Antihistamines
ACTIONS
Competitively block the H1-receptor sites and impede histamine-mediated responses. Second-generation antihistamines cause less drowsiness.
USES
• Prevent and treat seasonal allergies, decrease itching and pruritis.
• Are adjunct with epinephrine for severe allergic reaction (anaphylaxis).
• Prevent and treat motion sickness.
PRECAUTIONS
• Asthma—acute or chronic; chronic obstructive pulmonary disease (COPD)
• Pregnancy and lactation; glaucoma
• Conditions resulting in urinary retention and obstruction
SIDE EFFECTS
• Benadryl: Includes **sedation, thickening of bronchial secretions, dry mouth, drowsiness, dizziness,** and muscular weakness.
• Zyrtec: May cause paradoxical reaction in children—restlessness, anxiety.
NURSING IMPLICATIONS
1. ‡Caution patient not to take antihistamines with alcohol.‡
2. diphenhydramine (Benadryl)—‡Caution patient about drowsiness because‡ of safety concerns.
3. Do not administer antihistamines within 4 days of skin testing.
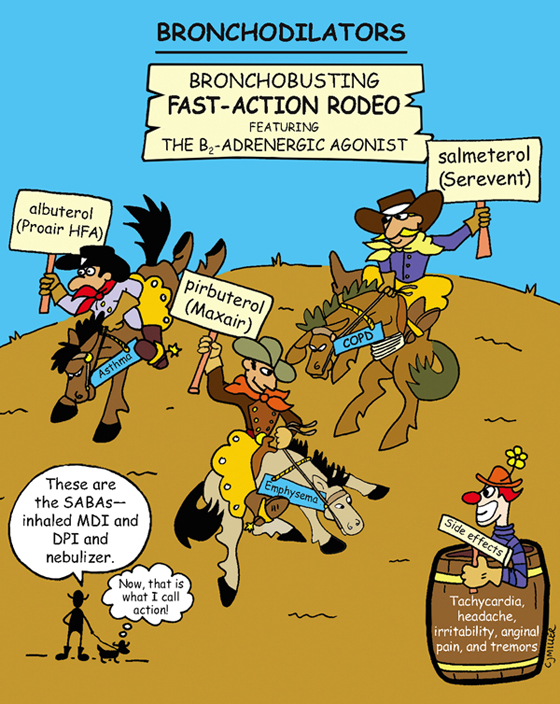
Bronchodilators
ACTIONS
Short-acting beta2 agonists (SABA) are selective adrenergic agonists. Sympathomimetic agents activate the beta2-receptors to relax the smooth muscles in the bronchioles, producing dilation.
USES
• Short-acting preparations to treat acute exacerbations of asthma
• Short-term relief of bronchoconstriction caused by bronchitis, emphysema, and asthma
• Prevention of exercise-induced bronchospasm (EIB)
SIDE EFFECTS
• **Headache, nausea, restlessness, nervousness, tremors**
• Increased blood pressure (BP), heartburn, insomnia, bronchial irritation
ADVERSE OR TOXIC EFFECTS (Excessive sympathomimetic stimulation)
• Palpitations, **tachycardia,** chest pain
• Slight increase in BP, followed by a drop in BP; diaphoresis
NURSING IMPLICATIONS
1. *Evaluate patient’s respiratory status and vital signs.*
2. ‡Explain to patient which type of medication is for long-term control and which one is for short-term response. Short-term preparations are used to treat and/or to prevent immediate problems; long-term preparations are given on a schedule for maintenance.‡
4. *Advise patient not to use more doses than ordered.*
5. Check with health care provider before using over-the-counter medicine.
6. ‡Teach patient the correct use of inhalation devices—metered-dose inhalers (MDI), dry powder inhalers (DPI), and nebulizers.‡
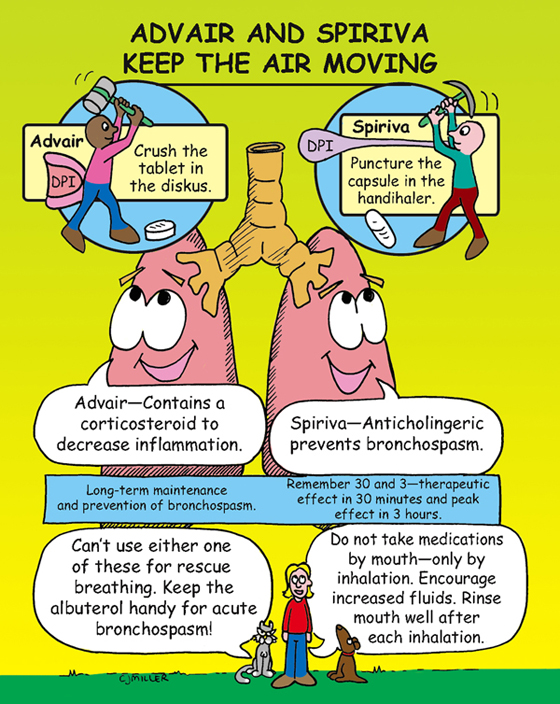
Advair and Spiriva
FLUTICASONE/SALMETEROL (ADVAIR)
Classification: Long-acting B2-agonist and glucocorticoid
Actions: Provides antiinflammatory and bronchodilator actions.
