Procedure 14 Distal Anterior Interosseous Nerve Transfer to Motor Branch of Ulnar Nerve
![]() See Video 12: Distal Anterior Interosseous Nerve Transfer to Motor Branch of Ulnar Nerve
See Video 12: Distal Anterior Interosseous Nerve Transfer to Motor Branch of Ulnar Nerve
Indications
 For recovery of intrinsic muscle function in a patient with a high ulnar nerve injury (near or above the elbow) to shorten the distance between the donor nerve and the recipient muscles
For recovery of intrinsic muscle function in a patient with a high ulnar nerve injury (near or above the elbow) to shorten the distance between the donor nerve and the recipient muscles
Examination/Imaging
Clinical Examination
 Check motor function of the anterior interosseous nerve (AIN).
Check motor function of the anterior interosseous nerve (AIN).
 Check the joints of the ring and small fingers. The joints of the hand should be supple. If mild contractures of the joints are discovered, the patient will require hand therapy before any nerve transfer procedures are performed.
Check the joints of the ring and small fingers. The joints of the hand should be supple. If mild contractures of the joints are discovered, the patient will require hand therapy before any nerve transfer procedures are performed.
Surgical Anatomy
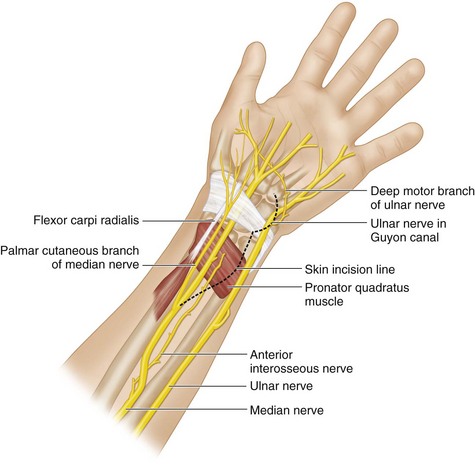
 The ulnar nerve enters the anterior (flexor) compartment of the forearm between the two heads of flexor carpi ulnaris (FCU) and innervates one and a half muscles (FCU and medial half of FDP to the ring and small fingers). It runs along the ulna with the ulnar artery, and the two travel distally under the FCU. Proximal to the wrist, the fascicles of the motor branch lie ulnar to the sensory fascicles. The ulnar nerve and artery pass superficial to the flexor retinaculum into the Guyon canal. In the Guyon canal, the ulnar artery is radial to the ulnar nerve. At the radial side of the pisiform bone, the ulnar nerve is divided into the superficial and deep branches. The deep branch of the ulnar nerve curves laterally to supply the hypothenar muscles and runs across the palm with the deep palmar arch; it terminates by supplying the first dorsal interosseous and the deep head of the flexor pollicis brevis (Fig. 14-1).
The ulnar nerve enters the anterior (flexor) compartment of the forearm between the two heads of flexor carpi ulnaris (FCU) and innervates one and a half muscles (FCU and medial half of FDP to the ring and small fingers). It runs along the ulna with the ulnar artery, and the two travel distally under the FCU. Proximal to the wrist, the fascicles of the motor branch lie ulnar to the sensory fascicles. The ulnar nerve and artery pass superficial to the flexor retinaculum into the Guyon canal. In the Guyon canal, the ulnar artery is radial to the ulnar nerve. At the radial side of the pisiform bone, the ulnar nerve is divided into the superficial and deep branches. The deep branch of the ulnar nerve curves laterally to supply the hypothenar muscles and runs across the palm with the deep palmar arch; it terminates by supplying the first dorsal interosseous and the deep head of the flexor pollicis brevis (Fig. 14-1).
 The AIN is a branch of the median nerve that supplies the deep muscles on the front of the forearm. It accompanies the anterior interosseous artery and runs on the anterior surface of the interosseous membrane in the interval between the FPL and FDP, supplying the whole of the former and the radial half of the latter. The AIN terminates in the volar capsule of the wrist joint after it innervates the PQ (see Fig. 14-1).
The AIN is a branch of the median nerve that supplies the deep muscles on the front of the forearm. It accompanies the anterior interosseous artery and runs on the anterior surface of the interosseous membrane in the interval between the FPL and FDP, supplying the whole of the former and the radial half of the latter. The AIN terminates in the volar capsule of the wrist joint after it innervates the PQ (see Fig. 14-1).
Exposures
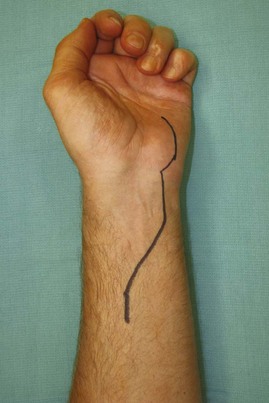
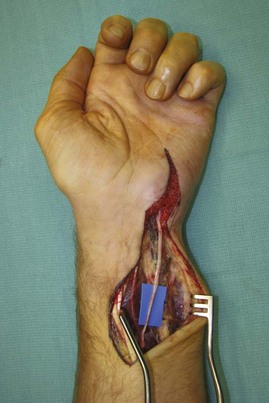
 A 10-cm curvilinear incision begins at the pisiform and curves gently radially and proximally. This incision will expose the ulnar nerve in Guyon canal and the AIN in the distal forearm (Fig. 14-2). The skin and subcutaneous fat are dissected in the distal half of the incision to expose the ulnar nerve in Guyon canal. In the proximal half of the incision, the antebrachial fascia is divided ulnar to the palmaris longus. The median nerve is identified below the palmaris longus to expose the flexor tendons. The palmaris longus, median nerve, and flexor tendons to the radial two fingers are retracted radially, and the flexor tendons to the ulnar fingers are retracted ulnarly to expose the PQ.
