Antivirals, Antiretrovirals, and Antifungal Medications
Objectives
1. Describe how antiviral, antiretroviral, and antifungal medications work.
3. Outline Standard Precautions the nurse takes in limiting exposure to AIDS. (Review material in Chapter 10.)
Key Terms
acquired immune deficiency syndrome (AIDS) (ā-KWĪ-ĕrd ĬM-ū-nō-dē-FĬSH-ĭn-sē, p. 189)
antifungal medications (ăn-tī-FŬN-găl, p. 196)
antiretrovirals (ăn-tī-RĔT-rō-vī-rălz, p. 191)
human immunodeficiency virus (HIV) (ĬM-ū-nō-dē-FĬSH-ĭn-sē, p. 190)
mycotic infections (mī-KŎT-ĭk, p. 196)
opportunistic infections (ŏp-ŏr-TŪN-ĭst-ĭk, p. 193)
retrovirus (RĔT-rō-vī-rŭs, p. 190)
virions (VĪ-rē-ŭnz, p. 190)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
Antiviral and antiretroviral drugs have two basic uses: (1) They treat a variety of common conditions caused by different viruses. These include viruses that cause herpes zoster, herpes simplex, genital herpes, varicella, and some influenza infections. Some antiviral medications are helpful in treating patients with cytomegalovirus retinitis. (2) More specialized antiviral products are used in treating the immunocompromised patient with human immunodeficiency virus (HIV) infection or for adults and children at risk for developing HIV and acquired immune deficiency syndrome (AIDs). They do not cure HIV or AIDS but they do help many patients live longer by acting to stop the production of new retroviruses by interfering with the ability of the retrovirus to replicate (reproduce).
Antivirals
Overview
A virus is a small infectious agent that can replicate only inside the living cells of organisms. They cannot survive without finding a host in which they may metabolize or make chemicals, grow, and reproduce. Viral infections are not suppressed by antibiotics. Antivirals interfere with the ability of the virus to carry out these reproductive functions.
Action and Uses
Many individuals have times when their body is not as strong at fighting infection as at other times or have low immunity. Individuals who once had varicella (chickenpox) still have the virus in their bodies. When immunity is low, patients have a greater chance of developing herpes infections from these usually quiet viruses that remained behind from the chicken pox. We now have some medications that are helpful in reducing the effects of some types of viral infections, such as herpes or influenza. Most common antiviral drugs may therefore be classed as either antiherpes, antiinfluenza, or neuraminidase inhibitors.
Antiviral drugs must enter the infected cell and act at the site of infection to be effective. The drugs often act in a very specific manner—they stop the virus from growing, but cannot kill it.
Antivirals used for herpes simplex or zoster are effective for short-term treatment, long-term suppression, and treatment of recurrence. Treatment of acute infection does not eliminate the chronic infection, which lies dormant. Resistance to the action of the drug may develop quickly.
Resistance to the antiinfluenza drugs amantadine and rimantadine has made them largely ineffective for the treatment of influenza. Neuraminidase products are effective against most strains of influenza A and B but the product may not always be available. With concerns about Avian flu, the government has stockpiled more of these products. Zanamivir is an antiviral product that must be given by inhalation.
Adverse Reactions
Many of these antiviral drugs are given topically and may have few recognized side or adverse effects. Some of the drugs are quite new, and information about adverse effects is still being collected. All health care personnel involved with giving these drugs must read the latest product information before administering these products.
Drug Interactions
Antivirals may also have drug interactions, often with products not usually involved in drug reactions. If giving antivirals, the nurse must read carefully about each of these products to determine if it can be given safely to the patient.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Understand clearly why the product is being ordered and what the physician or other health care provider hopes to accomplish with the drug plan. Learn all about the patient’s history. Know the precautions or contraindications. What conditions exist that may help or hurt the patient’s ability to take antiviral medicines as prescribed?
n Diagnosis
Identify other problems this patient has that might limit the effectiveness of treatment. Because antivirals only lessen symptoms and cannot cure disease, the same viral infection often occurs many times, and patients may need education, comfort, and basic teaching about how to reduce pain, itching, or discharge. These patients often experience weakness and muscle wasting. Ask questions such as: Do they have adequate nutrition? Can they afford the medicine? Will they be compliant?
n Planning
More information about antiviral medications is available every day. Review the latest information from the package inserts before giving these products.
n Implementation
Several of these products have special storage requirements or instructions for mixing. Read the latest information to administer these products correctly.
