Procedure 13 Cervical Pedicle Screw Fixation
Overview
 Despite increasing acceptance of the use of pedicle screws in the lumbar and thoracic spine, screw insertion into the cervical pedicle has been considered by spine surgeons to be too risky for the neurovascular structures, except at C2 and C7. Leconte first reported C2 pedicle screw insertion for osteosynthesis of the C2 hangman’s fracture. In the late 1980s, Goel and Laheri started to use C2 pedicle screws for atlantoaxial plate fixation in combination with C1 lateral mass screws. However, there had been no reports of pedicle screw fixation from C3 to C6 until the 1994 report by Abumi and colleagues of pedicle screw fixation for traumatic lesions of the lower cervical spine. Biomechanical studies revealed the superior stabilizing effect of pedicle screw fixation compared with other internal fixation procedures used with the cervical spine, including lateral mass screw fixation. In their recent experimental study, Johnston and colleagues revealed the superior pullout strength of a cervical pedicle screw versus a lateral mass screw after repetitive loading. Dunlop and colleagues demonstrated, by an in-vitro biomechanical study, that cervical pedicle screw/rod constructs support a greater axial load than lateral mass screw/rod constructs.
Despite increasing acceptance of the use of pedicle screws in the lumbar and thoracic spine, screw insertion into the cervical pedicle has been considered by spine surgeons to be too risky for the neurovascular structures, except at C2 and C7. Leconte first reported C2 pedicle screw insertion for osteosynthesis of the C2 hangman’s fracture. In the late 1980s, Goel and Laheri started to use C2 pedicle screws for atlantoaxial plate fixation in combination with C1 lateral mass screws. However, there had been no reports of pedicle screw fixation from C3 to C6 until the 1994 report by Abumi and colleagues of pedicle screw fixation for traumatic lesions of the lower cervical spine. Biomechanical studies revealed the superior stabilizing effect of pedicle screw fixation compared with other internal fixation procedures used with the cervical spine, including lateral mass screw fixation. In their recent experimental study, Johnston and colleagues revealed the superior pullout strength of a cervical pedicle screw versus a lateral mass screw after repetitive loading. Dunlop and colleagues demonstrated, by an in-vitro biomechanical study, that cervical pedicle screw/rod constructs support a greater axial load than lateral mass screw/rod constructs.
 The pedicle screw fixation procedure allows rigid fixation that provides the high correction capability needed to restore physiologic sagittal alignment of the cervical spine, as well as sufficient correction of malalignment in the occipitoatolantoaxial region. In addition, the pedicle screw fixation procedure, which does not require use of the lamina for stabilization, is quite valuable in patients who undergo one-stage posterior cervical decompression and stabilization, and in patients who undergo posterior reconstruction after previous posterior cervical decompression. On the other hand, the risks of neurovascular complications caused by inadequate screw placement into the cervical pedicle cannot be completely obviated. Thorough knowledge of local anatomy, sufficient preoperative radiologic examinations, and the application of established surgical techniques are essential for this procedure.
The pedicle screw fixation procedure allows rigid fixation that provides the high correction capability needed to restore physiologic sagittal alignment of the cervical spine, as well as sufficient correction of malalignment in the occipitoatolantoaxial region. In addition, the pedicle screw fixation procedure, which does not require use of the lamina for stabilization, is quite valuable in patients who undergo one-stage posterior cervical decompression and stabilization, and in patients who undergo posterior reconstruction after previous posterior cervical decompression. On the other hand, the risks of neurovascular complications caused by inadequate screw placement into the cervical pedicle cannot be completely obviated. Thorough knowledge of local anatomy, sufficient preoperative radiologic examinations, and the application of established surgical techniques are essential for this procedure.
Indications
 Almost all the pathologic conditions requiring posterior stabilization of the occipitocervical junction, cervical spine, or cervicothoracic junction.
Almost all the pathologic conditions requiring posterior stabilization of the occipitocervical junction, cervical spine, or cervicothoracic junction.
 Most middle and lower cervical injuries with posterior disruption, or anterior and posterior disruption without a severely disrupted anterior column, can be managed by posterior surgery using cervical pedicle screw fixation alone.
Most middle and lower cervical injuries with posterior disruption, or anterior and posterior disruption without a severely disrupted anterior column, can be managed by posterior surgery using cervical pedicle screw fixation alone.
 Cervical spinal instability caused by nontraumatic lesions, including metastatic tumor, rheumatoid arthritis, destructive spondyloarthropathy, cervical intervention for posterior decompression of the spinal cord or nerve root, and so forth, are well managed by this procedure.
Cervical spinal instability caused by nontraumatic lesions, including metastatic tumor, rheumatoid arthritis, destructive spondyloarthropathy, cervical intervention for posterior decompression of the spinal cord or nerve root, and so forth, are well managed by this procedure.
 Cervical kyphosis caused by many causes, including postlaminectomy and posttraumatic kyphosis, cervical spondylotic myelopathy associated with kyphosis, and so forth, can be corrected sufficiently by this procedure.
Cervical kyphosis caused by many causes, including postlaminectomy and posttraumatic kyphosis, cervical spondylotic myelopathy associated with kyphosis, and so forth, can be corrected sufficiently by this procedure.
