Procedure 13 In Situ Cubital Tunnel Decompression
![]() See Video 11: In Situ Cubital Tunnel Decompression
See Video 11: In Situ Cubital Tunnel Decompression
Indications
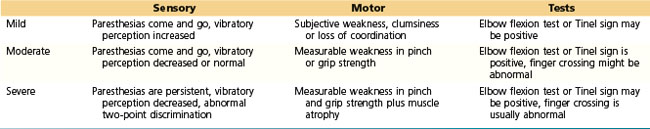
 In situ decompression of the ulnar nerve is indicated for patients with symptoms that are mild or intermittent (Table 13-1). If there is subluxation or instability of the ulnar nerve and/or ulnar nerve palsy owing to an abnormal osseous architecture of the elbow, in situ decompression is not indicated. In these situations, an anterior transposition is more appropriate to correct the anatomic problem.
In situ decompression of the ulnar nerve is indicated for patients with symptoms that are mild or intermittent (Table 13-1). If there is subluxation or instability of the ulnar nerve and/or ulnar nerve palsy owing to an abnormal osseous architecture of the elbow, in situ decompression is not indicated. In these situations, an anterior transposition is more appropriate to correct the anatomic problem.
Examination/Imaging
Clinical Examination
 Palpation: The ulnar nerve is palpated to check for enlargement or subluxation.
Palpation: The ulnar nerve is palpated to check for enlargement or subluxation.
 The elbow joint is checked for range of motion.
The elbow joint is checked for range of motion.
 Check Tinel sign from the distal forearm to above the elbow along the course of the ulnar nerve. In cubital tunnel syndrome, Tinel sign is present at the medial epicondylar groove or over the proximal end of the flexor carpi ulnaris (FCU) muscle.
Check Tinel sign from the distal forearm to above the elbow along the course of the ulnar nerve. In cubital tunnel syndrome, Tinel sign is present at the medial epicondylar groove or over the proximal end of the flexor carpi ulnaris (FCU) muscle.
 A provocative test for ulnar nerve subluxation is performed by placing the elbow in full flexion with the wrist hyperextended, whereas manual pressure is applied to the nerve for 60 seconds. If the patient’s ring and small finger become numb, the ulnar nerve is likely compressed.
A provocative test for ulnar nerve subluxation is performed by placing the elbow in full flexion with the wrist hyperextended, whereas manual pressure is applied to the nerve for 60 seconds. If the patient’s ring and small finger become numb, the ulnar nerve is likely compressed.
 Intrinsic muscle function is tested by asking the patient to cross the long finger over the index finger (i.e., the crossed finger test). Patients with severe ulnar nerve entrapment will not be able to perform this task.
Intrinsic muscle function is tested by asking the patient to cross the long finger over the index finger (i.e., the crossed finger test). Patients with severe ulnar nerve entrapment will not be able to perform this task.
Imaging
 Radiographs of the elbow may be obtained if elbow pathology is suspected, such as valgus cubitus, bone spurs or fragments, a shallow epicondylar groove, osteochondroma, and/or destructive lesions. In most cases of idiopathic ulnar nerve entrapment, however, radiographs are not necessary.
Radiographs of the elbow may be obtained if elbow pathology is suspected, such as valgus cubitus, bone spurs or fragments, a shallow epicondylar groove, osteochondroma, and/or destructive lesions. In most cases of idiopathic ulnar nerve entrapment, however, radiographs are not necessary.
 Electromyography tests and nerve conduction studies are indicated to confirm the area of entrapment and to document the extent of the pathology.
Electromyography tests and nerve conduction studies are indicated to confirm the area of entrapment and to document the extent of the pathology.
 Nerve conduction studies showing a diminished signal conduction rate of less than 50 meters per second (33% decrease from normal) across the elbow are indicative of nerve compression.
Nerve conduction studies showing a diminished signal conduction rate of less than 50 meters per second (33% decrease from normal) across the elbow are indicative of nerve compression.
