Antineoplastic Medications
Objectives
1. List the types of drugs used to treat neoplastic disease or cancer.
2. Identify the major adverse reactions associated with antineoplastic agents.
3. Develop a teaching plan for a patient taking an antineoplastic drug.
Key Terms
alkylating agents (ĂL-k-lā-tĭng, p. 201)
antibiotic preparations (ăn-tĭ-bī-ŎT-ĭk, p. 201)
antimetabolites (ăn-tĭ-mě-TĂB-ō-līts, p. 201)
Biologic Response Modifiers (BĪ-ō-LŎJ-ĭk, p. 202)
chemotherapeutic agents (kē-mō-thěr-ă-PŪ-tĭk, p. 200)
male or female hormones (HŎR-mōnz, p. 201)
malignancy (mă-LĬG-năn-sē, p. 200)
metastasis (mă-TĂS-tă-sĭs, p. 200)
mitotic inhibitors (mī-TŎT-ĭkĭn-HĬB-ĭ-tŏrs, p. 202)
neoplasms (NĒ-ō-plăz mz, p. 200)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
Licensed practical and vocation nurses (LPNs/LVNs) often do not play a direct role in giving medications for cancer. There are many types of cancer and patients who have cancer are very commonly seen in areas in which LPNs/LVNs work. Every nurse should have some familiarity with the most common drugs given to fight cancer and a general awareness of why they might be ordered. Nurses are also frequently involved in administering other drugs to the cancer patient to fight the side effects of the very toxic cancer drugs.
Most cells in the body grow slowly at a rate that can be predicted. When cell growth becomes rapid and uncontrolled, neoplasms (abnormal growths or tumors that may be benign or malignant) may be found. These cells often have the ability to travel throughout the body, spreading this unusually rapid cell growth into other areas (metastasis). Cancer cells rob other tissues of the nutrients (substances that support life and growth) required for normal health. We call this out-of-control cell growth malignancy or cancerous growth. The causes of cancer are many—chemical, physical, hereditary, or biological. Some types of cancer are increased by patient behavior or lifestyle, such as lung cancer caused by smoking. Thus risk for developing some types of cancer may be reduced by changing eating habits, exercise, exposure to sun, or other types of behavior.
Antineoplastic agents, also called chemotherapeutic agents, are used to treat cancerous or malignant diseases. They slow cell growth or delay the spread of the malignant cells into other parts of the body. To achieve a cure, every malignant cell must be removed, destroyed, or crippled. Antineoplastic (anticancer) agents are most often used with other forms of treatment such as surgery and radiation. Drug therapy is rigorous, often requiring multiple drugs, intensive courses of high doses, and repeated courses of medicine if they are to be effective.
The following types of medications are used to treat neoplastic diseases: alkylating agents, antibiotic preparations, antimetabolites, hormones, natural products, and biologic response modifiers.
The types and sites of malignancies vary, and some agents are more effective than others in treating certain types of malignancies. The ideal antineoplastic agent damages the malignant cells of the patient while keeping the normal cells as healthy as possible.
Normal cells in the body do not all grow at the same rate. The cells in the gastrointestinal (GI) tract, bone marrow, hair follicles, lymph tissue, mouth, and testes or ovaries are rapidly dividing and growing. Antineoplastic drugs affect rapidly growing tumor cells, but also affect all other rapidly growing normal cells, thus producing many of the adverse reactions caused by these drugs (diarrhea, alopecia [hair loss], infertility, and the like).
There are many new, highly toxic products on the market in cancer treatment, including interferon, mitotane, and asparaginase. Antineoplastic drugs are strong and may be toxic; they are only ordered by a cancer or oncology specialist. Many drugs require intravenous (IV) administration. Even small dosage errors could have significant negative effects on the patient. Adverse reactions are common with this group of medications, and patients must be watched carefully for the development of toxicities. Hospitals may vary in whether they allow LPNs/LVNs to administer these drugs, so it is important to know institutional policy and stay within the authorized scope of practice.
Safety is a particular issue with oncology drugs. They are already toxic products and any errors in medication selected, dosage, or administration may be overwhelming to an ill patient.
Action and Uses
The five major types of antineoplastic agents may be used in combination or alone. There are often specific research protocols or rules that govern the use of these medications. It is important for the nurse to accurately report all reactions and adverse effects the patient might have so the action of the drug can be understood.
Alkylating agents are used to interfere with the normal process of cell division. They are some of the most widely used antineoplastic drugs. These drugs attach physically to deoxyribonucleic acid (DNA) in the tumor cell, a process called alkylation. As they do this, they change the structure of DNA in cancer cells and prevent it from functioning normally. There are different alkylating agents and they all attach to DNA in different ways. Working together, they are able to kill the cell or stop the production of new tumor cells. Although the alkylation occurs in the cancer cells, the killing action does not occur until the affected cell tries to divide.