 A degenerative cervical spine with segmental instability requiring posterior decompression also can be managed by simultaneous decompression and stabilization using pedicle screw fixation.
A degenerative cervical spine with segmental instability requiring posterior decompression also can be managed by simultaneous decompression and stabilization using pedicle screw fixation.
 This procedure is beneficial for stabilization of the unstable motion segment caused by extensive decompression of the nerve root or spinal cord, affecting stability of the facet joint.
This procedure is beneficial for stabilization of the unstable motion segment caused by extensive decompression of the nerve root or spinal cord, affecting stability of the facet joint.
 Salvage of pseudarthrosis of anterior fusion.
Salvage of pseudarthrosis of anterior fusion.
 Fusion-level elongation for adjacent segment degeneration after anterior or posterior fusion surgery.
Fusion-level elongation for adjacent segment degeneration after anterior or posterior fusion surgery.
Indications Pitfalls
• Infectious disorders at the posterior portion of the cervical spine are contraindications for pedicle screw fixation.
• Pedicles destroyed by injuries, tumors, rheumatoid arthritis
• Pedicles of the vertebra associated with major anomalies of the vertebral artery, and so forth, are inadequate and risky for screw insertion (Figures 13-1 and 13-2).
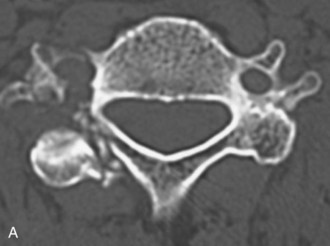
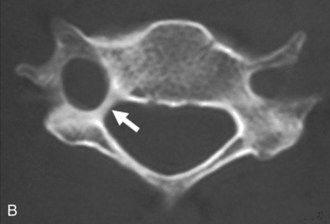
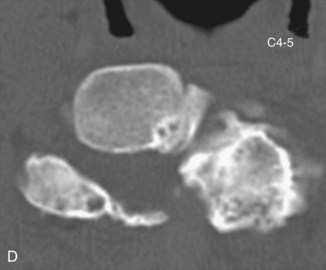
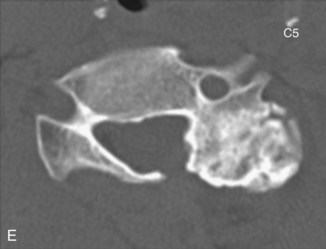
• Figure 13-1 shows an abnormal condition of the cervical pedicle. Pedicles destroyed by injuries, tumors, or marked osteoporosis; extremely small pedicles; pedicles of the vertebrae associated with major anomalies of the vertebral artery, and so forth, are inadequate and risky for screw insertion. Figure 13-1, A shows a fracture of the pedicle in a patient with a lateral mass fracture. Figure 13-2, B shows a pedicle of an extremely small size in a patient with rheumatoid arthritis.
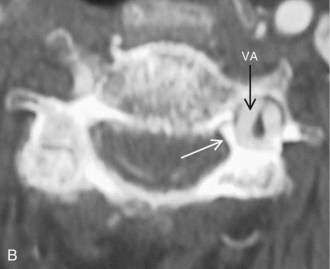
• Figure 13-2 shows a small size of the pedicle of the axis. Figure 13-2, A shows that the diameter of right side of the pedicle of the axis is too small for screw insertion by high-riding vertebral artery bends into the lateral mass of the axis (arrow). Figure 13-2, B shows extremely small pedicles of the axis for screw insertion.
• Patients sometimes have extreme unilateral dominance of the vertebral artery. In this condition, the dominant-side foramen transversarium enlarges, and the ipsilateral side of the pedicle decreases in size (Figure 13-3). Retrogression of the pedicle is found on the side of the dominant vertebral artery. Figure 13-3, A shows that patients sometimes show extreme right-left dominance of the vertebral artery. Figure 13-3, B shows that the dominant side of the foramen transversarium enlarges and that the ipsilateral side of the pedicle decreases in size (white arrow).
• For the patient with unilateral obstruction of the vertebral artery by injury, tumor, congenital anomaly, and so forth, screw insertion on the preserved artery side must be conducted with great care, or screw insertion should only be performed on the obstructed side.
Examination/Imaging
 Preoperative oblique-projection plain radiograph films are valuable for evaluation of the pedicle size. In an oblique projection, the contralateral pedicle is seen as an oval projected onto the vertebral body, showing the outer and inner diameter of the pedicle. If the projection shows no inner diameter, the pedicle does not have a medullary canal.
Preoperative oblique-projection plain radiograph films are valuable for evaluation of the pedicle size. In an oblique projection, the contralateral pedicle is seen as an oval projected onto the vertebral body, showing the outer and inner diameter of the pedicle. If the projection shows no inner diameter, the pedicle does not have a medullary canal.
 Computerized tomography (CT) evaluations (adjusted to the bone windows) are essential to assess the pedicle morphometry and to determine pedicle size, which allows surgeons to choose the appropriate pedicle screw diameter, length, direction in the coronal plane, and screw insertion point. Reconstructive CT in the oblique plane provides useful information about the size of the neural foramen.
Computerized tomography (CT) evaluations (adjusted to the bone windows) are essential to assess the pedicle morphometry and to determine pedicle size, which allows surgeons to choose the appropriate pedicle screw diameter, length, direction in the coronal plane, and screw insertion point. Reconstructive CT in the oblique plane provides useful information about the size of the neural foramen.
