CHAPTER 134
Multiple Sclerosis
Definition
Multiple sclerosis (MS) can be defined as an inflammatory disorder that results in damage, primarily to myelin sheaths and oligodendrocytes and less so to axons and nerve cells, in the central nervous system [1,2].
The prevalence of MS has been estimated at 300,000 to 400,000 in the United States and 2 million worldwide [3]. The disease usually becomes clinically apparent between the ages of 20 and 40 years, with a peak incidence at 24 to 30 years and onset as late as the seventh decade [3]. The disease appears twice as likely to develop in women as in men, and whites are more frequently diagnosed than are other races [3]. Although African Americans may experience greater MS-related disability than white individuals do, the disease progresses similarly for both races [3,4].
There are four common clinical courses in MS:
• Secondary progressive MS: Patients initially experience a relapsing-remitting course followed by progression of the disease with or without additional episodes of exacerbation and improvement. Most patients eventually transition to this disease course.
• Primary progressive MS: Patients experience a relentless progression of symptoms from the onset [5,6].
• Progressive relapsing MS: Patients experience a baseline progressive course with episodes of acute relapses followed by a return to the baseline progressive course.
MS can be diagnosed if there is evidence of two attacks disseminated in time and space with clinical, laboratory, or imaging evidence of at least two lesions in the brain or spinal cord [1–3,7]. Evidence may be obtained from clinical findings, magnetic resonance imaging, cerebrospinal fluid analysis, or visual evoked potentials [6,7]. Other diseases that could explain the symptoms must be excluded (see differential diagnosis) [8,9]. The most recent guidelines and revisions do not recommend the use of “clinically definite MS” or “probable MS”; the outcome of a diagnostic evaluation is MS, “possible MS,” or “not MS” (Table 134.1) [2,6,7].
Table 134.1
The 2010 McDonald Criteria for Diagnosis of Multiple Sclerosis
| Clinical Presentation | Additional Data Needed for MS Diagnosis |
| ≥ 2 attacks*; objective clinical evidence of ≥ 2 lesions or objective clinical evidence of 1 lesion with reasonable historical evidence of a prior attack† | None‡ |
| ≥ 2 attacks*; objective clinical evidence of 1 lesion | Dissemination in space, demonstrated by: ≥ 1 T2 lesion in at least 2 of 4 MS-typical regions of the CNS (periventricular, juxtacortical, infratentorial, or spinal cord)§; or Await a further clinical attack* implicating a different CNS site |
| 1 attack*; objective clinical evidence of ≥ 2 lesions | Dissemination in time, demonstrated by: Simultaneous presence of asymptomatic gadolinium-enhancing and nonenhancing lesions at any time; or A new T2 and/or gadolinium-enhancing lesion(s) on follow-up MRI, irrespective of its timing with reference to a baseline scan; or Await a second clinical attack* |
| 1 attack*; objective clinical evidence of 1 lesion (clinically isolated syndrome) | Dissemination in space and time, demonstrated by: For DIS: ≥ 1 T2 lesion in at least 2 of 4 MS-typical regions of the CNS (periventricular, juxtacortical, infratentorial, or spinal cord)§; or Await a second clinical attack* implicating a different CNS site; and For DIT: Simultaneous presence of asymptomatic gadolinium-enhancing and nonenhancing lesions at any time; or A new T2 and/or gadolinium-enhancing lesion(s) on follow-up MRI, irrespective of its timing with reference to a baseline scan; or Await a second clinical attack* |
| Insidious neurological progression suggestive of MS (PPMS) | 1 year of disease progression (retrospectively or prospectively determined) plus 2 of 3 of the following criteria§: 1. Evidence for DIS in the brain based on ≥ 1 T2 lesions in the MS-characteristic (periventricular, juxtacortical, or infratentorial) regions 2.Evidence for DIS in the spinal cord based on ≥ 2 T2 lesions in the cord 3. Positive CSF (isoelectric focusing evidence of oligoclonal bands and/or elevated IgG index) |
From Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 2011;69:292-302.
If the criteria are fulfilled and there is no better explanation for the clinical presentation, the diagnosis is “MS”; if suspicious, but the criteria are not completely met, the diagnosis is “possible MS”; if another diagnosis arises during the evaluation that better explains the clinical presentation, then the diagnosis is “not MS.”