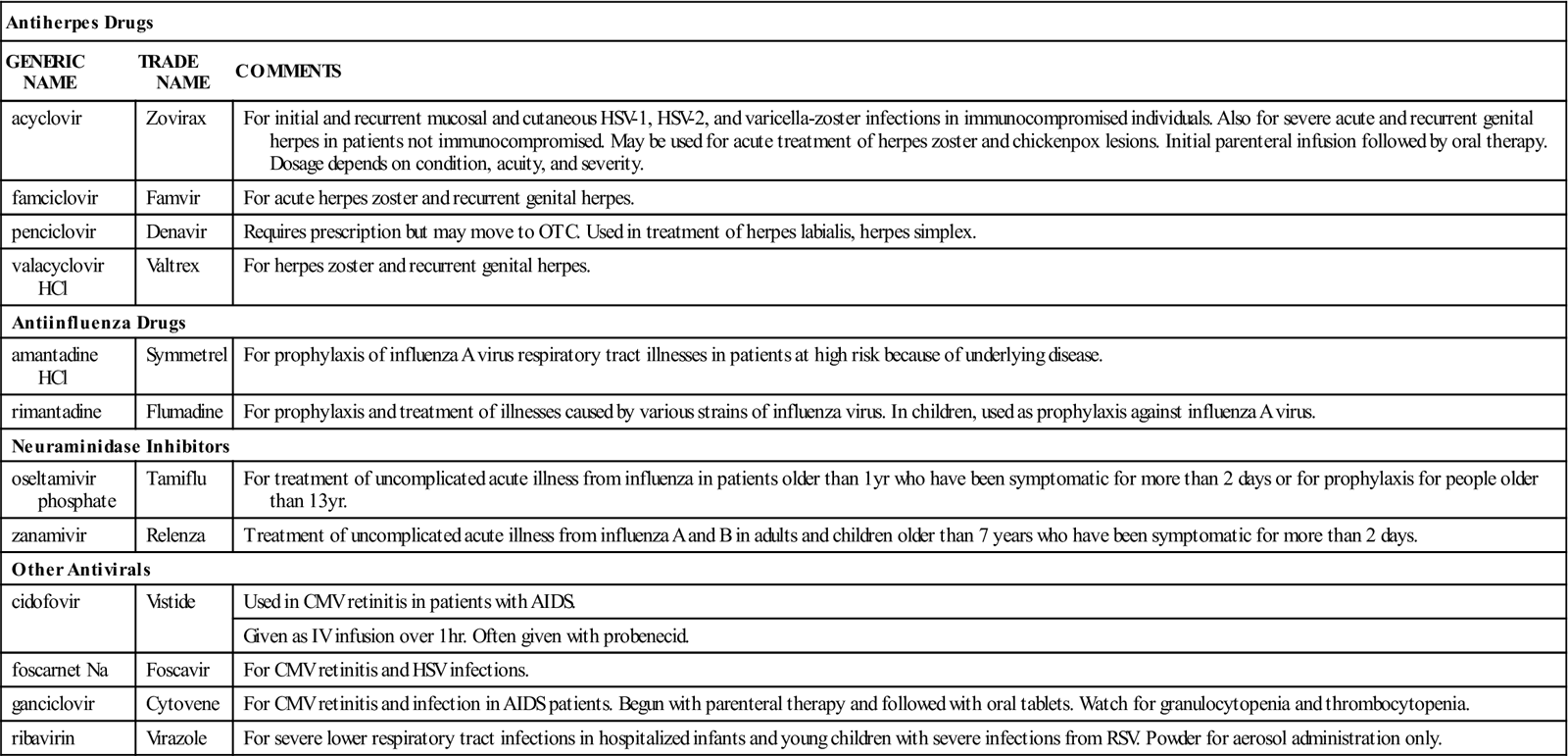
Specific information about these products is given in Table 13-1.