 Preoperative evaluation of the morphology of the vertebral artery is important in preventing serious complications involving the artery.
Preoperative evaluation of the morphology of the vertebral artery is important in preventing serious complications involving the artery.
Surgical Anatomy
 According to previous studies by Panjabi and colleagues and by Karaikovic and colleagues, the pedicle of the cervical spine in a normal population has a sufficient diameter to allow insertion of a screw with a diameter of 3.5 mm or more.
According to previous studies by Panjabi and colleagues and by Karaikovic and colleagues, the pedicle of the cervical spine in a normal population has a sufficient diameter to allow insertion of a screw with a diameter of 3.5 mm or more.
 According to an anatomic study by Reinhold and colleagues, the average overall angle between the sagittal plane and the longitudinal pedicle axis was 46 degrees, varying from 30 degrees to 62 degrees. The smallest angle was at C7, the largest at C4. Their results were similar to previous studies by Karaikovic and colleagues.
According to an anatomic study by Reinhold and colleagues, the average overall angle between the sagittal plane and the longitudinal pedicle axis was 46 degrees, varying from 30 degrees to 62 degrees. The smallest angle was at C7, the largest at C4. Their results were similar to previous studies by Karaikovic and colleagues.
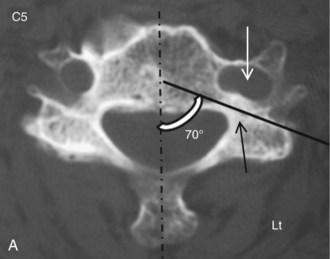
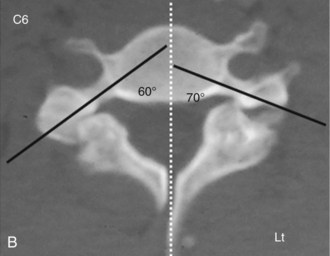
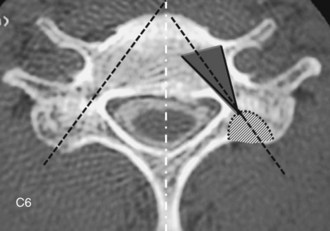
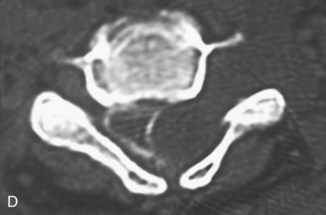
 Pedicle screw insertion into a vertebra with an extremely large angle between the pedicle axis and the sagittal plane may be possible but puts the vertebral artery and the spinal cord at risk. Figure 13-4 shows an extremely large angle between the pedicle axis and the sagittal plane. The left side of the foramen transversarium is enlarged toward the vertebral body (Figure 13-4, A, open arrow), and the angle between the pedicle axis (black line) and the sagittal plane is extremely large because of deformation of the foramen. In a case of C6 spondylolysis, the angle between the pedicle axis (Figure 13-4, B, black line) and the sagittal plane is extremely large. Screw insertion into the left side of the pedicle is too risky for the vertebral artery and the spinal cord.
Pedicle screw insertion into a vertebra with an extremely large angle between the pedicle axis and the sagittal plane may be possible but puts the vertebral artery and the spinal cord at risk. Figure 13-4 shows an extremely large angle between the pedicle axis and the sagittal plane. The left side of the foramen transversarium is enlarged toward the vertebral body (Figure 13-4, A, open arrow), and the angle between the pedicle axis (black line) and the sagittal plane is extremely large because of deformation of the foramen. In a case of C6 spondylolysis, the angle between the pedicle axis (Figure 13-4, B, black line) and the sagittal plane is extremely large. Screw insertion into the left side of the pedicle is too risky for the vertebral artery and the spinal cord.
 Karaikovic and colleagues defined the inner morphology of the cervical pedicles. They revealed that the thinnest pedicle cortex was always the lateral cortex, and some pedicles had no medullary canal (i.e., where solid cortical bone is expected: 0.9% for C2, 2.8% for C3 and C4, and 3.8% for C5 pedicles).
Karaikovic and colleagues defined the inner morphology of the cervical pedicles. They revealed that the thinnest pedicle cortex was always the lateral cortex, and some pedicles had no medullary canal (i.e., where solid cortical bone is expected: 0.9% for C2, 2.8% for C3 and C4, and 3.8% for C5 pedicles).