This alkylating effect occurs in rapidly growing malignant cells, but it also occurs in some normal cells. Within the body, normal rapidly growing cells such as blood cells, white blood cells (WBCs) and epithelial cells lining the GI tract are also damaged. Thus as soon as the alkylating medications are given, red blood cells, WBCs, and platelets begin dying. These patients experience anemia and higher risk of infection. The death or damage to cells lining the GI tract produces nausea, vomiting, and diarrhea.
Specific antibiotic preparations are used, not for their antiinfective properties, but to delay or prevent cell division of the malignant cells. This action is caused by interference with DNA and ribonucleic acid synthesis. These antitumor antibiotics are obtained from bacteria and have the ability to kill cancer cells. These chemicals are more toxic than other antibiotics and their use is limited to use in treating very specific cancers.
Because the antitumor antibiotics interact with DNA in a way similar to the alkylating agents, their general actions and side effects are similar to those of the alkylating agents. However, all the antitumor antibiotics must be given intravenously or put directly into a cavity of the body using a catheter.
Antimetabolites disrupt normal cell functions by interfering with various metabolic functions of the cells and interrupt critical cell pathways in cells. Cells that are rapidly growing require large amounts of nutrients to build nucleic acids and proteins. These drugs resemble the essential building blocks of the cells but when the cancer cell attempts to use these chemicals as building blocks, the cancer cells slow their growth or die. This action is most effective in cells that are the most rapidly dividing—cancer cells, as well as normal hair and skin cells.
Some tumors may depend on male or female hormones, the chemicals produced by the sex glands. In patients who have these types of tumors, various hormones that counteract the effects of the hormones used by the tumors may be effective in treatment. The mechanism of action is unclear. Administering high doses of specific hormones or hormone antagonists can block the receptors in reproductive tissue tumors and slow tumor growth. An example is the use of tamoxifen to slow specific types of breast cancers that depend on estrogen for growth. Administration of the female hormone estrogen also slows the growth of prostate cancer.
In general, hormones and hormone antagonists produce few of the cytotoxic side effects seen with other antineoplastic drugs. However, as these medications may be given in high doses and for long periods, they may produce other unpleasant side effects. They rarely produce cures but may slow the growth of the cancer.
There are a variety of other primary plant extracts or alkaloids that are used as antineoplastics. These chemicals have been isolated from a number of plants, including common flowers and shrubs. Although these chemicals are structurally different, they all have the ability to stop cell division. As a group, they may be called mitotic inhibitors.
Taxoids and topoisomerase inhibitors are other groups of medications that have biologic properties helpful in treating cancer. They often have significant adverse effects.
Biologic response modifiers are relativity new immunologic drugs that do not kill tumor cells directly themselves, but instead stimulate the body’s immune system to help it fight the cancer. They may also be helpful in minimizing the toxic effects of other antineoplastics. Specifically, some drugs work to prevent anemia, stimulate platelet production, or help prevent severe thrombocytopenia. Thus the quality of life of these patients may be better when these drugs are given.
See Figure 14-1 to see where major antineoplastic drugs act on the cells.
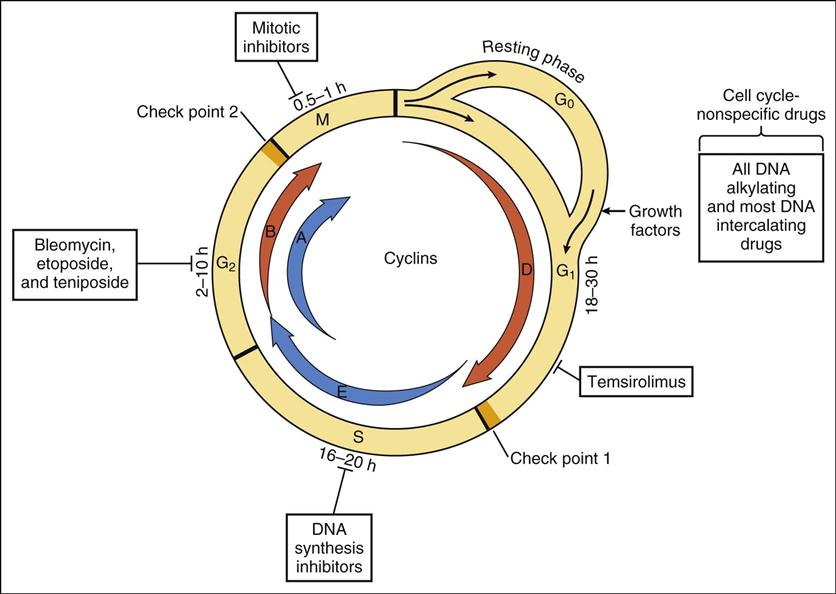
Cell division or replication proceeds in a cycle. In sequence, the cycle involves G1 (gap1), S (DNA synthesis), G2 (gap 2), and M (mitosis). Differentiated cells may enter a resting state called GO. Growth factors may stimulate resting cells to reenter the cell cycle. Proteins called cyclins (A,B,D,E) promote cell progress through the cycle. Two check points in the cycle which often malfunction in cancer cells are those which control entry into the critical phases of DNA synthesis and mitosis. Cell cycle-specific drugs act primarily during the designated phase of the cycle. Cell cycle-nonspecific drugs act throughout the cell cycle.