![]() Table 13-1
Table 13-1
| Antiherpes Drugs | ||
| GENERIC NAME | TRADE NAME | COMMENTS |
| acyclovir | Zovirax | For initial and recurrent mucosal and cutaneous HSV-1, HSV-2, and varicella-zoster infections in immunocompromised individuals. Also for severe acute and recurrent genital herpes in patients not immunocompromised. May be used for acute treatment of herpes zoster and chickenpox lesions. Initial parenteral infusion followed by oral therapy. Dosage depends on condition, acuity, and severity. |
| famciclovir | Famvir | For acute herpes zoster and recurrent genital herpes. |
| penciclovir | Denavir | Requires prescription but may move to OTC. Used in treatment of herpes labialis, herpes simplex. |
| valacyclovir HCl | Valtrex | For herpes zoster and recurrent genital herpes. |
| Antiinfluenza Drugs | ||
| amantadine HCl | Symmetrel | For prophylaxis of influenza A virus respiratory tract illnesses in patients at high risk because of underlying disease. |
| rimantadine | Flumadine | For prophylaxis and treatment of illnesses caused by various strains of influenza virus. In children, used as prophylaxis against influenza A virus. |
| Neuraminidase Inhibitors | ||
| oseltamivir phosphate | Tamiflu | For treatment of uncomplicated acute illness from influenza in patients older than 1 yr who have been symptomatic for more than 2 days or for prophylaxis for people older than 13 yr. |
| zanamivir | Relenza | Treatment of uncomplicated acute illness from influenza A and B in adults and children older than 7 years who have been symptomatic for more than 2 days. |
| Other Antivirals | ||
| cidofovir | Vistide | Used in CMV retinitis in patients with AIDS. |
| Given as IV infusion over 1 hr. Often given with probenecid. | ||
| foscarnet Na | Foscavir | For CMV retinitis and HSV infections. |
| ganciclovir | Cytovene | For CMV retinitis and infection in AIDS patients. Begun with parenteral therapy and followed with oral tablets. Watch for granulocytopenia and thrombocytopenia. |
| ribavirin | Virazole | For severe lower respiratory tract infections in hospitalized infants and young children with severe infections from RSV. Powder for aerosol administration only. |
n Evaluation
Watch the patient for signs of improvement in symptoms. Watch particularly for signs of toxicity or adverse effects that are specific to the medication taken.
n Patient and Family Teaching
Tell the patient and family the following:
• This medication is usually able to reduce or suppress symptoms, but it does not cure disease.
• The patient should be careful to follow any specific storage instructions for the medication.
The health care provider should work with pregnant patients to admit them to the national Antiretroviral Registry. This registry is the only project to evaluate first-trimester as well as late-pregnancy exposure to antiretroviral medications. Patient confidentiality is protected. Information obtained through this registry is used to learn how to weigh the risks and benefits of treatment for pregnant women and their fetuses.
Antiretroviral Agents
Overview
Acquired immune deficiency syndrome (AIDS) is a disease that causes a breakdown in the immune system, leaving the patient unable to fight infection. Because many people who develop AIDS die, it is one of the most frightening diseases. More than 98% of individuals who develop the most severe form of the disease die within 5 years of diagnosis. In some cases, advances in treatment have prolonged the lives of patients who can get the needed medications for as long as 35 years.
AIDS is a viral disease that arose in central Africa in the 1950s but is now found throughout the world. In the United States, the groups at highest risk for developing AIDS include homosexual and bisexual men, although the fastest growing group to develop AIDS is heterosexual women. Intravenous drug abusers, people in prison, female sexual partners of people in AIDS risk groups, and children born to mothers at risk of being HIV positive make up the other groups of people most likely to get AIDS. Minorities are overrepresented among the people who get AIDS. Recipients of blood products or of semen for artificial insemination also have developed AIDS. Because AIDS is an epidemic with a high mortality rate, it is important to understand what role medications play in slowing the advance of this disease and treating the other diseases that may result from the patient’s reduced immunity.
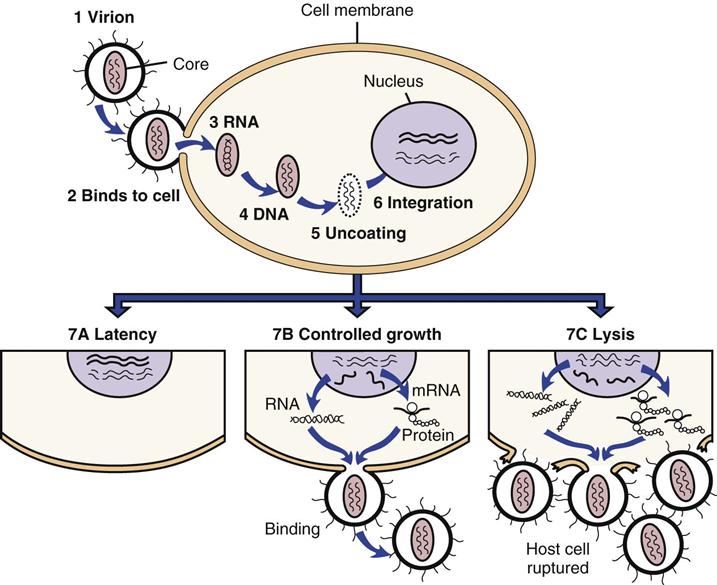
AIDS is caused by a retrovirus currently named human immunodeficiency virus (HIV). Retroviruses are viruses that contain ribonucleic acid (RNA) rather than deoxyribonucleic acid (DNA) as their genetic material. The HIV attaches to the CD4 protein with the help of coreceptors (CXCR4 or CCR5) found on helper T lymphocytes and other cells such as macrophages and dendritic cells. The HIV then fuses its membrane with that of the host cell and inserts its genetic material into the cytoplasm. The viral genetic material is then transcribed into double-stranded DNA called proviral DNA. The HIV enzyme reverse transcriptase is responsible for creating proviral DNA from viral RNA. Once produced, this DNA often becomes integrated into the chromosomal DNA of the host cell. The HIV DNA is then able to use the host cell’s genetic machinery to create new HIV RNA genetic material and messenger RNA. The messenger RNA codes for the development of HIV polyproteins, which must be cleaved, or separated, into individual proteins by the HIV enzyme protease for infectious virions (rudimentary virus particles) to be produced. Once this occurs, new virions are assembled; these bud from the host cell’s membrane and are able to infect new cells. This process is demonstrated in Figure 13-1![]() . Antiretrovirals are an important group of drugs that slow the growth or prevent the duplication of retroviruses; they are used to limit the advance of HIV and AIDS.