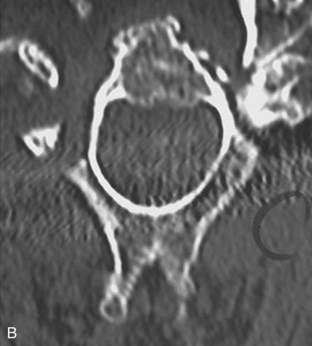
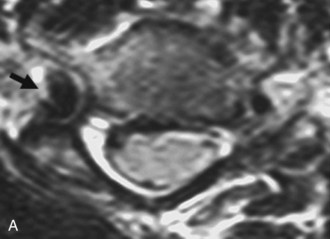
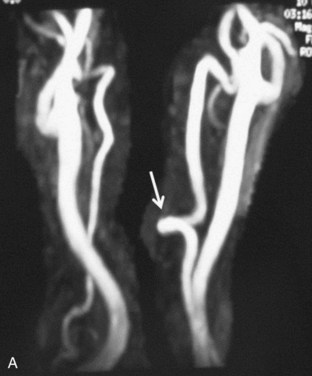
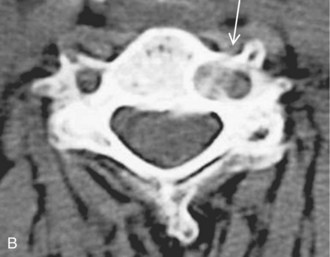
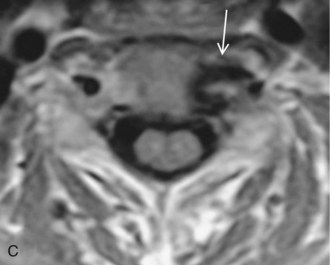
 The vertebral artery sometimes bends into the vertebral body forming the loop, and screw insertion into the ipsilateral side of the pedicle may put the artery at risk. Figure 13-5 shows loop formation of the vertebral artery.
The vertebral artery sometimes bends into the vertebral body forming the loop, and screw insertion into the ipsilateral side of the pedicle may put the artery at risk. Figure 13-5 shows loop formation of the vertebral artery.
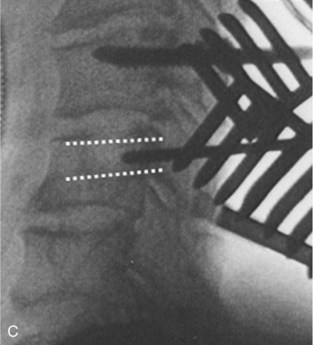
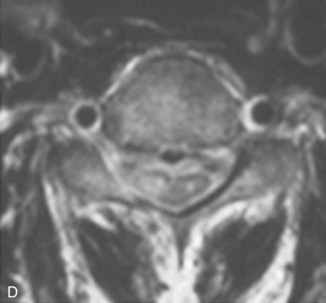
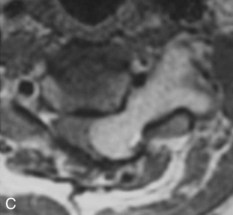
 MRA shows the medial loop of the left vertebral artery (Figure 13-5, A, arrow).
MRA shows the medial loop of the left vertebral artery (Figure 13-5, A, arrow).
 CT (Figure 13-5, B) and MRI (Figure 13-5, C) images show that the vertebral artery bends into the vertebral body, forming the loop (arrows). Screw insertion into the left side of the pedicle is too risky for the artery.
CT (Figure 13-5, B) and MRI (Figure 13-5, C) images show that the vertebral artery bends into the vertebral body, forming the loop (arrows). Screw insertion into the left side of the pedicle is too risky for the artery.
Positioning
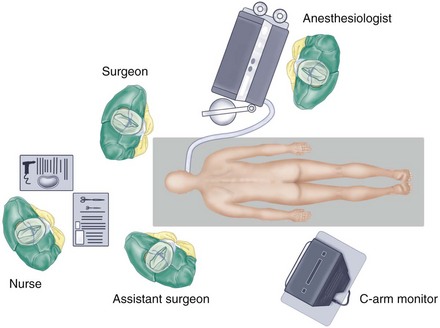
 The authors prefer to stand at the head of the patient, to ensure symmetric insertion of the right and left screws, while the assistant for a right-handed surgeon usually stands on the left side of the patient.
The authors prefer to stand at the head of the patient, to ensure symmetric insertion of the right and left screws, while the assistant for a right-handed surgeon usually stands on the left side of the patient.
 The C-arm display is placed on the left side of the patient near the patient’s pelvis for easy viewing by the surgeon. The authors’ preferred operation room setup for posterior cervical spinal procedures is shown in Figure 13-6.
The C-arm display is placed on the left side of the patient near the patient’s pelvis for easy viewing by the surgeon. The authors’ preferred operation room setup for posterior cervical spinal procedures is shown in Figure 13-6.
 The patient is placed prone on a Relton-Hall frame, using a horseshoe-type headrest or a Mayfield headholder.
The patient is placed prone on a Relton-Hall frame, using a horseshoe-type headrest or a Mayfield headholder.
 The shoulders are pulled caudally using heavy bandage for intraoperative lateral fluoroscopic imaging of the lower cervical spine.
The shoulders are pulled caudally using heavy bandage for intraoperative lateral fluoroscopic imaging of the lower cervical spine.
Portals/Exposures
 A skin incision is made, usually longer than that required for a standard spinous process wiring. The cephalad adjacent lamina of the most cephalad-fixed vertebra should entirely be exposed, taking care to protect the surrounding facet joint capsule. The paravertebral muscles are dissected laterally to expose the lateral margins of the articular masses for exact mediolateral determination of the screw insertion point.
A skin incision is made, usually longer than that required for a standard spinous process wiring. The cephalad adjacent lamina of the most cephalad-fixed vertebra should entirely be exposed, taking care to protect the surrounding facet joint capsule. The paravertebral muscles are dissected laterally to expose the lateral margins of the articular masses for exact mediolateral determination of the screw insertion point.