A mix of other drugs, most of which have been developed in the last few years, now make up the largest category of antineoplastic drugs, the miscellaneous agents. These products are used for treatment of a wide variety of conditions. Many of them have unlabeled uses, whereas, for others, clinical trials are being done to determine if they are effective and safe. Many of these drugs are being evaluated further.
Adverse Reactions
The action of the antineoplastic agents on normal cells causes many of the adverse reactions experienced by patients on chemotherapy. Some of these reactions depend on the dose given. Nausea, vomiting, anorexia, and diarrhea are seen with almost all products. Other common reactions include alopecia (hair loss) and bone marrow depression. (Patients with bone marrow depression are more likely to get infections and may show bruising or bleeding.) Renal toxicity, hepatic toxicity, ototoxicity, ocular effects, peripheral neurotoxicity, and hypersensitivity are common among these drugs, and patients must be monitored carefully.
Some reactions are so severe that the patient feels worse with therapy than with the malignancy. There may be no cure for the adverse effects except to stop therapy and not treat the malignancy. Knowledge about the most common adverse effects will help the nurse develop a care plan to prevent or reduce as many symptoms as possible.
Drug Interactions
Most antineoplastic drugs interact with other medications the patient may be taking. It is very important to consult the manufacturer’s guidelines before starting treatment.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn everything possible about the patient’s history, the type of malignancy and current status, medications taken, surgeries, allergies, and response. Many patients have numerous hospital admissions for treatment of a malignancy. Old hospital records should be read whenever possible to find accurate information and avoid the need for the patient to repeat information. The patient who comes into the hospital several times should be asked about progress since the last hospitalization. It is important to find out about the patient’s emotional and physical responses to the illness, as well as cultural beliefs, spiritual and family support, and acceptance of the problem.
n Diagnosis
What other problems does this patient have that may interfere with treatment? Are there adverse effects or disease progression that must be treated? Is the patient fearful or worried? Is money an issue?
n Planning
Read the latest product information about the preparation, storage, and administration of antineoplastic medications. Understand and follow all warnings, precautions, and contraindications. Some preparations should be given only by a physician or other health care provider or a specially trained chemotherapy nurse. New drug information is common.
The initial dosage of antineoplastic medication is often calculated in milligrams per kilogram (mg/kg) or milligrams per square meter of body surface area (mg/m2 BSA). These calculations are based on surface nomograms, which are provided in the drug maker’s product insert. The starting dosage will be calculated by the specialist, with future adjustments based on the patient’s response as measured by laboratory tests and x-ray studies.
Some medications given intravenously will damage and destroy the tissues of the skin if the IV needle becomes dislodged and medication goes into the tissue and not the veins. This is called extravasation. Medication must be on hand that can be immediately injected directly into the skin to counter the effect of the antitumor medicine. Failure to act quickly may result in huge areas of tissue damage, sometimes destroying the ability of the hand or arm to function.
n Implementation
Carefully follow the dosage, frequency, and administration procedures as outlined for any drugs the nurse is authorized to give. Administration of these toxic products may pose a safety hazard to the nurse, as well as the patient, if the products are not administered properly. The syringes, bottles, and needles must be handled and disposed of carefully. There should be a special area designated for mixing these preparations.
