CASE 133
History: A 24-year-old woman presents with nausea and diarrhea 52 days after bone marrow transplant for leukemia.
1. What should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
A. Graft-versus-host disease (GVHD)
2. What is the most common site of involvement with acute GVHD?
3. When does subacute GVHD occur?
A. Within 100 days after bone marrow transplant
B. In 1 to 4 months after bone marrow transplant
C. In 3 to 6 months after bone marrow transplant
D. In 3 to 12 months after bone marrow transplant
4. What is the most common site of GI tract chronic GVHD?
ANSWERS
CASE 133
Small Bowel Graft-Versus-Host Disease
1. A, B, C, and E
2. A
3. B
4. B
References
Coy DL, Ormazabal A, Godwin FD, et al: Imaging evaluation of pulmonary and abdominal complications following hematopoietic stem cell transplantation. Radiographics. 2005;25(2):305–318.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 125.
Comment
Transplant recipients face a variety of GI complications, which are typically related to the immunosuppressive drugs taken to prevent rejection. Peptic ulcer disease, bowel perforation, and opportunistic infections are common. Pancreatitis and hepatitis also occur more frequently in these patients. In patients who undergo bone marrow transplants for various diseases, other complications can occur in addition to those already mentioned. In the initial induction phase of therapy, during which the native bone marrow is destroyed, the patient receives high-dose radiation or chemotherapy. During this phase, acute enteritis with diarrhea, pain, and bleeding may develop because of the loss of mucosal cells lining the bowel. In the latter stages, the transplanted marrow (graft) may mount an immune response against the body (host), producing GVHD. This rejection typically occurs within the first few months of bone marrow transplant, although later development is possible.
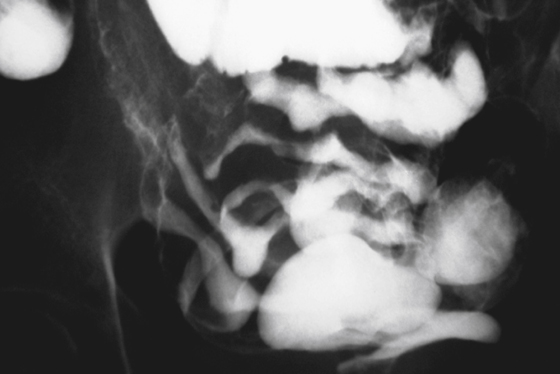
The major organs involved in GVHD include the skin, GI tract, lungs, and liver. Patients develop a diffuse rash, protein-losing diarrhea, and jaundice. Abnormalities encountered in the small bowel include fold thickening, which may progress to complete effacement of the folds; luminal narrowing; and separation of the bowel loops (see figure). Similar changes also may occur in the colon, resembling chronic ulcerative colitis. Pneumatosis of the bowel also has been reported. Gastric abnormalities include dilation and delayed gastric emptying. An unusual radiologic abnormality is prolonged barium coating of the mucosa. CT findings include bowel wall thickening, the “halo” sign caused by bowel wall edema, pericolic inflammation, and mesenteric thickening.