Procedure
Step 1: Manual Screw Placement
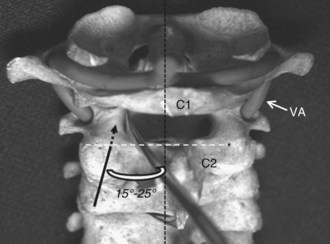
 The cranial margin of the C2 lamina is the craniocaudal landmark for the screw insertion point for C2. To confirm the screw insertion points in C2, a small spatula can be inserted into the spinal canal along the cranial margin of the C2 lamina to the medial surface of the C2 pedicle. Figure 13-7 shows the pedicle screw insertion point for C2. The cranial margin of the C2 lamina (white broken line) is the landmark for the screw insertion point for C2 (asterisk). To confirm the screw insertion points in C2, a small spatula can be inserted into the spinal canal along the margin cortex of the C2 pars interarticularis to the medial surface of the C2 pedicle. The black broken arrow indicates the screw direction toward the C2 pedicle.
The cranial margin of the C2 lamina is the craniocaudal landmark for the screw insertion point for C2. To confirm the screw insertion points in C2, a small spatula can be inserted into the spinal canal along the cranial margin of the C2 lamina to the medial surface of the C2 pedicle. Figure 13-7 shows the pedicle screw insertion point for C2. The cranial margin of the C2 lamina (white broken line) is the landmark for the screw insertion point for C2 (asterisk). To confirm the screw insertion points in C2, a small spatula can be inserted into the spinal canal along the margin cortex of the C2 pars interarticularis to the medial surface of the C2 pedicle. The black broken arrow indicates the screw direction toward the C2 pedicle.
 The angle for the C2 pedicle should be 15 to 25 degrees medial to the midline in the transverse plane.
The angle for the C2 pedicle should be 15 to 25 degrees medial to the midline in the transverse plane.
 The screw insertion points for the C3 to C7 pedicles are slightly lateral to the center of the articular mass and close to the inferior margin of the inferior articular process of the cranially adjacent vertebra. However, the shape and size of the lateral mass are variable in each vertebra and in each patient.
The screw insertion points for the C3 to C7 pedicles are slightly lateral to the center of the articular mass and close to the inferior margin of the inferior articular process of the cranially adjacent vertebra. However, the shape and size of the lateral mass are variable in each vertebra and in each patient.
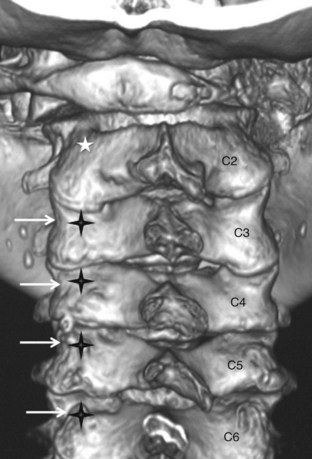
 The lateral margin of the articular mass of the cervical spine has a notch approximately at the level of the pedicle. The pedicles are located approximately below the lateral vertebral notch at C2, at the notch at C3 through C6, and at or slightly above the notch at C7. Figure 13-8 shows the pedicle screw insertion points for C3 to C7. Three-dimensional CT reconstruction shows the screw insertion points for C3 to C7. The lateral margin of the articular mass of the cervical spine has a notch approximately at the level of the pedicle (white arrow). The pedicles are located approximately below the lateral vertebral notch at C2, at C3 to C6, and at or slightly above the notch at C7. Screw insertion points (black crosses) are 2 to 4 mm medial to the notch. The white asterisk shows the C2 pedicle screw insertion point.
The lateral margin of the articular mass of the cervical spine has a notch approximately at the level of the pedicle. The pedicles are located approximately below the lateral vertebral notch at C2, at the notch at C3 through C6, and at or slightly above the notch at C7. Figure 13-8 shows the pedicle screw insertion points for C3 to C7. Three-dimensional CT reconstruction shows the screw insertion points for C3 to C7. The lateral margin of the articular mass of the cervical spine has a notch approximately at the level of the pedicle (white arrow). The pedicles are located approximately below the lateral vertebral notch at C2, at C3 to C6, and at or slightly above the notch at C7. Screw insertion points (black crosses) are 2 to 4 mm medial to the notch. The white asterisk shows the C2 pedicle screw insertion point.
 The thinnest pedicle cortex is always the lateral cortex. Therefore the surgeon should keep this in mind while probing and tapping the pedicle and while placing the screws.
The thinnest pedicle cortex is always the lateral cortex. Therefore the surgeon should keep this in mind while probing and tapping the pedicle and while placing the screws.
 The medial pedicle cortex must be used as a safe guide for the insertion of the screw into the vertebral body through the pedicle isthmus.
The medial pedicle cortex must be used as a safe guide for the insertion of the screw into the vertebral body through the pedicle isthmus.
 Use of a drill bit cannot be recommended to penetrate the cortex of the lateral mass or to make a hole for screw advancement. However, the neurocentral junction in the cervical spine, which is near the base of the pedicle in the vertebral body, is sometimes hard to pass with the pedicle probe, because it is in the thoracic and lumbar spine. In such cases, the junction can be perforated with a Kirschner wire or with small-sized high-speed diamond burr to make the path for the pedicle probe into the vertebral body.