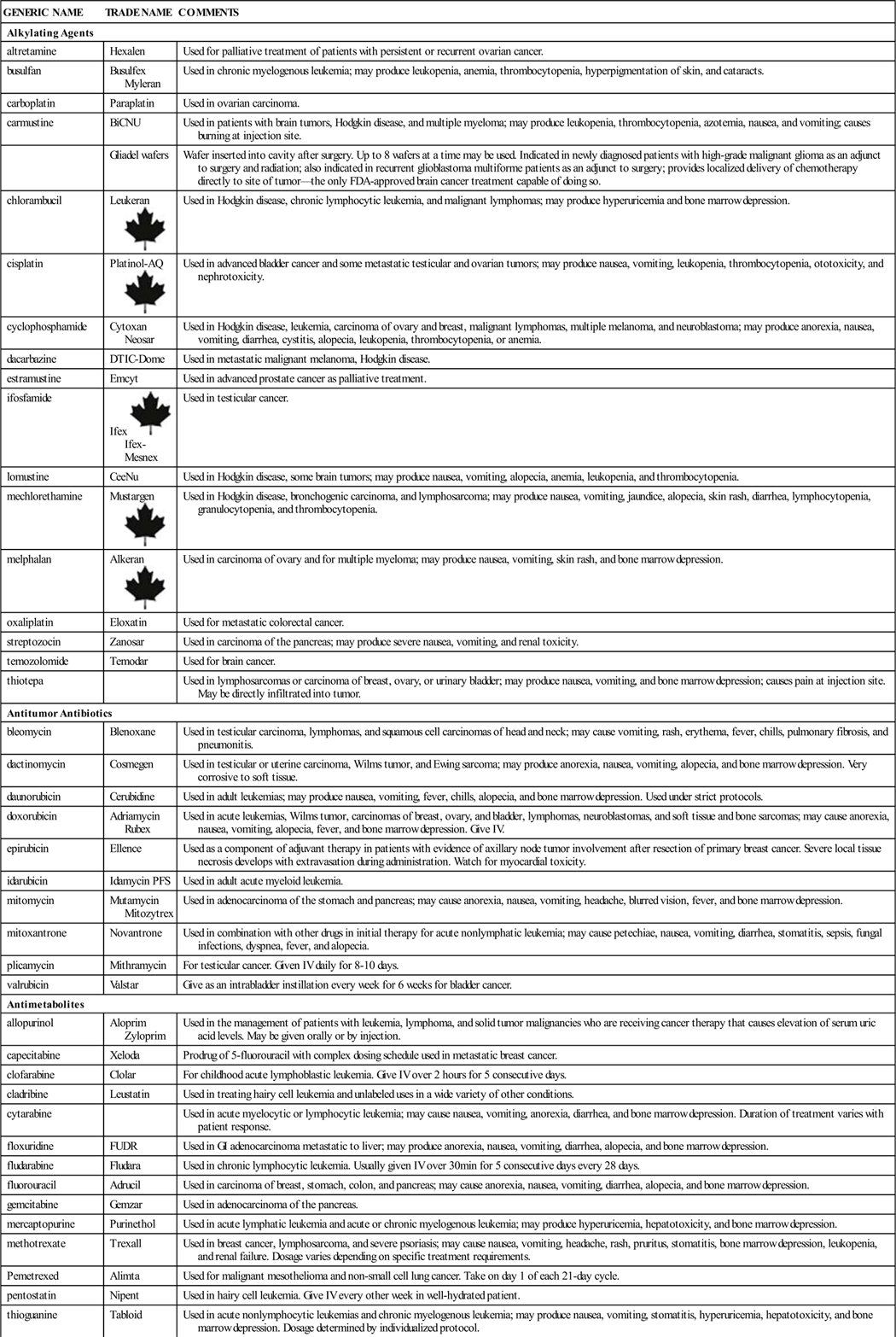
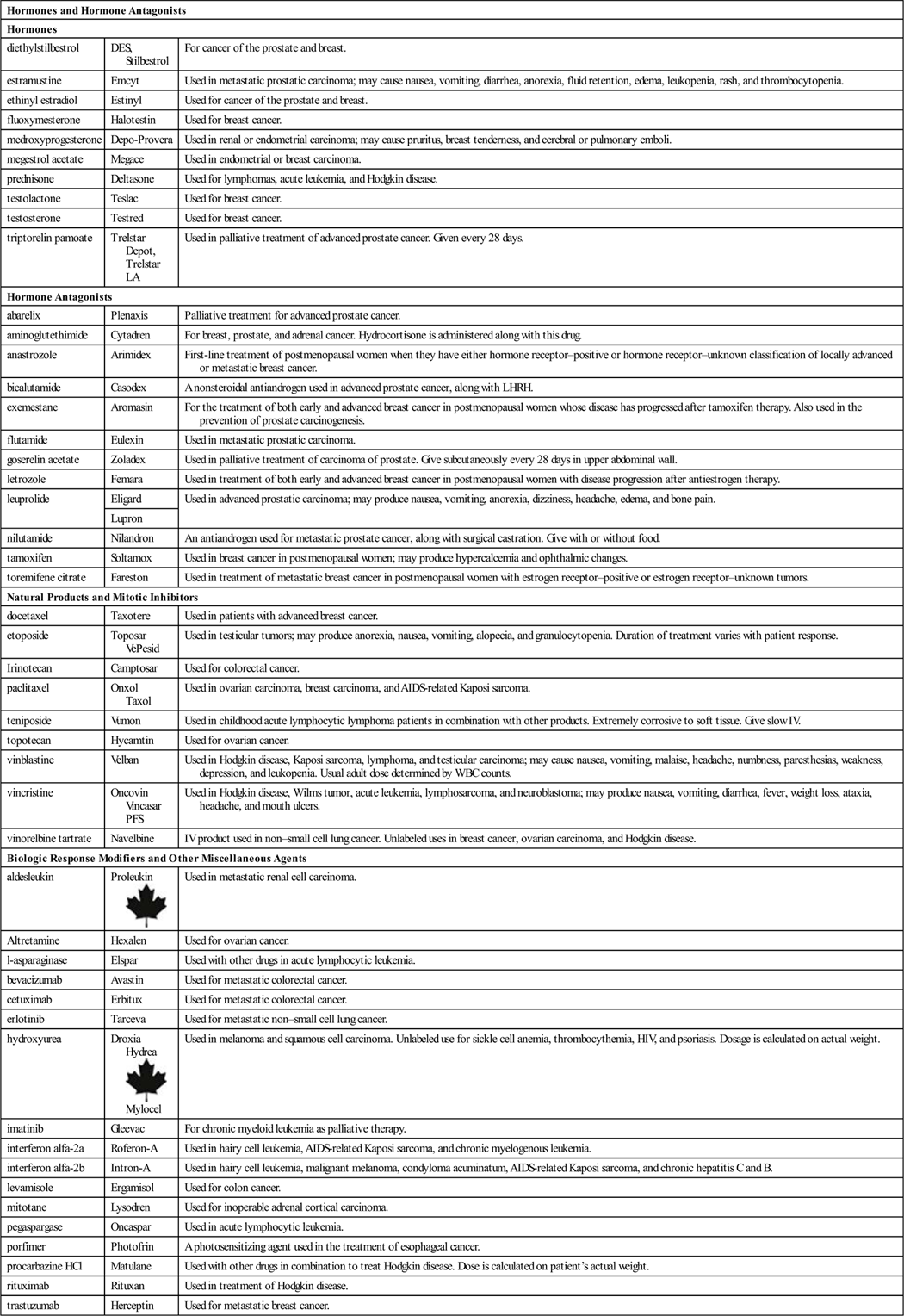
Table 14-1 presents the product information for the major antineoplastic agents. Additional detailed information on hormones may be found in Chapter 20.
![]() Table 14-1
Table 14-1
| GENERIC NAME | TRADE NAME | COMMENTS |
| Alkylating Agents | ||
| altretamine | Hexalen | Used for palliative treatment of patients with persistent or recurrent ovarian cancer. |
| busulfan | Busulfex Myleran |
Used in chronic myelogenous leukemia; may produce leukopenia, anemia, thrombocytopenia, hyperpigmentation of skin, and cataracts. |
| carboplatin | Paraplatin | Used in ovarian carcinoma. |
| carmustine | BiCNU | Used in patients with brain tumors, Hodgkin disease, and multiple myeloma; may produce leukopenia, thrombocytopenia, azotemia, nausea, and vomiting; causes burning at injection site. |
| Gliadel wafers | Wafer inserted into cavity after surgery. Up to 8 wafers at a time may be used. Indicated in newly diagnosed patients with high-grade malignant glioma as an adjunct to surgery and radiation; also indicated in recurrent glioblastoma multiforme patients as an adjunct to surgery; provides localized delivery of chemotherapy directly to site of tumor—the only FDA-approved brain cancer treatment capable of doing so. | |
| chlorambucil | Leukeran |
Used in Hodgkin disease, chronic lymphocytic leukemia, and malignant lymphomas; may produce hyperuricemia and bone marrow depression. |
| cisplatin | Platinol-AQ |
Used in advanced bladder cancer and some metastatic testicular and ovarian tumors; may produce nausea, vomiting, leukopenia, thrombocytopenia, ototoxicity, and nephrotoxicity. |
| cyclophosphamide | Cytoxan Neosar |
Used in Hodgkin disease, leukemia, carcinoma of ovary and breast, malignant lymphomas, multiple melanoma, and neuroblastoma; may produce anorexia, nausea, vomiting, diarrhea, cystitis, alopecia, leukopenia, thrombocytopenia, or anemia. |
| dacarbazine | DTIC-Dome | Used in metastatic malignant melanoma, Hodgkin disease. |
| estramustine | Emcyt | Used in advanced prostate cancer as palliative treatment. |
| ifosfamide | Ifex Ifex-Mesnex |
Used in testicular cancer. |
| lomustine | CeeNu | Used in Hodgkin disease, some brain tumors; may produce nausea, vomiting, alopecia, anemia, leukopenia, and thrombocytopenia. |
| mechlorethamine | Mustargen |
Used in Hodgkin disease, bronchogenic carcinoma, and lymphosarcoma; may produce nausea, vomiting, jaundice, alopecia, skin rash, diarrhea, lymphocytopenia, granulocytopenia, and thrombocytopenia. |
| melphalan | Alkeran |
Used in carcinoma of ovary and for multiple myeloma; may produce nausea, vomiting, skin rash, and bone marrow depression. |
| oxaliplatin | Eloxatin | Used for metastatic colorectal cancer. |
| streptozocin | Zanosar | Used in carcinoma of the pancreas; may produce severe nausea, vomiting, and renal toxicity. |
| temozolomide | Temodar | Used for brain cancer. |
| thiotepa | Used in lymphosarcomas or carcinoma of breast, ovary, or urinary bladder; may produce nausea, vomiting, and bone marrow depression; causes pain at injection site. May be directly infiltrated into tumor. | |