MS, multiple sclerosis; CNS, central nervous system; MRI, magnetic resonance imaging; DIS, dissemination in space; DIT, dissemination in time; PPMS, primary progressive multiple sclerosis; CSF, cerebrospinal fluid; IgG, immunoglobulin G.
* An attack (relapse; exacerbation) is defined as patient-reported or objectively observed events typical of an acute inflammatory demyelinating event in the CNS, current or historical, with duration of at least 24 hours, in the absence of fever or infection. It should be documented by contemporaneous neurological examination, but some historical events with symptoms and evolution characteristic for MS, but for which no objective neurological findings are documented, can provide reasonable evidence of a prior demyelinating event. Reports of paroxysmal symptoms (historical or current) should, however, consist of multiple episodes occurring over not less than 24 hours. Before a definite diagnosis of MS can be made, at least 1 attack must be corroborated by findings on neurological examination, visual evoked potential response in patients reporting prior visual disturbance, or MRI consistent with demyelination in the area of the CNS implicated in the historical report of neurological symptoms.
† Clinical diagnosis based on objective clinical findings for 2 attacks is most secure. Reasonable historical evidence for 1 past attack, in the absence of documented objective neurological findings, can include historical events with symptoms and evolution characteristics for a prior inflammatory demyelinating event; at least 1 attack, however, must be supported by objective findings.
‡ No additional tests are required. However, it is desirable that any diagnosis of MS be made with access to imaging based on these criteria. If imaging or other tests (for instance, CSF) are undertaken and are negative, extreme caution needs to be taken before making a diagnosis of MS, and alternative diagnoses must be considered. There must be no better explanation for the clinical presentation, and objective evidence must be present to support a diagnosis of MS.
§ Gadolinium-enhancing lesions are not required; symptomatic lesions are excluded from consideration in subjects with brainstem or spinal cord syndromes.
Symptoms
Symptoms of MS may involve multiple systems [10,11] (Table 134.2). Motor symptoms typically include weakness and spasticity [11]. Up to 85% of patients with MS may experience spasticity, and as many as a third may be affected by spasticity that is severe enough to diminish their quality of life [12]. Patients with MS may report paroxysmal spasms or nocturnal spasms.
Table 134.2
Common Symptoms in Multiple Sclerosis
| Bladder symptoms | Urgency, frequency, hesitancy, retention, incontinence |
| Bowel symptoms | Constipation, urgency, incontinence |
| Cerebellar symptoms | Incoordination, imbalance, tremor |
| Cognition | Concentration, memory, executive dysfunction |
| Fatigue | Lassitude, reduced endurance |
| Mood disorders | Depression, anxiety, emotional lability |
| Motor | Weakness, spasticity |
| Sensory symptoms | Loss of sensation, positive sensations |
| Sexual dysfunction | Decreased libido, erectile dysfunction |
| Vision | Visual loss and double vision |
From Goldman MD, Cohen JA, Fox RJ, Bethoux FA. Multiple sclerosis: treating symptoms, and other general medical issues. Cleve Clin J Med 2006;73:178.
