CASE 136

1. What etiologies can cause the finding seen in Fig. A? (Choose all that apply.)
A. Trauma
C. Barotrauma
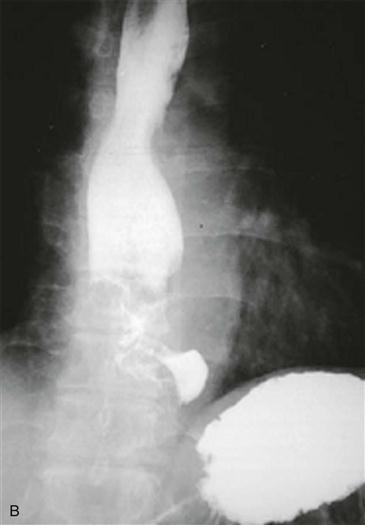
2. What finding is seen on the upper gastrointestinal (GI) examination (Fig. B)?
A. Achalasia
3. In the absence of a history of instrumentation, what is the most likely cause of the finding in Fig. A?
A. Trauma
4. What is the most likely cause of the patient’s fever?
A. Aspiration
B. Pneumonia
C. Abscess
D. Pericarditis
ANSWERS
References
Kaufman J, Thongsuwan N, Stern E, et al. Esophageal-pericardial fistula with purulent pericarditis secondary to esophageal carcinoma presenting with tamponade. Ann Thorac Surg. 2003;75(1):288–289.
Meltzer P, Elkayam U, Parsons K, et al. Esophageal-pericardial fistula presenting as pericarditis. Am Heart J. 1983;105(1):148–150.
Comment
Etiology
Hydropneumopericardium usually occurs after pericardiocentesis or placement of a pericardial drain. Other causes, such as a fistula, are rare. Tumors that invade the pericardium include breast carcinoma, lung carcinoma, lymphoma, and esophageal carcinoma. Patients with a malignant esophageal-pericardial fistula usually have a diagnosis of metastatic cancer elsewhere in the body.
Imaging
Chest radiography can demonstrate hydropneumopericardium (Fig. A), as can CT, MRI, and echocardiography. Contrast esophagram or endoscopy is helpful in confirming a diagnosis of esophageal carcinoma in patients with suspected malignant fistulae (Fig. B). Patients with malignant or nonmalignant esophageal-pericardial fistula generally have an infected pericardial space. Treatment of a malignant esophageal-pericardial fistula generally requires open drainage and debridement followed by endoscopic placement of an esophageal stent. Percutaneous drainage procedures are generally inadequate as there are often extensive adhesions. Nonmalignant fistulas should ideally be surgically excised or ablated.