| Antitumor Antibiotics | ||
| bleomycin | Blenoxane | Used in testicular carcinoma, lymphomas, and squamous cell carcinomas of head and neck; may cause vomiting, rash, erythema, fever, chills, pulmonary fibrosis, and pneumonitis. |
| dactinomycin | Cosmegen | Used in testicular or uterine carcinoma, Wilms tumor, and Ewing sarcoma; may produce anorexia, nausea, vomiting, alopecia, and bone marrow depression. Very corrosive to soft tissue. |
| daunorubicin | Cerubidine | Used in adult leukemias; may produce nausea, vomiting, fever, chills, alopecia, and bone marrow depression. Used under strict protocols. |
| doxorubicin | Adriamycin Rubex |
Used in acute leukemias, Wilms tumor, carcinomas of breast, ovary, and bladder, lymphomas, neuroblastomas, and soft tissue and bone sarcomas; may cause anorexia, nausea, vomiting, alopecia, fever, and bone marrow depression. Give IV. |
| epirubicin | Ellence | Used as a component of adjuvant therapy in patients with evidence of axillary node tumor involvement after resection of primary breast cancer. Severe local tissue necrosis develops with extravasation during administration. Watch for myocardial toxicity. |
| idarubicin | Idamycin PFS | Used in adult acute myeloid leukemia. |
| mitomycin | Mutamycin Mitozytrex |
Used in adenocarcinoma of the stomach and pancreas; may cause anorexia, nausea, vomiting, headache, blurred vision, fever, and bone marrow depression. |
| mitoxantrone | Novantrone | Used in combination with other drugs in initial therapy for acute nonlymphatic leukemia; may cause petechiae, nausea, vomiting, diarrhea, stomatitis, sepsis, fungal infections, dyspnea, fever, and alopecia. |
| plicamycin | Mithramycin | For testicular cancer. Given IV daily for 8-10 days. |
| valrubicin | Valstar | Give as an intrabladder instillation every week for 6 weeks for bladder cancer. |
| Antimetabolites | ||
| allopurinol | Aloprim Zyloprim |
Used in the management of patients with leukemia, lymphoma, and solid tumor malignancies who are receiving cancer therapy that causes elevation of serum uric acid levels. May be given orally or by injection. |
| capecitabine | Xeloda | Prodrug of 5-fluorouracil with complex dosing schedule used in metastatic breast cancer. |
| clofarabine | Clolar | For childhood acute lymphoblastic leukemia. Give IV over 2 hours for 5 consecutive days. |
| cladribine | Leustatin | Used in treating hairy cell leukemia and unlabeled uses in a wide variety of other conditions. |
| cytarabine | Used in acute myelocytic or lymphocytic leukemia; may cause nausea, vomiting, anorexia, diarrhea, and bone marrow depression. Duration of treatment varies with patient response. | |
| floxuridine | FUDR | Used in GI adenocarcinoma metastatic to liver; may produce anorexia, nausea, vomiting, diarrhea, alopecia, and bone marrow depression. |
| fludarabine | Fludara | Used in chronic lymphocytic leukemia. Usually given IV over 30 min for 5 consecutive days every 28 days. |