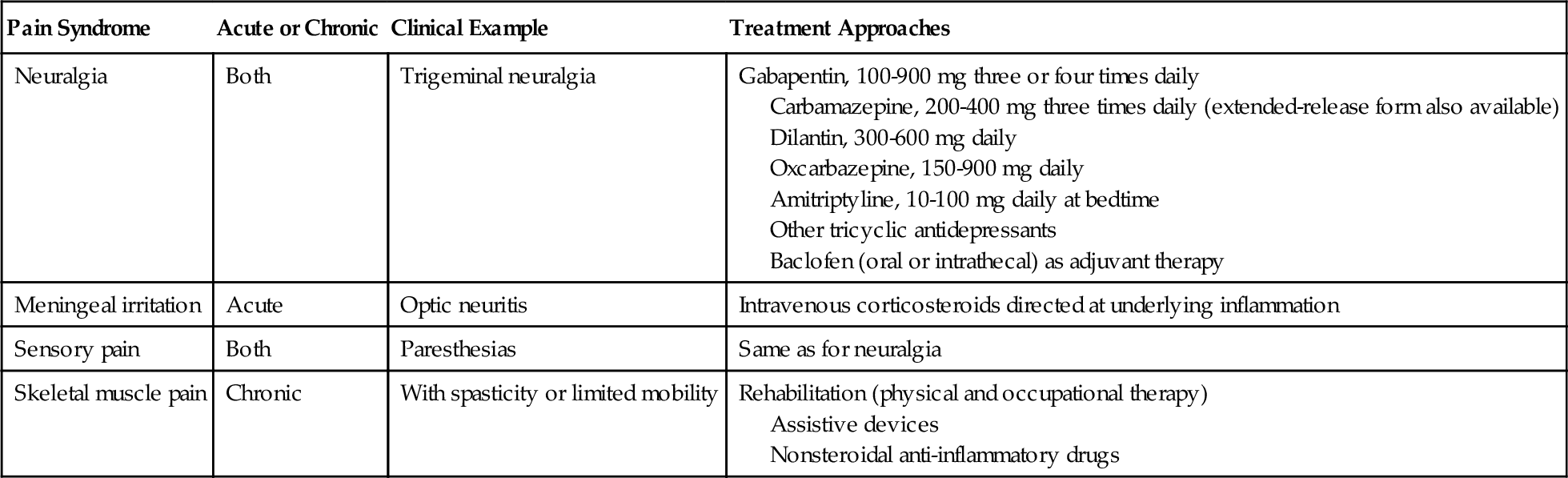
MS may be the cause of decreased or even absent sensation in various body parts, including sensory levels that most often affect the trunk. Paresthesia (uncomfortable abnormal sensation that may be described by the patient as pain, pins and needles, or tingling) can occur in up to 50% of patients with MS and most commonly is neuropathic. Lhermitte sign is an electric shock–like sensation that radiates down the spine to the legs when the neck is flexed [10]. It may occur in up to 40% of patients with MS [7]. Multiple pain syndromes may occur in patients with MS [11,13] (Table 134.3). Visual symptoms may include optic neuritis that results from inflammation of the optic nerves and typically is manifested as retro-orbital pain or painful eye movements [14]. Visual deficits can range from mild distortions to complete visual loss [14]. Scotoma may be present as an area in the visual field with absent or impaired vision and dyschromatopsia as imperfect color vision [14]. Ocular motor deficits usually include internuclear ophthalmoplegia and nystagmus and are manifested as diplopia, blurry vision, and reading fatigue [14].
Cerebellar symptoms may include tremor, which can range from mildly annoying to disabling, be gross or fine, and occur at rest or with purposeful actions. Various parts of the body may be involved, including the head, the upper or lower limbs, and the trunk.
Constipation and bowel incontinence may occur in up to 73% of patients with MS [15]. More than 70% of patients with MS may suffer from bladder dysfunction [15]. MS lesions in the spinal cord can result in a small spastic bladder due to detrusor overactivity. This usually is manifested as urinary urgency, frequency, voiding of small amounts of urine, and eventually incontinence [15]. Bladder underactivity can result in retention and overflow incontinence. Bladder dysfunction is often associated with urinary tract infections that can worsen MS symptoms. Sexual dysfunction commonly includes erectile and ejaculatory dysfunction in men; vaginal dryness in women; and increased time to arousal, decreased genital sensation, and decreased libido in men and women [15]. Factors contributing to sexual dysfunction include disease progression, antidepressants, fatigue, and depression [15].
Involvement of cranial nerves VII, IX, X, and XII may result in dysphagia or swallowing difficulties. These are manifested as coughing, frequent throat clearing, complaints of food “sticking” in the throat, weight loss, weak voice, choking, or even aspiration pneumonia [16].
Fatigue has been reported to occur in more than 90% of MS patients and is regarded as the most disabling symptom in as many as 60% of these patients [15,17]. MS-related fatigue has been described as an overwhelming feeling of tiredness, lack of energy, or exhaustion exceeding the expected [15,17].
As many as 50% of patients with MS may have cognitive deficits that are manifested as problems with memory, planning, concentration, judgment, problem solving, and processing speed [18–21]. MS patients frequently report heat intolerance with an exacerbation of symptoms in warm or humid environments [22].
