognosis for RIS after treatment for breast cancer?
A. The prognosis is good because RIS is not as aggressive as typical sarcoma.
B. The prognosis is poor because it is usually detected late.
D. The prognosis is very good because this is a routine complication of radiation therapy.
4. What imaging modality should be used to follow patients with breast cancer to detect RIS?
A. All patients treated with radiation should have annual MRI.
B. All patients treated with radiation should have annual mammograms, supplemented with ultrasound.
C. All patients treated with mastectomy and radiation should have annual bilateral mammograms.
D. All patients treated with breast conservation therapy should have annual bilateral mammograms.
ANSWERS
CASE 149
Radiation-Induced Sarcoma
1. A and B
2. C
3. B
4. D
References
Blanchard DK, Reynolds C, Grant CS, et al. Radiation-induced breast sarcoma. Am J Surg. 2002;184(4):356–358.
Cross-Reference
Ikeda D: Breast Imaging: THE REQUISITES, 2nd ed, Philadelphia: Saunders, 2010, p 398
Comment
Radiation-induced sarcoma (RIS) is a disease that develops in the radiated field 3 to 20 years after treatment. The incidence is related to the dose, with most reported cases occurring after a dose of 60 to 80 Gy. It is relatively rare, occurring in 0.07% of patients treated with radiation therapy for breast cancer 5 years after treatment in one large series. The incidence increases with time following therapy, with 0.048% risk after 15 years. RIS carries a poor prognosis, with 5-year survival rate of 36% in the aforementioned series.
Late detection is believed to be one reason for the poor prognosis. Although in one series most RIS developed in the breast, the lesions also were found in the chest wall, sternum, above the clavicle, in the scapula, and in the axilla, where they may go undetected.
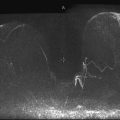
The patient in the present case was diagnosed with RIS when she felt a lump in her treated breast 7 years after lumpectomy and radiation treatment for left breast cancer. The mass was surgically excised and revealed a high-grade angiosarcoma. She underwent mastectomy, and she presented 1 year later for routine evaluation of the contralateral breast. An enlarged node was seen in the right axilla (see the figures). Ultrasound was performed (see the figures) to guide biopsy. Increased blood flow within the node was noted on ultrasound (see the figures). Biopsy pathology was metastatic high-grade angiosarcoma.
CASE 150

History: A 49-year-old woman who has a family history of breast cancer in her mother, diagnosed at age 52, presents with a palpable mass in the right upper breast.
1. What should be included in the differential diagnosis, based on the mammographic and ultrasound images shown? (Choose all that apply.)
B. Ductal carcinoma in situ (DCIS) adjacent to a cyst
C. Mucinous carcinoma, with adjacent DCIS
D. Fibrocystic change, with benign calcifications and a cyst
2. After standard mammogram views and ultrasound, what additional imaging may help?
A. Magnification views to evaluate the calcifications further
B. Rolled craniocaudal views to evaluate the round mass better
C. True lateral mediolateral view
D. Spot compression view of the calcifications
3. Biopsy is indicated. How would you approach the biopsy?
A. Stereotactic biopsy of the calcifications
B. Ultrasound-guided core biopsy of the round mass
C. MRI-guided biopsy of the mass
D. Ultrasound-guided biopsy of the calcifications
4. What is the role of MRI in this patient?
A. To evaluate the calcifications further before biopsy
B. To evaluate for enhancement in the round mass
C. To evaluate for extent of disease after malignant diagnosis is established by needle biopsy
D. To evaluate only the right breast, for evidence of additional disease
ANSWERS
CASE 150
Cancer Adjacent to Palpable Cyst
1. B and C
2. A
3. A
4. C
Reference
Venkatesan A, Chu P, Kerlikowske K, et al. Positive predictive value of specific mammographic findings according to reader and patient variables. Radiology. 2009;250(3):648–657.
Cross-Reference
Ikeda D. Breast Imaging. In: THE REQUISITES. 2nd ed Philadelphia: Saunders; 2010:85. 95, 100, 271
Comment
This case shows numerous important points in the diagnostic work-up of a palpable finding, as follows:
▪ It is essential to establish concordance between the palpable finding and the imaging finding.
▪ Clinical breast examination is important, and palpable findings should not be ignored.
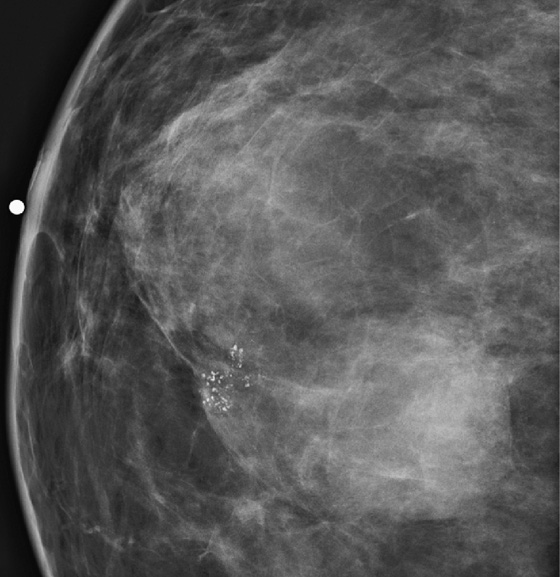
This 49-year-old woman has a family history of cancer in her mother at age 52. Clinical or mammographic findings should be viewed with suspicion because of this family history. Mammography (see the figures) shows a mass and adjacent clustered calcifications; this is suspicious for a round invasive malignancy with adjacent DCIS. Ultrasound and magnification views (see the figures) fail to clarify the mass as a simple cyst. The calcifications are pleomorphic and tightly clustered.
Biopsy was performed with stereotactic guidance and showed in situ and invasive ductal carcinoma, grade II.