Use of a drill bit cannot be recommended to penetrate the cortex of the lateral mass or to make a hole for screw advancement. However, the neurocentral junction in the cervical spine, which is near the base of the pedicle in the vertebral body, is sometimes hard to pass with the pedicle probe, because it is in the thoracic and lumbar spine. In such cases, the junction can be perforated with a Kirschner wire or with small-sized high-speed diamond burr to make the path for the pedicle probe into the vertebral body.
 The intended angle of screw insertion in the sagittal plane is parallel to the upper end plate for the pedicles of C5 to C7, and it is slightly in the cephalad direction for C2 to C4 (based on angulation in the sagittal plane). The C2 screw usually is perpendicular to the anterior surface of the vertebral body.
The intended angle of screw insertion in the sagittal plane is parallel to the upper end plate for the pedicles of C5 to C7, and it is slightly in the cephalad direction for C2 to C4 (based on angulation in the sagittal plane). The C2 screw usually is perpendicular to the anterior surface of the vertebral body.
Computer-Assisted Screw Placement
 Modern technology for computer navigation systems has been developing in the field of cervical spine surgery.
Modern technology for computer navigation systems has been developing in the field of cervical spine surgery.
 Kim and colleagues and Ludwig and colleagues conducted a study to compare current computer-assisted technology with the original fluoroscopy-based technique in the laboratory. They concluded that the use of a computer-assisted image guidance system did not enhance the safety or accuracy of placing pedicle screws. However, their computer-assisted system (StealthStation; Medtronic Sofamor-Danek USA, Memphis, Tenn.) only navigated a screw guide tube at the insertion point of the bone surface and did not guide the actual tip of the pedicle probe, tap, or screw within the pedicle.
Kim and colleagues and Ludwig and colleagues conducted a study to compare current computer-assisted technology with the original fluoroscopy-based technique in the laboratory. They concluded that the use of a computer-assisted image guidance system did not enhance the safety or accuracy of placing pedicle screws. However, their computer-assisted system (StealthStation; Medtronic Sofamor-Danek USA, Memphis, Tenn.) only navigated a screw guide tube at the insertion point of the bone surface and did not guide the actual tip of the pedicle probe, tap, or screw within the pedicle.
 Kotani and colleagues developed a new computer-assisted guidance system for cervical pedicle screw placement. The system facilitates obtaining real-time, three-dimensional instrument/screw tip information at each step (probing, tapping, and screw insertion into the vertebra) and is useful in improving the safety and accuracy of pedicle screw placement in the cervical spine.
Kotani and colleagues developed a new computer-assisted guidance system for cervical pedicle screw placement. The system facilitates obtaining real-time, three-dimensional instrument/screw tip information at each step (probing, tapping, and screw insertion into the vertebra) and is useful in improving the safety and accuracy of pedicle screw placement in the cervical spine.
 More recently, several authors have reported that intraoperative three-dimensional fluoroscopy-based navigation improved the safety and accuracy of the pedicle screw insertion in the cervical spine.
More recently, several authors have reported that intraoperative three-dimensional fluoroscopy-based navigation improved the safety and accuracy of the pedicle screw insertion in the cervical spine.
 Rajasekaran and colleagues emphasized that the advantages conferred by cervical pedicle screws into adults also can be extended to the pediatric population.
Rajasekaran and colleagues emphasized that the advantages conferred by cervical pedicle screws into adults also can be extended to the pediatric population.
 Further modifications and developments in technology will increase safety and refine surgical techniques.
Further modifications and developments in technology will increase safety and refine surgical techniques.
Step 1 Instrumentation/Implantation
• Screw diameters vary from 3.5 to 4.5 mm for cervical pedicle screw fixation. However, a screw with a proper diameter must be chosen to obtain sufficient bite of the screw thread in the pedicle cortex. The length of the screw is usually 20 to 24 mm for C3 to C7. A screw length of 24 mm or more is sometimes required to penetrate the anterior cortex of the vertebral body to increase the C2 screw stability. A constrained type of locking mechanism is essential for connecting the screws and plates/rods, to obtain the rigid stabilizing effect of this procedure. Regarding the longitudinal connectors of screws, a rod rather than a plate is recommended for multisegmental fixation.
Step 2
 Before plate or rod application, a posterior decompression by laminoplasty or laminectomy is recommended for a patient with a narrow spinal canal, to avoid possible neurologic deterioration caused when the vertebral alignment is changed after longitudinal connection of the screws.
Before plate or rod application, a posterior decompression by laminoplasty or laminectomy is recommended for a patient with a narrow spinal canal, to avoid possible neurologic deterioration caused when the vertebral alignment is changed after longitudinal connection of the screws.
 The lateral masses and laminae must be decorticated, and bone chips obtained from spinous processes and laminae must be placed.
The lateral masses and laminae must be decorticated, and bone chips obtained from spinous processes and laminae must be placed.
 In the final stage of instrumentation, inserted screws are connected with a plate or rod.
In the final stage of instrumentation, inserted screws are connected with a plate or rod.
 The alignment of the screw head in the coronal plane may be off in multilevel fixation. Therefore a rod with a screw rather than plate is recommended for multilevel fixation across three segments.