Physical Examination
Inflammation of the optic nerve may result in optic or retrobulbar neuritis manifesting as acute vision loss. Even after treatment, vision deficits may persist in the form of poor vision, especially in dim light, or blind spots in the visual field known as scotomas. Demyelination in the medial longitudinal fasciculus may result in varying degrees of horizontal nystagmus; involvement of the third cranial nerve may be manifested as a persistently enlarged pupil. Double vision may be attributable to weakened strength and coordination in the eye muscles. Cataracts may develop at an earlier age in the MS population because of the use of steroids. Visual problems may worsen with stress, increased temperature, and infection [14].
Speech dysfunction may include dysarthria with diminished fluency, slurring, decreased speed, and eventually incomprehensibility.
Sensory testing may reveal deficits in pinprick, temperature, proprioception, or vibration. A sensory level may be evident.
Manual muscle testing can show varying degrees of muscle weakness. The patient may exhibit poor control of a limb or insufficient clearance of the foot during gait. Spastic gait may be another motor finding. Cerebellar involvement may be manifested as dysmetria with past pointing on finger to nose testing and uncoordinated heel to shin movements. The Ashworth Scale (or Modified Ashworth Scale) [23] is commonly used to measure the amount of spasticity, and the 88-item Multiple Sclerosis Spasticity Scale is a reliable and valid measure of the impact of spasticity in patients with MS [24].
Early in the course, deep tendon reflexes tend to be hyperactive. Decreased or absent reflexes can represent segmental levels of deficit. Corticospinal tract involvement may be evident with an asymmetric plantar response or loss of the abdominal reflex. Deep tendon reflexes can also be asymmetric; testing them in more than one position can determine the consistency of the findings.
Cognitive testing may reveal multiple deficits, including in memory, problem solving, judgment, and concentration.
Functional Limitations
The combinations of deficits in MS lead to difficulties with activities of daily living and mobility. Weakness, incoordination, spasticity, or sensory deficits may each or in combination contribute to falls. In addition to possible injuries, these falls may lead to decreased mobility because of fear of repeated falls. Decreased mobility itself leads to further weakness, decreased endurance, and less independence. Weakness or spasticity can also lead to difficulties with feeding and self-care, resulting in the need for personal care attendants. The Multiple Sclerosis Functional Composite is a clinical measure developed by a task force of the National Multiple Sclerosis Society [25,26] and is mostly used in clinical trials. It measures ambulation, arm and hand function, and cognition and has been found to have greater reliability, sensitivity, and validity than the Kurtzke Expanded Disability Status Scale [3].
Bowel and bladder dysfunction can contribute to many embarrassing moments in the community, causing patients with MS to fear leaving home or to become distracted by seeking out the locations of bathrooms in areas they plan to visit. Many resort to wearing diapers or catheters. Fear of bladder incontinence may also lead a patient to decrease fluid intake, resulting in dehydration.
Depression, insomnia, and fatigue can all contribute to activity intolerance.
Visual deficits may limit activities such as driving and reading, thus limiting participation in work and recreation.
Diagnostic Studies
Magnetic resonance imaging is the most important test in the diagnosis and management of MS [27]. The use of gadolinium allows enhancement of active inflammatory lesions that represent areas with blood-brain barrier breakdown. These hyperintense lesions on T2-weighted images are more specific for MS if they are located in the cerebral white matter, especially the corpus callosum, periventricular area, and brainstem [6].
Cerebrospinal fluid studies, visual evoked potentials, and brainstem auditory evoked potentials can assist in the diagnosis of MS when magnetic resonance imaging findings but not clinical findings support a diagnosis of MS [6,22].
Treatment
Initial
Treatment of patients with MS requires a multidisciplinary approach that should involve careful identification of the symptoms with consideration given to the consequences of these symptoms. Symptoms then need to be prioritized and a treatment plan formulated with use, where appropriate, of nonpharmacologic interventions first [28–33].
Education of the patient and family should be included in any initial treatment plan involving patients with MS. This provides information about a balanced diet [34], including adequate fluid intake, weight control, and appropriate exercise [35]. The patient is encouraged to continue working and participating in recreational activities for as long as possible. Modifications may be necessary to allow these activities to continue. The health care providers, the family, and the patient should closely monitor emotional stability, especially mood, because such conditions as depression can contribute to disability. Disabled parking placards can make the task of driving and parking more convenient for the disabled patient with MS.