. Antiretrovirals are an important group of drugs that slow the growth or prevent the duplication of retroviruses; they are used to limit the advance of HIV and AIDS.
Research and clinical drug trials continue to make changes in what we know about AIDS. This will affect what drugs we use to treat AIDS patients and how we use them. Use only the most current information about these medications and their use in HIV-positive patients.
Action
By interfering with the ability of a retrovirus to reproduce, or replicate, antiretroviral agents act to stop more retroviruses from being made. At present, there are a wide variety of antiretrovirals in clinical use with other products in development. These types include:
Uses
Antiretroviral agents are used to slow the advance of AIDS infection and support whatever immunity the patient still has. They may also be used to prevent HIV in infants born to HIV-infected mothers or in health care workers who have been exposed to HIV. (The effectiveness of such treatment is shown when there is no change in antibody test results from HIV-negative to HIV-positive, or seroconversion.) All of these medications are relatively new and fairly toxic, with many adverse effects and drug interactions. Pediatric antiretroviral medication usage is different than that for adults.
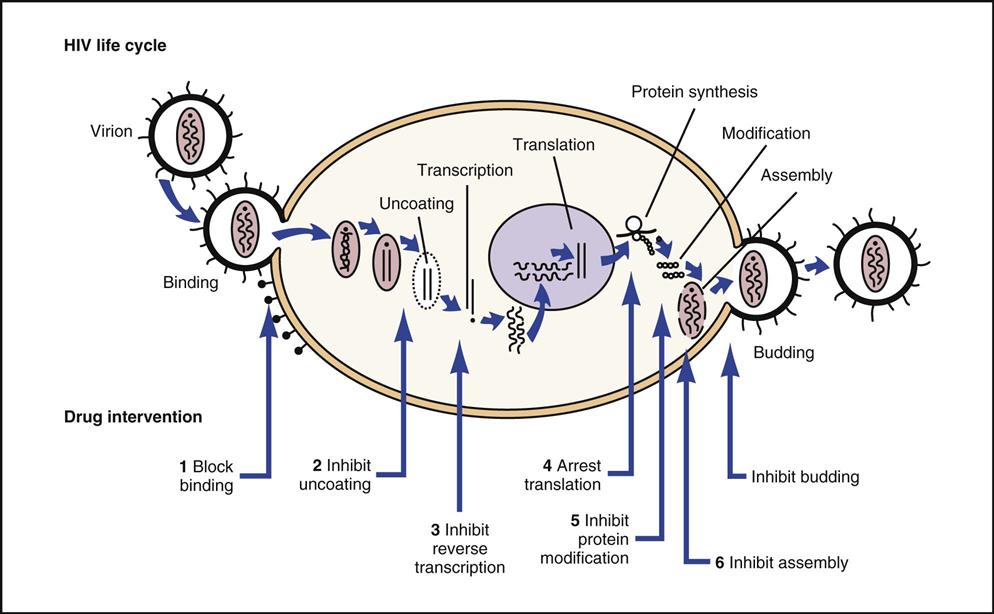
Figure 13-2 illustrates different stages in which drugs attack HIV. Antiretroviral medications are given only under the direction of a specialist, but the nurse may encounter patients getting these drugs when they are admitted with other health problems.
