CASE 138
History: A 3-year-old boy presents with vomiting.
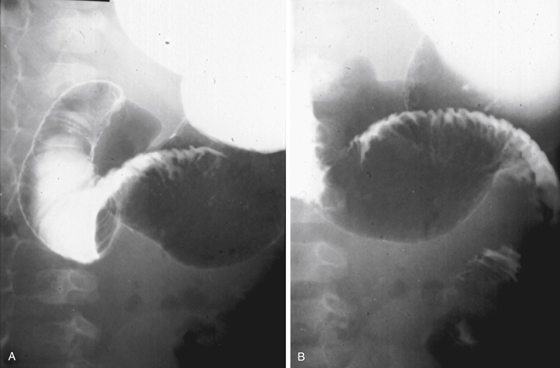
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
E. Duodenal intraluminal diverticulum
2. Which of the following patterns is diagnostic of a duodenal hematoma on CT scan?
D. Asymmetric ovoid intramural mass
3. What is the most common cause of a duodenal hematoma?
4. Which of the following statements regarding blunt abdominal trauma in children is true?
B. The most common intestinal injury is hematoma formation and obstruction.
C. There is a higher mortality with pancreatic than with intestinal tract injury.
D. The most common site of injury is the duodenum.
ANSWERS
CASE 138
Duodenal Hematoma
1. B, C, and D
2. D
3. A
4. A
References
Iuchtman M, Steiner T, Faierman T, et al: Post-traumatic intramural duodenal hematoma in children. Isr Med Assoc J. 2006;8(2):95–97.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 97.
Comment
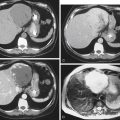
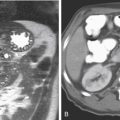
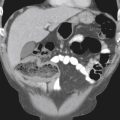
Numerous references in the literature discuss large duodenal hematomas being mistakenly diagnosed as upper abdominal masses (see figures). These hematomas may be present without a history of trauma. Huge lymphomatous masses (root of mesentery and retroperitoneal adenopathy) through which the duodenum passes unobstructed—the so-called sandwich sign—are a good example. The patient in this case experienced both gastric outlet obstruction and a degree of obstruction of the biliary duct, had decompression of the obstruction performed with a nasogastric tube, and was treated conservatively and continuously improved. No bile duct intervention was required, and a repeat study obtained 6 weeks later showed almost complete resolution of the hematoma. Not all large upper abdominal hematomas manifest with a history of trauma. Sometimes the history is suppressed. Sometimes the patient has a coagulability problem. Sometimes the hematoma is entirely idiopathic. Some of these patients are diagnosed at surgery.