The alignment of the screw head in the coronal plane may be off in multilevel fixation. Therefore a rod with a screw rather than plate is recommended for multilevel fixation across three segments.
Step 3
• The pedicle screw procedure is a strong tool for correction of the deformities in the cervical spine.
• Plates and rods are contoured in the sagittal plane, with the expected correction of kyphotic deformity.
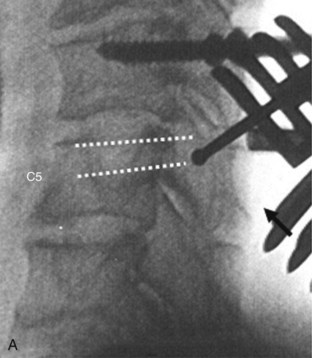
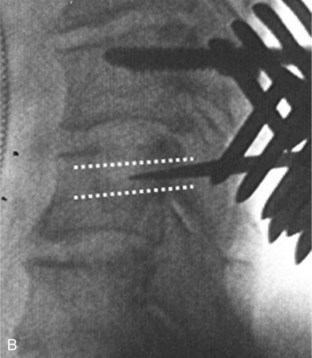
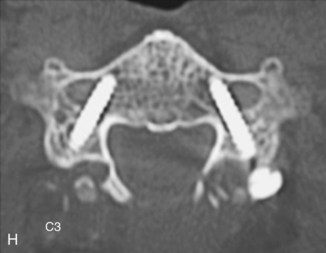
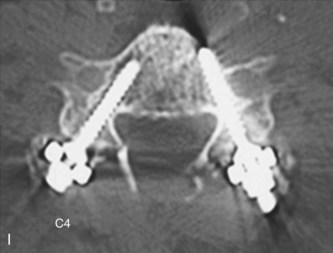
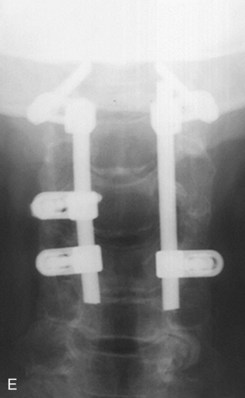
• Correction of the kyphosis is performed by tightening the nuts or by rotating the rods using rodholders (Figure 13-12). A preoperative myelogram (see Figure 13-12, A) shows postlaminectomy kyphosis. MRI images (see Figure 13-12, B and C) demonstrate dumbbell-type recurrent spinal cord tumor (schwannoma). A postmyelogram CT (see Figure 13-12, D) shows that the tumor is expanding from intracanal-extradural to the outside of the spinal canal. The patient sustained progressive spinal cord compression symptoms. The patient underwent simultaneous posterior decompression by tumor extirpation and correction of kyphosis (see Figure 13-12, E and F). Consequently, the posterior part of the cervical spine can be shortened.
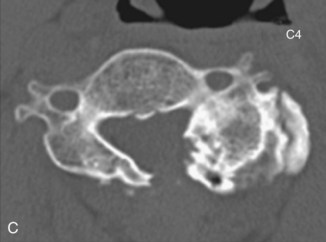
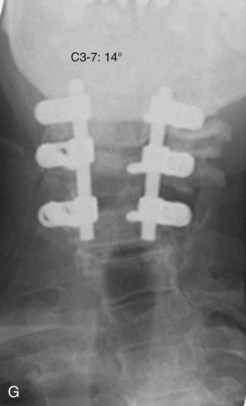
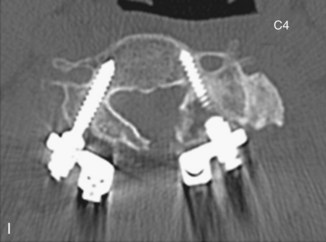
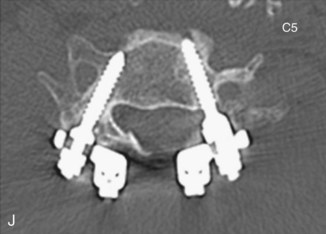
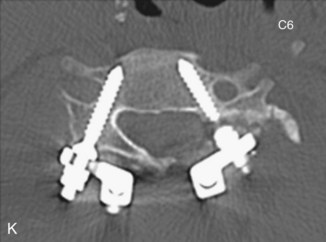
• Cases of cervical scoliosis requiring surgical correction are uncommon. If necessary, however, the deformity is correctable using this procedure by applying distraction force on the concave side (Figure 13-13). Preoperative images (see Figure 13-13, A and B) show 31 degrees of scoliosis after laminoplasty. The patient suffered from severe radiculopathy of the left C5 and C6 caused by C4-5 and C5-6 foraminal stenosis. Preoperative CT scans (see Figure 13-13, C to F) show proliferated degenerative changes of the left lateral mass. In Figure 13-13, G and H, postoperative images show sufficient correction of scoliosis. Postoperative CT images (see Figure 13-13, G to K) show proper screw placement in each vertebra.
Step 3 Pearls
• The neural foramina in patients with degenerative disorders are sometimes stenotic preoperatively. There is the risk of iatrogenic nerve root lesion because of foraminal stenosis caused by reduction of anterior translation or correction of kyphosis.
• Reconstructive CT performed in the oblique plane provides useful information about the size of the neural foramen.
• The use of a washer under the plate/rod for the cranial vertebral screws is helpful in situations where excessive reduction would occur during screw tightening.