Adverse Reactions
Antiretrovirals often cause severe toxic reactions. The nurse constantly watches for symptoms of pancreatitis, peripheral neuropathy, and myopathies, as well as less serious conditions such as mouth ulcers, rash, headaches, diarrhea, and nausea. Most of these products can also cause damage to the liver or kidneys (hepatotoxic or nephrotoxic); many are associated with blood dyscrasias and peripheral neuropathies.
Drug Interactions
Most antiretroviral agents inhibit the cytochrome P-450 enzyme system involved in the metabolism of medications in the liver. For this reason, they should not be taken at the same time as other drugs. It is important to check with the physician or other health care provider before any medications are given to patients taking antiretroviral medications. Many of these drugs are changed when given at the same time as other drugs.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn all about the history and course of the disease, the medications the patient has used, and past response to the medications. Most drugs used in the treatment of AIDS are toxic to the liver. Assess for past or present history of hepatitis or hepatomegaly (enlarged liver) plus current, as well as past, alcohol use or abuse. Assess for a history of pancreatitis and symptoms of peripheral neuropathy, because these are frequently caused by medications.
Ask about AIDS-related opportunistic infections—infections that develop because the damage to the body’s immune system leaves it unable to protect the patient against other infections. Opportunistic infections would not ordinarily be a problem to an individual, but because of reduced immunity, they may cause great pain and suffering in an AIDS patient. Ask the patient specifically about respiratory infections, skin lesions, and Candida infections.
Some of the specific questions the nurse might ask to explore related patient problems include: What are the patient’s beliefs and feelings about this illness? Does the patient have a support system? Does he or she have friends and family who can help the patient when he or she is most vulnerable to infection or having problems? Does the patient have health care insurance and the means to pay for medicines? Is the patient in need of financial assistance?
n Diagnosis
The medical diagnosis might be clear. In order to understand it, the nurse will want to understand what stage of disease the patient has (e.g., if the diagnosis is limited to exposure to HIV, or has exposure progressed to actual infection and symptoms). In addition to the medical diagnosis, the nurse will explore whether the patient has problems in the areas of hydration, nutrition, or hygiene? What are the financial needs, emotional concerns, and spiritual needs? Is there a support system in place, or is the patient going through this illness alone? Does the patient engage in unsafe sex or drug practices that put other individuals at risk? Are there knowledge deficits about HIV infection, prognosis, and treatment?
n Planning
Compliance is a big challenge for patients with HIV infection. They must return frequently to their health care providers for tests and examinations. Because they are at risk for developing opportunistic infections as a result of their damaged immune system, patients must be taught the signs of such infections. The patients must be willing to take all the medicines that are prescribed. Antiretroviral drugs are expensive and may have complicated directions for when they need to be taken. The drugs may cause side effects. For patients who are trying to slow or halt their HIV infection, it is important to provide individual teaching, encouragement and support and help with specific problems that present obstacles to treatment goals.
Before beginning drug therapy with antiretrovirals, the helper T lymphocyte (CD4) count must be measured, and plasma HIV RNA laboratory studies must be done. These results help assess a patient’s immunologic status and severity of infection. They also provide a means of measuring how well the treatment is working. A complete blood cell count (including a WBC count with differential), folate, vitamin B12, ferritin, iron, and percentage of iron saturation, should also be obtained. Liver function tests and hepatitis B, C, and A serologies, as well as amylase, triglyceride, and lipase levels, will also be ordered. All of these laboratory studies are repeated during the treatment and help show treatment success or onset of adverse effects.
All of the protease inhibitors are potent inhibitors of the cytochrome P-450 enzyme system and have many contraindications to use of other drugs at the same time.
n Implementation
In working with HIV-infected patients, be certain to follow Standard Precautions. Wear gloves when necessary to avoid exposure to lesions or bodily fluids. Patients should be taught how to take care of minor problems and when they should return for care.
Table 13-2 provides a list of important information about antiretrovirals.