Surgical Anatomy
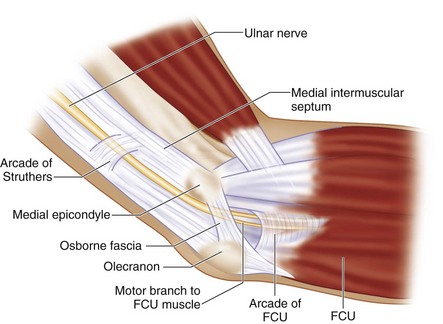
 The ulnar nerve is the terminal branch of the medial cord of the brachial plexus. Initially, the ulnar nerve lies medial to the axillary artery. In the upper arm, the ulnar nerve lies posteromedial to the brachial artery, posterior to the intermuscular septum, and anterior to the medial head of the triceps muscle. Approximately 8 cm proximal to the medial epicondyle is the arcade of Struthers, a thin fibrous band. At the elbow, the ulnar nerve travels posterior to the medial epicondyle and medial to the olecranon at the subcutaneous level, then it enters the cubital tunnel. The cubital tunnel is covered by fibroaponeurotic bands and the Osborne fascia (a ligament over the epicondylar groove), which is the fibroaponeurotic tissue between the two heads of the FCU. After passing through the cubital tunnel, the ulnar nerve travels deep into the forearm between the humeral and ulnar heads of the FCU. Distally, the ulnar nerve follows through the FCU to the deep flexor-pronator aponeurosis (Fig. 13-1).
The ulnar nerve is the terminal branch of the medial cord of the brachial plexus. Initially, the ulnar nerve lies medial to the axillary artery. In the upper arm, the ulnar nerve lies posteromedial to the brachial artery, posterior to the intermuscular septum, and anterior to the medial head of the triceps muscle. Approximately 8 cm proximal to the medial epicondyle is the arcade of Struthers, a thin fibrous band. At the elbow, the ulnar nerve travels posterior to the medial epicondyle and medial to the olecranon at the subcutaneous level, then it enters the cubital tunnel. The cubital tunnel is covered by fibroaponeurotic bands and the Osborne fascia (a ligament over the epicondylar groove), which is the fibroaponeurotic tissue between the two heads of the FCU. After passing through the cubital tunnel, the ulnar nerve travels deep into the forearm between the humeral and ulnar heads of the FCU. Distally, the ulnar nerve follows through the FCU to the deep flexor-pronator aponeurosis (Fig. 13-1).
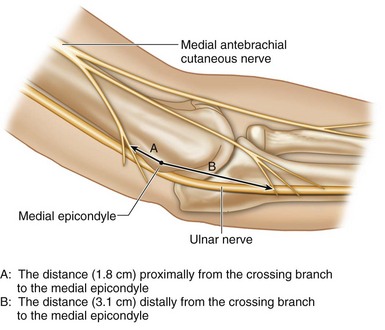
 The posterior branch of the medial antebrachial cutaneous nerve is at risk of injury during cubital tunnel surgery. The proximal crossing branch lies approximately 1.8 cm proximal to the medial epicondyle, whereas the distal crossing branch is about 3.1 cm distal to the medial epicondyle (Fig. 13-2).
The posterior branch of the medial antebrachial cutaneous nerve is at risk of injury during cubital tunnel surgery. The proximal crossing branch lies approximately 1.8 cm proximal to the medial epicondyle, whereas the distal crossing branch is about 3.1 cm distal to the medial epicondyle (Fig. 13-2).
 The ulnar nerve may be easily compressed at five sites (see Fig. 13-1).
The ulnar nerve may be easily compressed at five sites (see Fig. 13-1).
 The most common sites of ulnar nerve compression are the epicondylar groove and the cubital tunnel.
The most common sites of ulnar nerve compression are the epicondylar groove and the cubital tunnel.
Positioning
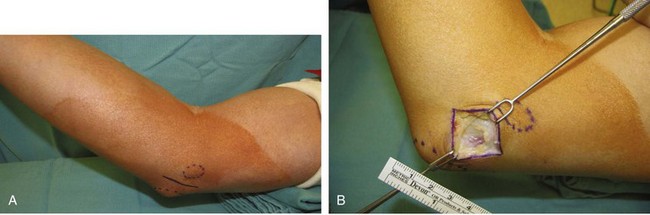
 The procedure is performed under tourniquet control. It can be done under regional or general anesthesia. The patient is positioned supine with the affected extremity on a hand table. The elbow is in 90-degree flexion, with some towels under the elbow to keep the elbow in flexion and supination posture. Placing these towels under the elbow will help in locating the medial epicondyle (Fig. 13-3).
