CASE 14
Josh is a 19-year-old man who has been rushed to your emergency department from a local Italian restaurant, where he had become acutely “ill” while eating. On arrival he is pale, cool, and clammy and has a low blood pressure. There is no medic-alert bracelet to be seen. Putting your stethoscope to his chest you find he has wheezes throughout his lung fields but very poor air intake. A friend who is with him says this has never happened before, and, to his knowledge, no one in Josh’s family has ever been like this. What are your thoughts on how to proceed?
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Clinical History
A number of nontrauma conditions can manifest in this manner. For example, patients experiencing septic shock as a result of gram-negative bacterial infection, dehydration, or heart damage may also present with similar symptoms. Josh’s illness, however, occurred suddenly while eating at an Italian restaurant, and this should steer us away from these causes. The acute presentation of Josh’s symptoms while eating is a strong indication that something this patient ate is most likely the precipitating factor. Ingested toxins (poisons) or a protein to which Josh had been previously sensitized are both in the realm of possibilities because these stimuli can induce the observed clinical “picture.”
THERAPY
Pharmacologic Intervention
Epinephrine
Epinephrine needs to be given first! Subcutaneous administration of epinephrine produces an immediate response (seconds to minutes). It is the treatment of choice because it stimulates α-, β1-, and β2-adrenergic receptors. Stimulation of β2-adrenergic receptors leads to an increase in cyclic adenosine monophosphate and relaxation of smooth muscles surrounding the bronchi and bronchioles, which results in bronchodilation (eliminates wheezing). Additionally, β2 agonists enhance clearance of mucus and inhibit the release of inflammatory mediators from mast cells/basophils. Stimulation of α-adrenergic receptors constricts blood vessels and increases heart rate and blood pressure. The action of epinephrine lasts for 30 to 90 minutes.
Long-Term Care
Many allergic reactions are inconvenient but not life threatening. Welts after insect bites (local histamine release to insect saliva) and orbital edema on exposure to cat/animal dander are two such examples (Fig. 14-1). Other allergies kill people! These life-threatening allergies include some food allergies (nuts/shellfish) and some allergies to insect stings (yellow jackets). Therefore, Josh should be advised to carry an epinephrine-containing pen (Epi-Pen) to deliver immediate epinephrine in the event of re-exposure, as well as diphenhydramine (Benadryl) (to be taken after epinephrine, as the patient is en route to the hospital). A medic-alert bracelet (in case a patient is ever unable to communicate significant medical history to caregivers) is essential.
IMMUNE-MEDIATED ANAPHYLAXIS
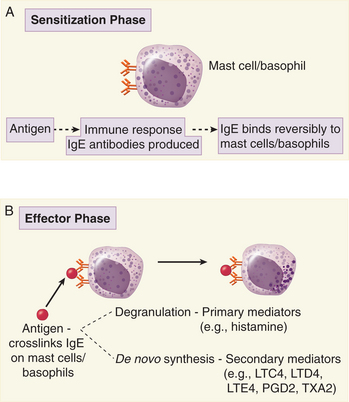
Immune-mediated anaphylaxis is the effector phase, or clinical manifestation, of a type I hypersensitivity reaction. These reactions are, as the term implies, an exaggerated (hyper) response to an allergen and occur only after a sensitization phase in which IgE antibodies are produced. In Josh’s case, it appears that the allergen is a protein, perhaps found in peanut oil or in shellfish.
Sensitization Phase
In the initial response to the allergen, IgE antibodies do not appear for at least 7 to 10 days after protein ingestion because of the length of time required for B cells to undergo antigen-induced differentiation and isotype switching to IgE. By this time, the allergen has long been removed from the system, so there is no antigen available to bind the newly generated IgE. Consequently, IgE antibodies bind to Fcε receptors present on mast cells and basophils (Fig. 14-2A). Although circulating IgE antibodies have a very short half-life, antibodies bound to mast cells can persist for months. Because these IgE antibodies are bound via their Fc regions, the antigen-binding sites are readily available to bind the allergen should it enter the system again. An absolute requirement for a type I hypersensitivity reaction is the localization of IgE antibodies on mast cells and basophils, and so the effector phase/clinical manifestation cannot occur in the absence of previous exposure to the allergen.
Effector Phase
In cases of food allergies, there is a breakdown in oral tolerance such that allergen-specific IgE antibodies are generated and bind to mast cells/basophils. The effector phase is initiated when allergens (e.g., food allergen) enter the circulation and crosslink two IgE antibodies bound via their Fc regions to Fcε receptors on mast cells or basophils (see Fig. 14-2B). When the allergen crosslinks the IgE antibodies on these cells, tyrosine kinases are activated and numerous proteins are phosphorylated, including phospholipase Cγ1 and Cγ2. It is thought that this phosphorylation event triggers phospholipase C activation because inositol phospholipids are degraded and calcium is released from intracellular stores. Following these signal transduction events, mast cells degranulate, causing the release of histamine, proteases, and chemotactic factors. Crosslinking of IgE on the surface of mast cells/basophils also leads to the activation of phospholipase A2. In some cases, this manifests as allergic urticaria.