![]() Table 13-2
Table 13-2
| DRUG | CLINICAL TOXICITIES | NURSING IMPLICATIONS |
| Nucleoside Reverse Transcriptase Inhibitors | ||
| Nucleoside Analogues | ||
| didanosine (ddI) (Videx) | Pancreatitis, peripheral neuropathy, retinal depigmentation, diarrhea, headache, dry mouth, insomnia, nervousness | Medication should not be taken with food or mixed with acidic beverages; separate other drugs from ddI by 2 hr. |
| lamivudine (3TC) (Epivir-HBV) | Peripheral neuropathy, headache, pancreatitis (in children) | Used in combination with zidovudine. |
| stavudine (d4T) (Zerit, Zerit X) | Peripheral neuropathy, diarrhea, nausea, vomiting | Do not use with zidovudine. |
| zidovudine (ZDV, AZT) (Retrovir) | Headache, nausea, myopathy, myositis, malaise, hepatic stenosis | Nausea and headaches often resolve after 4-6 weeks of therapy; 60% CNS penetration; drug of choice for HIV CNS disease. |
| Nonnucleoside Reverse Transcriptase Inhibitors | ||
| abacavir sulfate (Ziagen) | Fatal hypersensitivity reactions (discontinue immediately if any signs of hypersensitivity appear) | Question patient about any new symptoms that may suggest hypersensitivity. |
| delavirdine (DLV) (Rescriptor) | Rash (pruritus), headaches | When used as monotherapy, resistance can rapidly develop; antacids decrease absorption. If used with ddI, separate by 1 hr. |
| efavirenz (Sustiva) | Used together with other antiretroviral agents in treating HIV | Take on an empty stomach. |
| nevirapine (NVP) (Viramune) | Rash (Stevens-Johnson syndrome) | When used as monotherapy, resistance can rapidly develop; once-daily dosing during first 2 wk may lessen incidence of rash. |
| Protease Inhibitors | ||
| amprenavir (Agenerase) | Rash, nausea, diarrhea | |
| atazanavir (Reyataz) | Indirect hyperbilirubinemia, prolonged PR interval, fat maldistribution, hyperglycemia | |
| Fosamprenavir (Lexiva) | Skin rash, diarrhea, nausea, headache, fat maldistribution | |
| indinavir (Crixivan) | Nephrolithiasis, nausea, abdominal pain, “Crix belly,” hematuria | Should be taken 1 hr before or 2 hr after meals; increase fluids to drink >1.5 L/day to avoid renal stones; decrease rifabutin dose by half. |
| Concurrent use with St. John’s wort and other CYP3A substrates contraindicated. | ||
| nelfinavir mesylate (Viracept) | Diarrhea, nausea | Should be taken with food. |
| ritonavir (Norvir) | Nausea, diarrhea, taste changes, circumoral paresthesias, thrombocytopenia | Should be taken with food; used extensively with other antiviral drugs because of the numerous drug interactions. These drug-drug interactions result in greater blood levels and better efficacy. |
| saquinavir mesylate (Invirase) | Diarrhea, nausea, abdominal pain, ataxia, neutropenia, hemolytic anemias | Should be taken with high-fat meals. |
| Second-Generation Protease Inhibitors | ||