The procedure is performed under tourniquet control. It can be done under regional or general anesthesia. The patient is positioned supine with the affected extremity on a hand table. The elbow is in 90-degree flexion, with some towels under the elbow to keep the elbow in flexion and supination posture. Placing these towels under the elbow will help in locating the medial epicondyle (Fig. 13-3).
Exposures
Procedure
Step 1
Step 2
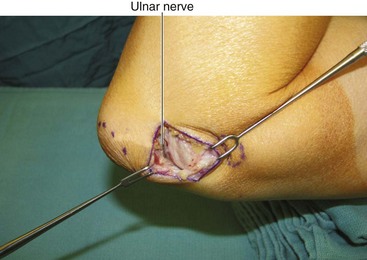
 After Osborne fascia release, the ulnar nerve is identified (Fig. 13-6).
After Osborne fascia release, the ulnar nerve is identified (Fig. 13-6).
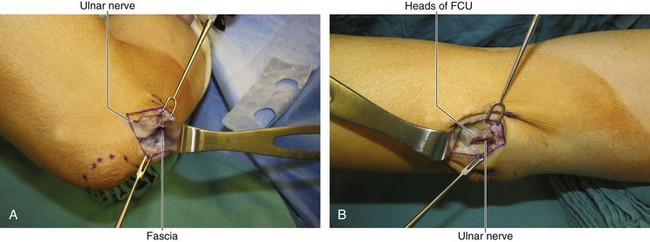
 The skin is retracted proximally and distally at the medial epicondyle. The tightened fascia over the ulnar nerve can be checked using scissors; if the fascia is tight, it may be divided with scissors (Fig. 13-7A and B).
The skin is retracted proximally and distally at the medial epicondyle. The tightened fascia over the ulnar nerve can be checked using scissors; if the fascia is tight, it may be divided with scissors (Fig. 13-7A and B).
 Distally, the muscle bellies of the FCU should be released if ulnar nerve compression is discovered.
Distally, the muscle bellies of the FCU should be released if ulnar nerve compression is discovered.
Step 2 Pearls
The ulnar nerve is secured in its groove with areolar tissue and longitudinal feeding blood vessels. Freeing this areolar tissue will cause ulnar nerve subluxation. Only the compressive fascia band needs to be released, whereas the supporting soft tissue posterior to the ulnar nerve should not be disturbed.
Step 3
 The elbow is moved through a range of movements to check whether the ulnar nerve subluxes.
The elbow is moved through a range of movements to check whether the ulnar nerve subluxes.
 If subluxation of the ulnar nerve over the medial epicondyle is noticed, medial epicondylectomy or anterior transposition of the ulnar nerve should be performed to avoid postoperative discomfort from nerve impingement.
If subluxation of the ulnar nerve over the medial epicondyle is noticed, medial epicondylectomy or anterior transposition of the ulnar nerve should be performed to avoid postoperative discomfort from nerve impingement.
Postoperative Care and Expected Outcomes
 The dressings are removed 2 to 3 days after surgery, and active range of motion of the elbow is started at that time.
The dressings are removed 2 to 3 days after surgery, and active range of motion of the elbow is started at that time.
 In mild to moderate nerve compression, the in situ decompression procedure should result in marked relief of paresthesias in the ulnar nerve distribution. The motor weakness may take a much longer time to recover.
In mild to moderate nerve compression, the in situ decompression procedure should result in marked relief of paresthesias in the ulnar nerve distribution. The motor weakness may take a much longer time to recover.
Miller RG, Hummel EE. The cubital tunnel syndrome: treatment with simple decompression. Ann Neurol. 1980;7:567-569.
Nathan PA, Istvan JA, Meadows KD. Intermediate and long-term outcomes following simple decompression of the ulnar nerve at the elbow. Chir Main. 2005;24:29-34.
Tanigughi Y, Takami M, Tamake T, et al. Simple decompression with small skin incision for cubital tunnel syndrome. J Hand Surg [Br]. 2002;27:559-562.