Dose: *Administered by Advair Diskus dry powder inhaler (DPI), 2 inhalations each morning and evening.*
TIOTROPIUM (SPIRIVA)
Classification: Anticholinergic bronchodilator
Actions: Blocks muscarinic (cholinergic) receptors in the lung. Therapeutic effects begin in approximately 30 minutes and peak in 3 hours.
Dose: *Administered by HandiHaler DPI, once daily.*
USES
• Long-term control and maintenance treatment for prevention of bronchospasm and airway inflammation associated with asthma, chronic bronchitis, and chronic obstructive pulmonary disease (COPD)
SIDE EFFECTS
• **Throat irritation, dry mouth**
• **Corticosteroids—increased incidence of oropharyngeal fungal infections**
NURSING IMPLICATIONS
1. *Medications are to be taken every day as directed, even on days when patients feel they are breathing better.*
2. *Medications are not for rescue in acute episodes.*
3. ‡Patients should carry a rescue inhaler, such as albuterol.‡
4. ‡Encourage patient to rinse mouth to decrease infection (Spiriva) and to decrease throat and mouth irritation.‡
6. ‡Medications must be taken with inhaler—capsules and tablets are not to be swallowed. Teach patients how to administer medication via a DPI.‡
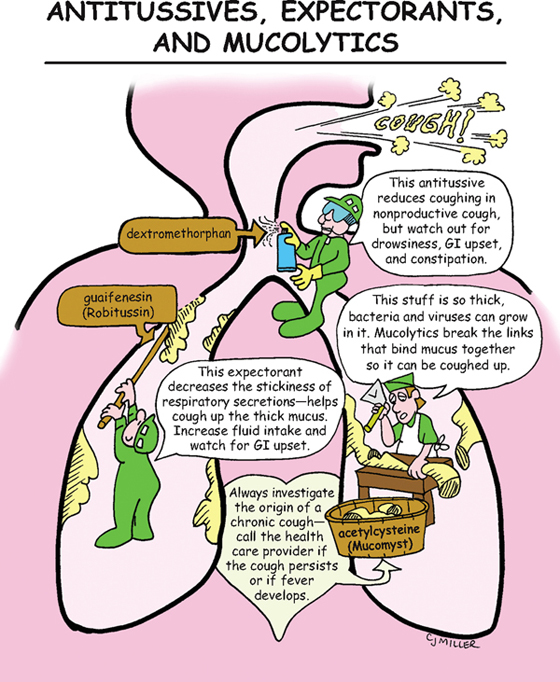
Antitussives, Expectorants, and Mucolytics
ACTION
Antitussives act either centrally (central nervous system [CNS]) or locally in the peripherally nervous system to decrease irritation and suppress the cough response. Expectorants decrease thickness of sputum and increase ease of the removal for a productive cough. Mucolytics disrupt the bond among proteins in respiratory secretions to liquefy the mucus.
USES
• Antitussives suppress persistent or nonproductive cough.
• Expectorants decrease viscosity and promote more productive cough.
• Mucolytics break down mucus and make cough more productive.
PRECAUTIONS
• Dextromethorphan is used in many over-the-counter (OTC) cough preparations.
• Origin of chronic cough should be investigated.
• Codeine is a very effective antitussive; is considered a Schedule V drug in cough medications.
SIDE EFFECTS
• Antitussives: Dextromethorphan—euphoria (may be abused); codeine—**drowsiness, constipation, gastrointestinal (GI) upset**
• Expectorants: nausea and vomiting, GI upset
• Mucolytics: nausea, rhinorrhea, bronchospasms, dizziness
NURSING IMPLICATIONS
1. *Evaluate patient’s respiratory status and response to medication.*
2. ‡Warn patient to avoid driving and operating machinery when taking codeine cough suppressant.‡
3. Mucomyst has a short-term disagreeable odor (rotten eggs).
4. ‡Teach patient to read labels; is frequently combined with other drugs in cold and flu preparations.‡