A 10-cm curvilinear incision begins at the pisiform and curves gently radially and proximally. This incision will expose the ulnar nerve in Guyon canal and the AIN in the distal forearm (Fig. 14-2). The skin and subcutaneous fat are dissected in the distal half of the incision to expose the ulnar nerve in Guyon canal. In the proximal half of the incision, the antebrachial fascia is divided ulnar to the palmaris longus. The median nerve is identified below the palmaris longus to expose the flexor tendons. The palmaris longus, median nerve, and flexor tendons to the radial two fingers are retracted radially, and the flexor tendons to the ulnar fingers are retracted ulnarly to expose the PQ.
Procedure
Step 1
Step 2
 The motor branch of the ulnar nerve in the hand is dissected proximally into the forearm for about 10 cm from the hook of the hamate (Fig. 14-4) to a point that is proximal to the AIN (Fig. 14-5).
The motor branch of the ulnar nerve in the hand is dissected proximally into the forearm for about 10 cm from the hook of the hamate (Fig. 14-4) to a point that is proximal to the AIN (Fig. 14-5).
Step 3
 The AIN is identified proximal to the PQ. This is confirmed using a nerve stimulator and should show marked contraction of the PQ. Intramuscular dissection of the AIN within the PQ is performed.
The AIN is identified proximal to the PQ. This is confirmed using a nerve stimulator and should show marked contraction of the PQ. Intramuscular dissection of the AIN within the PQ is performed.
 At about the midportion of the PQ, the AIN begins to branch. The AIN is divided proximal to this branching point.
At about the midportion of the PQ, the AIN begins to branch. The AIN is divided proximal to this branching point.
Step 4
 The motor branch of the ulnar nerve is divided in the forearm using micro-scissors and passed under the flexor tendons to reach the divided AIN within the PQ (Fig. 14-6).
The motor branch of the ulnar nerve is divided in the forearm using micro-scissors and passed under the flexor tendons to reach the divided AIN within the PQ (Fig. 14-6).
Step 4 Pearls
The motor branch of the ulnar nerve is divided at an adequate distance proximally so that a nerve graft is not necessary to reach the distal end of the AIN. The use of nerve graft will markedly decrease the axon count reaching the muscles and hamper muscle recovery.
The motor branch of the ulnar nerve should be passed underneath the flexor tendons to keep it on the same plane as the AIN to avoid compression of nerve while the flexor tendons glide during movement.
Step 5
 Direct epineural repair of the motor branch of the ulnar nerve to the PQ branch of the AIN in end-to-end fashion is achieved using 9-0 nylon sutures under microscope magnification (Fig. 14-7).
Direct epineural repair of the motor branch of the ulnar nerve to the PQ branch of the AIN in end-to-end fashion is achieved using 9-0 nylon sutures under microscope magnification (Fig. 14-7).
 The wrist and digits are taken through a full range of motion to make sure that there is no tension at the nerve repair site.
The wrist and digits are taken through a full range of motion to make sure that there is no tension at the nerve repair site.
Postoperative Care and Expected Outcomes
 A splint is used to maintain the wrist in neutral position for 3 weeks. The patient is instructed in range-of-motion exercise of the fingers, elbow, and shoulder to maintain movement and nerve gliding proximal and distal to the repair site.
A splint is used to maintain the wrist in neutral position for 3 weeks. The patient is instructed in range-of-motion exercise of the fingers, elbow, and shoulder to maintain movement and nerve gliding proximal and distal to the repair site.
 Postoperative rehabilitation includes motor rehabilitation. The patient is initially instructed in resisted forearm pronation exercises. With evidence of reinnervation of the intrinsic muscles, the patient is then instructed in pinching exercises in resisted forearm pronated positions.
Postoperative rehabilitation includes motor rehabilitation. The patient is initially instructed in resisted forearm pronation exercises. With evidence of reinnervation of the intrinsic muscles, the patient is then instructed in pinching exercises in resisted forearm pronated positions.
 Although the distal anterior interosseous nerve is not a powerful donor, one can at least expect to prevent clawing, improve pinch strength, and avoid tendon transfers.
Although the distal anterior interosseous nerve is not a powerful donor, one can at least expect to prevent clawing, improve pinch strength, and avoid tendon transfers.
Haase SC, Chung KC. Anterior interosseous nerve transfer to the motor branch of the ulnar nerve for high ulnar nerve injuries. Ann Plast Surg. 2002;49:285-290.
Novak CB, Mackinnon SE. Distal anterior interosseous nerve transfer to the deep motor branch of the ulnar nerve for reconstruction of high ulnar nerve injuries. J Reconstruct Microsurg. 2002;18:459-463.