High-dose methylprednisolone for 3 to 5 days has been established as effective treatment of acute relapses [36,37]. This can be given in a home or hospital setting with similar efficacy [38]. The medications approved by the U.S. Food and Drug Administration (FDA) that are available as first-line treatment to decrease the relapse rate in relapsing-remitting MS include interferon beta-1a (Avonex, Rebif), interferon beta-1b (Betaseron, Extavia), glatiramer acetate (Copaxone), mitoxantrone (Novantrone), natalizumab (Tysabri), and fingolimod (Gilenya) [39]. Fingolimod offers the advantage of oral administration and may be the most effective in decreasing relapse frequency in relapsing-remitting MS [40].
Spasticity management can be complex (see Chapter 153). Some patients use their spasticity to assist with transfers or gait; therefore, spasticity should be treated only if it interferes with mobility or activities of daily living. The first step is seeking and treatment of noxious stimuli, such as pain or infection, especially urinary tract infections, because such stimuli can exacerbate spasticity [41]. Treatment options include physical therapy (see the section on rehabilitation), oral or intrathecal medications, and nerve or muscle blocks [41].
Oral baclofen is the usual first-line treatment, starting with 5 mg two or three times per day and titrating up to the FDA-recommended maximum of 80 mg/day in divided doses. Patients with severe spasticity may require and have been shown to tolerate higher doses (up to 160 mg/day) [42]. Tizanidine, an α-adrenergic receptor antagonist, has been shown to be effective in reducing muscle tone in patients with MS [43]. Dosing should be started at 2 mg and slowly increased to the effective dose of 24 to 36 mg/day in three divided doses [41]. Side effects can include sedation, dry mouth, and weakness. Tizanidine may cause less weakness but more severe dry mouth compared with baclofen [44]. The GABAergic drugs gabapentin (Neurontin) and pregabalin (Lyrica) have been shown to have antispasticity properties [41] and can be used as monotherapy or in addition to baclofen or tizanidine. Sedation is the most common side effect. Benzodiazepines, such as diazepam (Valium) at 5 to 7.5 mg and clonazepam (Klonopin) at 0.5 to 1.5 mg, can be sedating and so are best used at bedtime for nocturnal spasms. They have addiction potential.
A third-line oral antispasticity option is dantrolene sodium, a direct-acting muscle relaxant [41]. It may be best for the nonambulatory patient with MS with severe spasticity who may be unaffected by the resultant weakness.
Back spasms in patients with MS may respond to cyclobenzaprine (Flexeril). Intractable spasticity may be managed with muscle or nerve blocks or intrathecal administration of baclofen (see the section on procedures).
Bladder dysfunction should be initially assessed with a urinalysis and urine culture to determine if a urinary tract infection is present. Appropriate antibiotics should be used for a urinary tract infection. If there is no infection or improvement after antibiotic treatment, a postvoid residual urine volume by ultrasound can help determine failure-to-empty (postvoid residual > 100 mL) or failure-to-store (postvoid residual < 100 mL) dysfunction [45]. A urodynamic study can help determine the presence (or absence) of detrusor hyperreflexia, detrusor-sphincter dyssynergia, or detrusor areflexia. Nonpharmacologic interventions for bladder dysfunction include timed voiding, minimizing the intake of bladder irritants such as caffeine, and regulation of fluid intake. Detrusor hyperactivity may respond to anticholinergic medications, such as the nonselective muscarinics oxybutynin (Ditropan), tolterodine (Detrol), trospium (Sanctura), and fesoterodine (Toviaz). Alternatively, the selective M2 and M3 antimuscarinics darifenacin (Enablex) and solifenacin (VESIcare) may be used [15]. The main side effects of the anticholinergics are dry mouth and constipation. Transdermal oxybutynin may offer even fewer side effects. Botulinum toxin type A injections into the detrusor muscle have shown efficacy in reducing symptoms in patients with detrusor hyperreflexia [46]. Detrusor underactivity is best managed with clean intermittent catheterization [45]. Cholinergic agents such as bethanechol (Urecholine) and tamsulosin may also reduce bladder urine volume [15]. Detrusor-sphincter dyssynergia may respond to a combination of clean intermittent catheterization and anticholinergic drugs [15]. Patients with MS and bladder dysfunction may eventually need continuous drainage by a suprapubic catheter. Urology consultation may be necessary for further workup and treatment in complicated cases that are not responding well to medications or for those patients requiring suprapubic catheterization. Surgical procedures may be necessary (see the section on surgery).