| fluorouracil | Adrucil | Used in carcinoma of breast, stomach, colon, and pancreas; may cause anorexia, nausea, vomiting, diarrhea, alopecia, and bone marrow depression. |
| gemcitabine | Gemzar | Used in adenocarcinoma of the pancreas. |
| mercaptopurine | Purinethol | Used in acute lymphatic leukemia and acute or chronic myelogenous leukemia; may produce hyperuricemia, hepatotoxicity, and bone marrow depression. |
| methotrexate | Trexall | Used in breast cancer, lymphosarcoma, and severe psoriasis; may cause nausea, vomiting, headache, rash, pruritus, stomatitis, bone marrow depression, leukopenia, and renal failure. Dosage varies depending on specific treatment requirements. |
| Pemetrexed | Alimta | Used for malignant mesothelioma and non-small cell lung cancer. Take on day 1 of each 21-day cycle. |
| pentostatin | Nipent | Used in hairy cell leukemia. Give IV every other week in well-hydrated patient. |
| thioguanine | Tabloid | Used in acute nonlymphocytic leukemias and chronic myelogenous leukemia; may produce nausea, vomiting, stomatitis, hyperuricemia, hepatotoxicity, and bone marrow depression. Dosage determined by individualized protocol. |
| Hormones and Hormone Antagonists | ||
| Hormones | ||
| diethylstilbestrol | DES, Stilbestrol | For cancer of the prostate and breast. |
| estramustine | Emcyt | Used in metastatic prostatic carcinoma; may cause nausea, vomiting, diarrhea, anorexia, fluid retention, edema, leukopenia, rash, and thrombocytopenia. |
| ethinyl estradiol | Estinyl | Used for cancer of the prostate and breast. |
| fluoxymesterone | Halotestin | Used for breast cancer. |
| medroxyprogesterone | Depo-Provera | Used in renal or endometrial carcinoma; may cause pruritus, breast tenderness, and cerebral or pulmonary emboli. |
| megestrol acetate | Megace | Used in endometrial or breast carcinoma. |
| prednisone | Deltasone | Used for lymphomas, acute leukemia, and Hodgkin disease. |
| testolactone | Teslac | Used for breast cancer. |
| testosterone | Testred | Used for breast cancer. |
| triptorelin pamoate | Trelstar Depot, Trelstar LA | Used in palliative treatment of advanced prostate cancer. Given every 28 days. |
| Hormone Antagonists | ||
| abarelix | Plenaxis | Palliative treatment for advanced prostate cancer. |
| aminoglutethimide | Cytadren | For breast, prostate, and adrenal cancer. Hydrocortisone is administered along with this drug. |
| anastrozole | Arimidex | First-line treatment of postmenopausal women when they have either hormone receptor–positive or hormone receptor–unknown classification of locally advanced or metastatic breast cancer. |
| bicalutamide | Casodex | A nonsteroidal antiandrogen used in advanced prostate cancer, along with LHRH. |
| exemestane | Aromasin | For the treatment of both early and advanced breast cancer in postmenopausal women whose disease has progressed after tamoxifen therapy. Also used in the prevention of prostate carcinogenesis. |
| flutamide | Eulexin | Used in metastatic prostatic carcinoma. |
| goserelin acetate | Zoladex | Used in palliative treatment of carcinoma of prostate. Give subcutaneously every 28 days in upper abdominal wall. |