• During the correction of kyphosis, the surgeon must also avoid applying excessive compression force at the spinal segment having neural foraminal stenosis because of degenerative changes. A prophylactic foraminotomy is recommended for the segments with marked stenosis of the neural foramen.
Postoperative Care and Expected Outcomes
 Complications directly attributable to screw insertion
Complications directly attributable to screw insertion
 Complications not directly attributable to screw insertion
Complications not directly attributable to screw insertion
Summary
 Pedicle screw fixation is a strong procedure for reconstruction of the cervical spine in various types of disorders. Furthermore, a screw inserted into the cervical pedicle screw can be a strong anchor for reconstruction of the craniocervical junction and cervicothoracic spine. Surgeons must keep in mind that there must be limitations of cervical pedicle screw placement based on anatomic variations of the pedicle and vertebral artery. Complications associated with cervical pedicle screw fixation cannot be completely obviated; however, they can be minimized by sufficient preoperative imaging studies of the pedicles, thorough knowledge of local anatomy, and strict control of screw placement during surgery.
Pedicle screw fixation is a strong procedure for reconstruction of the cervical spine in various types of disorders. Furthermore, a screw inserted into the cervical pedicle screw can be a strong anchor for reconstruction of the craniocervical junction and cervicothoracic spine. Surgeons must keep in mind that there must be limitations of cervical pedicle screw placement based on anatomic variations of the pedicle and vertebral artery. Complications associated with cervical pedicle screw fixation cannot be completely obviated; however, they can be minimized by sufficient preoperative imaging studies of the pedicles, thorough knowledge of local anatomy, and strict control of screw placement during surgery.
 Cervical pedicle screw fixation may become a more definitive tool for reconstruction of the cervical spine in the future with progress in supplemental technology, including computer navigation systems, monitoring procedures of the nerve, and so forth.
Cervical pedicle screw fixation may become a more definitive tool for reconstruction of the cervical spine in the future with progress in supplemental technology, including computer navigation systems, monitoring procedures of the nerve, and so forth.
Abumi K, Ito M, Kotani Y. Complications of cervical pedicle screw placement. Semin Spine Surg. 2002;14:112-124.
Abumi K, Ito H, Taneichi H, et al. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine. Description of the techniques and preliminary report. J Spinal Disorder. 1994;7:19-28.
Abumi K, Kaneda K, Shono Y, et al. One-stage posterior decompression and reconstruction of the cervical spine by using pedicle screw fixation systems. J Neurosurg. 1999;90(Suppl 1):19-26.
Abumi K, Shono Y, Ito M, et al. Complication of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962-969.
Abumi K, Shono Y, Taneichi T, et al. Correction of cervical kyphosis using pedicle screw fixation systems. Spine. 1999;24:2389-2396.
Abumi K, Takada T, Shono Y, et al. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine. 1999;24:1425-1434.
Duan S, Lv S, Ye F, Lin Q. Imaging anatomy and variation of vertebral artery and bone structure at craniocervical junction. Eur Spine J. 2009;18:1102-1108.
Dunlap BJ, Karaikovic EE, Park HS, Sokolowski MJ, Zhang LQ. Load-sharing properties of cervical pedicle screw-rod constructs versus lateral mass screw-rod constructs. Eur Spine J. 2010;19:803-808.
Goel A, Leheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994;129:47-53.
Hojo Y, Ito M, Abumi K, et al. A late neurological complication following posterior correction surgery of severe cervical kyphosis. Eur Spine J. 2010;20:890-898.
Ishikawa Y, Kanemura T, Yoshida G, et al. Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine. 2010;13:606-611.
Johnston TL, Karaikovic EE, Lautenschlager EP, et al. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667-672.
Karaikovic EE, Daubs MD, Madsen RW, et al. Morphologic characteristics of human cervical pedicles. Spine. 1997;22:493-550.
Karaikovic EE, Kunakornsawat S, Daubs MD, et al. Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord. 2000;13:63-72.
Karaikovic EE, Yngsakmongkol W, Gaines RW. Accuracy of cervical pedicle screw placement using the funnel technique. Spine. 2001;26:2456-2462.
Kast E, Mohr K, Richter HP, Borm W. Complication of transpedicular screw fixation in the cervical spine. Eur Spine J. 2005;15:327-334.
Kim HS, Heller JG, Hudgins PA, et al. The accuracy of computed tomography in assessing cervical pedicle screw placement. Spine. 2003;28:2441-2446.
Kotani Y, Abumi K, Ito M. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 1993;99(Suppl 3):257-263.
Kothe R, Ruther W, Schneider E, et al. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29:1969-1975.
Leconte P. Fracture et luxation des deux premieres vertebres cervicales. In: Judet R, editor. Luxation Congénitale de la Hanche. Fractures du Cou-de-pied Rachis Cervical. Actualités de Chirurgie Orthopédique de l’Hôpital Raymond-Poincaré, vol 3. Paris: Masson et Cie; 1964:147-166.
Ludwig SC, Kowalski JM, Edwards CC2nd, et al. Comparative accuracy of two insertion techniques. Spine. 2000;25:2675-2681.
Oda I, Abumi K, Sell LC, et al. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine. 1999;24:2377-2382.