Sexual dysfunction in men with MS may be treated with oral medications such as sildenafil, vardenafil, and tadalafil if the problem is erectile dysfunction [47]. Intraurethral or penile injections of papaverine or alprostadil, mechanical vibrators, and vacuum devices can enhance arousal and orgasm [11,18]. Treatment of sexual dysfunction should include counseling and education [18,48]. Sildenafil may help improve lubrication in women with MS and sexual dysfunction [49].
Bowel dysfunction manifesting as constipation is best managed by establishment of a bowel program. This consists of adequate fluid intake, incorporation of fiber, adherence to a bowel elimination schedule, biofeedback, maintenance of physical activity, and judicious use of medications [15,18]. Fluid intake should be at least 8 cups each day. Fiber can be found in such foods as raw fruits and vegetables, whole grains, nuts, and seeds. Bowel elimination is most likely to occur shortly after a meal when the gastrocolic reflex results in an increase in the movement of intestinal contents; allow up to 30 minutes of uninterrupted time. Bulk formers, stool softeners, laxatives, rectal stimulants such as suppositories, or occasional use of enemas may be necessary. Diarrhea may be managed by bulk formers taken once per day without the extra fluid as in treatment of constipation. Medications such as loperamide, to slow bowel activity, may be necessary in patients with chronic diarrhea with fecal incontinence [18]. Workup should seek to eliminate other causes of diarrhea, such as Clostridium difficile infection or lactose intolerance.
Factors contributing to or mimicking fatigue should be ruled out or identified and addressed. Common factors are thyroid dysfunction, anemia, sleep disturbance, infections, and sedating medications [15,18]. Treatment should include nonpharmacologic [50] (Table 134.4) and, if necessary, pharmacologic interventions. First-line medications include amantadine [51,52] (Symmetrel), started at 100 mg in the morning and early afternoon, and modafinil [51] (Provigil), 100 to 400 mg in the morning. Pemoline (Cylert) and methylphenidate (Ritalin) are third-line medications [15]. Aspirin has been shown to improve fatigue in patients with MS [52].
Table 134.4
Nonpharmacologic Interventions for Management of Fatigue in Patients with Multiple Sclerosis
| Intervention | Method |
| Treat underlying factors that exacerbate fatigue | Correction of sleep disturbances Treatment of depression Reversal of thyroid abnormalities Management of medication adverse effects |
| Improve physical fitness | Aerobic exercise |
| Improve mobility | Physical and occupational therapy Instruction in proper use of mobility aids and techniques |
| Teach energy conservation | Timed rest periods Work simplification techniques |
| Teach cooling techniques | Avoidance of heat Use of cooling vests or other garments |
From Crayton HJ, Rossman HS. Managing the symptoms of multiple sclerosis: a multimodal approach. Clin Ther 2006;28:449.
The multiple pain syndromes in patients with MS are amenable to nonpharmacologic and pharmacologic interventions [11,53,54] (see Table 134.3).
Cognitive impairment can be detected during daily interactions with family, colleagues, and friends or during interactions with speech-language pathologists, physical therapists, and occupational therapists. Formal neuropsychological testing can determine the presence and severity of even subtle cognitive impairments [19]. Speech-language pathologists can teach compensatory techniques, such as repetition and maintaining a memory book. Donepezil was not shown to improve MS-related cognitive dysfunctions [55,56]. Identifying and treating depression with antidepressant medication and counseling can be helpful [32].
Acute visual deficits attributable to inflammation may improve more rapidly after high-dose intravenous administration of methylprednisolone. Prism lenses may help compensate for double vision. Regular patching should be avoided because this may prevent the brain from learning to compensate for double vision; patching can be limited to specific activities, such as watching television or reading.
Rehabilitation
Physical therapy interventions to decrease spasticity include range of motion exercises, stretching, positioning, aerobic exercise, and relaxation techniques [32].