| letrozole | Femara | Used in treatment of both early and advanced breast cancer in postmenopausal women with disease progression after antiestrogen therapy. |
| leuprolide | Eligard | Used in advanced prostatic carcinoma; may produce nausea, vomiting, anorexia, dizziness, headache, edema, and bone pain. |
| Lupron | ||
| nilutamide | Nilandron | An antiandrogen used for metastatic prostate cancer, along with surgical castration. Give with or without food. |
| tamoxifen | Soltamox | Used in breast cancer in postmenopausal women; may produce hypercalcemia and ophthalmic changes. |
| toremifene citrate | Fareston | Used in treatment of metastatic breast cancer in postmenopausal women with estrogen receptor–positive or estrogen receptor–unknown tumors. |
| Natural Products and Mitotic Inhibitors | ||
| docetaxel | Taxotere | Used in patients with advanced breast cancer. |
| etoposide | Toposar VePesid |
Used in testicular tumors; may produce anorexia, nausea, vomiting, alopecia, and granulocytopenia. Duration of treatment varies with patient response. |
| Irinotecan | Camptosar | Used for colorectal cancer. |
| paclitaxel | Onxol Taxol |
Used in ovarian carcinoma, breast carcinoma, and AIDS-related Kaposi sarcoma. |
| teniposide | Vumon | Used in childhood acute lymphocytic lymphoma patients in combination with other products. Extremely corrosive to soft tissue. Give slow IV. |
| topotecan | Hycamtin | Used for ovarian cancer. |
| vinblastine | Velban | Used in Hodgkin disease, Kaposi sarcoma, lymphoma, and testicular carcinoma; may cause nausea, vomiting, malaise, headache, numbness, paresthesias, weakness, depression, and leukopenia. Usual adult dose determined by WBC counts. |
| vincristine | Oncovin Vincasar PFS |
Used in Hodgkin disease, Wilms tumor, acute leukemia, lymphosarcoma, and neuroblastoma; may produce nausea, vomiting, diarrhea, fever, weight loss, ataxia, headache, and mouth ulcers. |
| vinorelbine tartrate | Navelbine | IV product used in non–small cell lung cancer. Unlabeled uses in breast cancer, ovarian carcinoma, and Hodgkin disease. |
| Biologic Response Modifiers and Other Miscellaneous Agents | ||
| aldesleukin | Proleukin |
Used in metastatic renal cell carcinoma. |
| Altretamine | Hexalen | Used for ovarian cancer. |
| l-asparaginase | Elspar | Used with other drugs in acute lymphocytic leukemia. |
| bevacizumab | Avastin | Used for metastatic colorectal cancer. |
| cetuximab | Erbitux | Used for metastatic colorectal cancer. |
| erlotinib | Tarceva | Used for metastatic non–small cell lung cancer. |
| hydroxyurea | Droxia Hydrea Mylocel |
Used in melanoma and squamous cell carcinoma. Unlabeled use for sickle cell anemia, thrombocythemia, HIV, and psoriasis. Dosage is calculated on actual weight. |
| imatinib | Gleevac | For chronic myeloid leukemia as palliative therapy. |
| interferon alfa-2a | Roferon-A | Used in hairy cell leukemia, AIDS-related Kaposi sarcoma, and chronic myelogenous leukemia. |