| darunavir (Prezista) | Nausea, vomiting, diarrhea | |
| Fusion Inhibitor | ||
| enfuvirtide (Fuzeon) | Hypersensitivity, local site reaction, diarrhea, nausea, fatigue | Must be taken by subcutaneous injection twice daily, rotating sites. |
| HIV Integrase Inhibitor | ||
| raltegravir (Isentress) | Diarrhea, nausea, headache | |
| Combination Productions | ||
| zidovudine/lamivudine (Combivir) | May help compliance. | |
| zidovudine/lamivudine/abacavir (Trizivir) | May help compliance. | |
| lopinavir/ritonavir (Kaletra) | May help compliance. | |
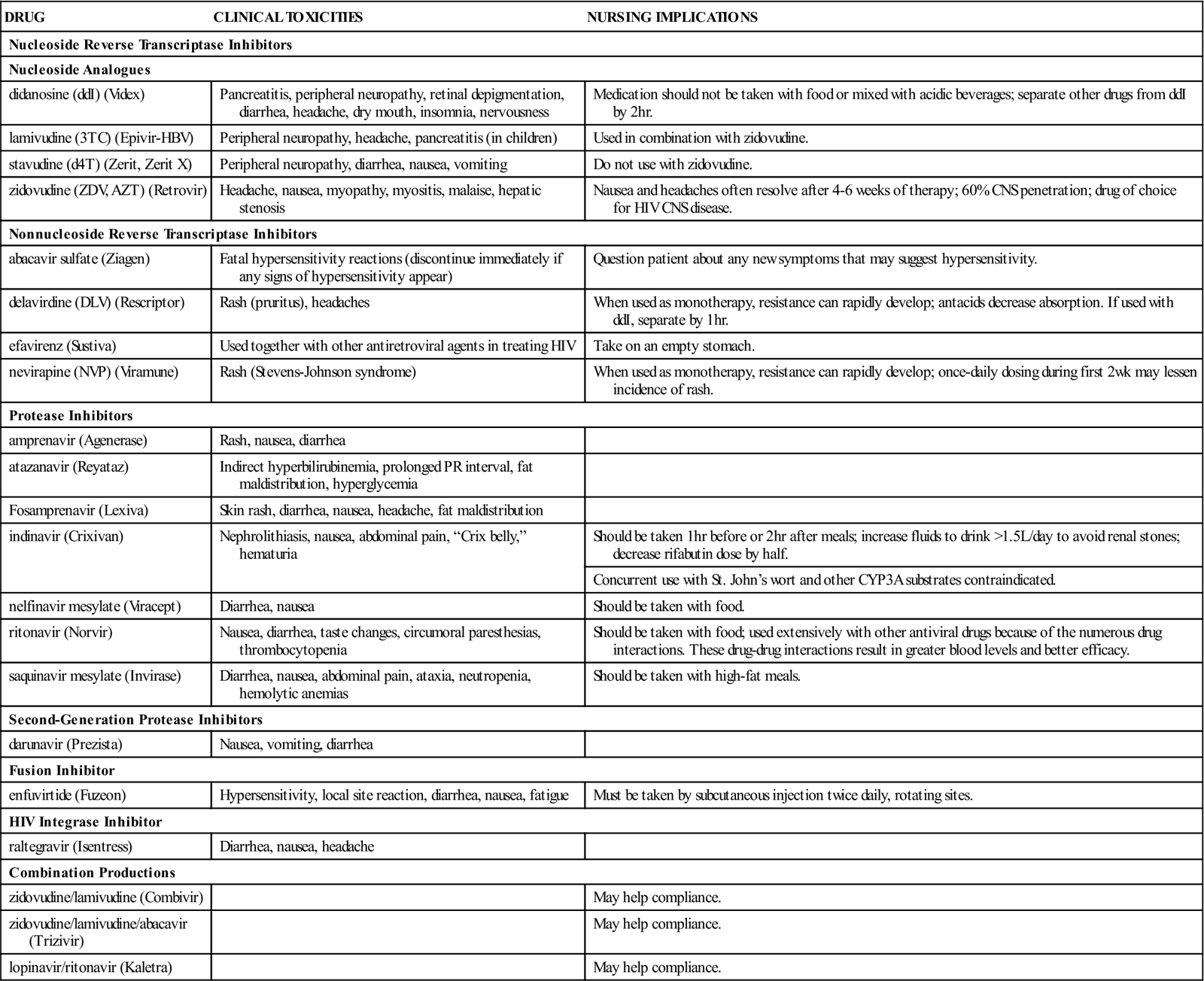
CNS, Central nervous system; HIV, human immunodeficiency virus.
n Evaluation
Patients must see their health care provider on a frequent basis for further blood work that measures their WBC level and may indicate the presence of infection. Patients must also return to their health care provider sooner for evaluation than their regular schedule when they suspect the presence of opportunistic infections. Patients generally have fewer severe side effects with the protease inhibitors, although patients taking indinavir sulfate may develop “Crix belly.” This is a syndrome characterized by elevated levels of triglycerides, cholesterol, and plasma glucose, with a weight gain of 40 lb or greater. Fat accumulates in the lower abdomen and flanks, and tissue is often lost in the arms and legs.
n Patient and Family Teaching
Tell the patient and family the following:
The patient should report signs and symptoms of sensorimotor peripheral neuropathy caused by several of the reverse transcriptase inhibitors. Initially, the patient feels numbness and burning, usually involving the toes. Patients may have decreased light touch, pinprick, temperature, and vibration sensation in the feet and up to the midcalf. These symptoms may be followed by sharp, shooting pains, which progress to severe, continuous burning pain that is often worse at night and requires narcotic analgesics.
Antifungals
Overview
Fungal infections are often called opportunistic infections because they develop when the patient’s immunity is weak. Some fungal infections are kept to a localized area, whereas others may become spread throughout the patient’s whole body. Fungi are more complex organisms than bacteria and thus require drugs that act in a different way than antibacterials. Antifungals often have adverse effects and their use must be closely monitored.
Action and Uses
A fungus is a plant that produces yeastlike or moldlike diseases called mycotic infections in humans. These can be either superficial infections, such as in the skin or nail, or systemic infections, such as in the lung or liver. Because fungi are found almost everywhere—in most water supplies, in the air, and in the soil—they pose a real risk for immunocompromised patients.