The physical therapist may also improve mobility by training the patient to use various assistive devices to compensate for weakness and fatigue. The physical therapist may also use transcutaneous electrical nerve stimulation to assist with pain management. Physical therapists can teach aerobic exercises to prevent deconditioning, to improve endurance, and thus to delay or to minimize the effects of fatigue [35]. Weakness due to the “short circuiting” in demyelinated nerves, as can occur in MS, may be made worse if the patient exercises to the point of fatigue. Exercise programs should be individualized and updated as the patient’s condition changes [35]. Occupational therapists can help mitigate the effects of fatigue by teaching energy conservation and work simplification through the use of adaptive equipment and techniques.
Ataxia and tremor can be difficult symptoms to manage. Weighted utensils and weights on the distal limbs or assistive devices may lessen the effect of the tremor on a patient’s function [15]. Compensatory techniques taught by occupational therapy may improve activities of daily living. Medications for tremor may include beta blockers, buspirone, and clonazepam [15].
A speech-language pathologist can teach the patient techniques to improve speech intelligibility. Various oromotor exercises can help maintain oral muscle coordination [57]. Swallowing dysfunction should be evaluated with a videofluoroscopy study. The speech-language pathologist can also help determine the safest food texture for a patient with dysphagia [57]. Severe dysphagia may require placement of a gastrostomy tube for nutrition to be maintained [57].
A vocational rehabilitation counselor can play an important role in integrating the disabled MS patient back into the workforce.
Procedures
Muscle or nerve blocks should be reserved for patients with focal spasticity or generalized spasticity with a focal target, such as hip adductor spasticity that interferes with toileting. The most commonly used agents are botulinum toxin and phenol [41]. Intramuscular injection of botulinum toxin to specific muscles usually takes effect within a week, peaks in 2 to 3 weeks, and lasts 3 to 4 months. Side effects may include muscle weakness, atrophy, and diffusion to other muscles. The maximum recommended dose of botulinum toxin is 400 units at a minimum interval of 3 months [41,58]. Resistance may occur from development of neutralizing antibodies. The neurolytic effect from phenol usually lasts 3 to 12 months, and the injection can be repeated. Side effects of the procedure include local soreness, edema, and fibrosis. Intrathecal administration of phenol has been used in selected patients whose spasticity was resistant to conventional treatment [41].
Surgery
Intrathecal administration of baclofen from a pump implanted in the abdomen is a reasonable option when oral antispasticity medications or muscle and nerve blocks are not tolerated or effective [59]. In rare cases, severe spasticity may need to be treated with stereotactic radiosurgery or deep brain stimulation [60] and refractory tremors with deep brain stimulation [61,62], thalamic stimulation, or thalamotomy [61–63]. Trigeminal neuralgia may be amenable to gamma knife radiosurgery [64]. Augmentation cystoplasty may be an option in patients with detrusor hyperreflexia that is refractory to conservative treatments [65].
Potential Disease Complications
MS has the potential to progress in such a way as to render the patient severely disabled both physically and cognitively. Dysphagia may lead to aspiration pneumonia that can cause death. Cervical myelopathy or severe demyelination in the brainstem may lead to respiratory failure. Complications related to the relative immobility include pneumonia, deep venous thrombosis, pulmonary embolism, and decubitus ulcers. Neurogenic bladder may contribute to urinary tract infections and even urosepsis. In a sample population of MS patients, half the deaths were due to pneumonia, pulmonary embolism, aspiration, urosepsis, and decubitus ulcers; respiratory complications accounted for most of the deaths [66]. The other deaths were similar to those in the general population. There may be a higher incidence of suicide in patients with MS [67]. If suicides are excluded, the life expectancy of patients with MS may be 6 to 7 years less than that of the general population [68].
Potential Treatment Complications
Corticosteroids may cause myriad adverse effects, including osteoporosis, immunosuppression, edema, cataracts, glaucoma, avascular necrosis, and myopathy. Interferon beta-1b and beta-1a may result in influenza-like symptoms and injection site reactions. Continued use of interferons may lead to the development of antibodies, rendering them less effective [69]. Baclofen and other antispasticity medications can lead to weakness, drowsiness, and dizziness [41]. If oral or intrathecal baclofen is abruptly withdrawn, hallucinations or seizures may occur [41]. Medications such as opiates for severe pain and benzodiazepines for tremor and spasticity have abuse potential. Dantrolene or tizanidine for spasticity may result in hepatitis, and liver enzymes should be monitored especially during the first 4 months [21]. Antidepressants may contribute to sexual dysfunction.