| interferon alfa-2b | Intron-A | Used in hairy cell leukemia, malignant melanoma, condyloma acuminatum, AIDS-related Kaposi sarcoma, and chronic hepatitis C and B. |
| levamisole | Ergamisol | Used for colon cancer. |
| mitotane | Lysodren | Used for inoperable adrenal cortical carcinoma. |
| pegaspargase | Oncaspar | Used in acute lymphocytic leukemia. |
| porfimer | Photofrin | A photosensitizing agent used in the treatment of esophageal cancer. |
| procarbazine HCl | Matulane | Used with other drugs in combination to treat Hodgkin disease. Dose is calculated on patient’s actual weight. |
| rituximab | Rituxan | Used in treatment of Hodgkin disease. |
| trastuzumab | Herceptin | Used for metastatic breast cancer. |
n Evaluation
Check the patient closely for adverse effects, regularly noting subjective complaints or objective findings on the chart so the physician or other health care provider may follow the patient’s progress. Teach the patient which symptoms to report to the nurse, physician, or other health care provider after discharge, when medications will be given on an outpatient basis. Table 14-1 includes a listing of common adverse effects for many of these drugs.
Nursing or pharmacologic interventions are often needed to reduce adverse effects. Some of the common problems and their treatment are included in Table 14-2.
Table 14-2
Common Symptoms Following Chemotherapy and Their Treatment
| SYMPTOMS OR PROBLEM | SUGGESTED TREATMENT |
| Nausea and or vomiting | Provide antiemetics. Some herbal preparations may be helpful. Drink liquids between meals and not with food. |
| Stomatitis | Practice good oral hygiene with soft tooth brush, water or mild salt solution; avoid alcohol-based mouthwash. Use mouth rinse such as Maalox, Xylocaine, Benadryl, BMX. Avoid hot, cold, or other products that might damage sensitive tissue. Increase fluid intake to decrease the risk of kidney damage and the formation of uric acid crystals. |
| Skin breakdown | Provide vitamin supplementation, practice good skin care. |
| Pain at surgical site | Provide analgesics or narcotics. |
| Dehydration | Force fluids, provide IV hydration. |
| Low WBC count or bone marrow suppression | Use neutropenic diet: avoid raw fish and meat, raw fruits and vegetables, or peppercorns. Watch for elevated temperatures. Stay away from other people or even use reverse isolation; provide interferon alfa-2 for severe problems. |
| Low platelet counts | Report any bruising, blood in urine or stools, severe fatigue, epigastric pain, difficulty clotting. Provide oprelvekin for severe problems. |
| Anemia | Provide epoetin alfa |
| Anorexia | Provide small feedings. Megestrol acetate is an appetite stimulant. |
| Reduced fertility | Consider sperm banking prior to chemotherapy. Chemotherapy may reduce sperm count or increase risk of genetic damage to sperm. |
The patient should be taught about the need to get follow-up laboratory work and x-ray studies to determine the response to medication. The nurse takes time and provides opportunities for patients to discuss their feelings and attitudes about the disease and their therapy.
n Patient and Family Teaching