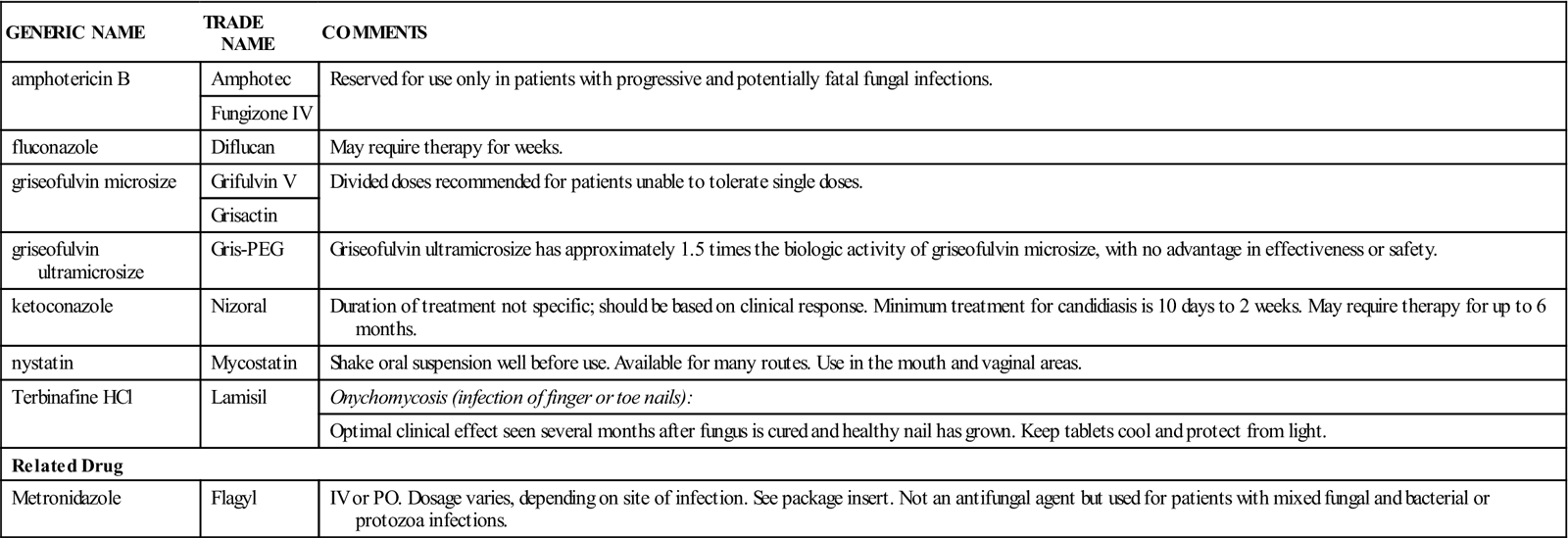
Antifungal medications are used orally, intravenously, topically, and vaginally to treat mycotic infections. There are a variety of antifungals; some are used primarily for vaginal yeast or fungal infections, and others are used to treat superficial or systemic infections. The actions and uses of the most common medications used to treat general fungal infections are described in Table 13-3.
![]() Table 13-3
Table 13-3
| GENERIC NAME | TRADE NAME | COMMENTS |
| amphotericin B | Amphotec | Reserved for use only in patients with progressive and potentially fatal fungal infections. |
| Fungizone IV | ||
| fluconazole | Diflucan | May require therapy for weeks. |
| griseofulvin microsize | Grifulvin V | Divided doses recommended for patients unable to tolerate single doses. |
| Grisactin | ||
| griseofulvin ultramicrosize | Gris-PEG | Griseofulvin ultramicrosize has approximately 1.5 times the biologic activity of griseofulvin microsize, with no advantage in effectiveness or safety. |
| ketoconazole | Nizoral | Duration of treatment not specific; should be based on clinical response. Minimum treatment for candidiasis is 10 days to 2 weeks. May require therapy for up to 6 months. |
| nystatin | Mycostatin | Shake oral suspension well before use. Available for many routes. Use in the mouth and vaginal areas. |
| Terbinafine HCl | Lamisil | Onychomycosis (infection of finger or toe nails): |
| Optimal clinical effect seen several months after fungus is cured and healthy nail has grown. Keep tablets cool and protect from light. | ||
| Related Drug | ||
| Metronidazole | Flagyl | IV or PO. Dosage varies, depending on site of infection. See package insert. Not an antifungal agent but used for patients with mixed fungal and bacterial or protozoa infections. |
Because AIDS destroys the body’s immune system, patients with AIDS are prey to many opportunistic infections. Fungi the body would usually keep under control now cause some of the most problematic infections. It is important to understand how antifungal medications may be helpful in improving the general well-being of AIDS patients.
Adverse Reactions
Nausea, vomiting, and diarrhea are the most common reactions. Other products may be associated with more severe problems such as hematologic, renal, or hepatic disease.
Symptoms of overdosage include severe nausea, vomiting, and diarrhea.
Drug Interactions
Severe superinfection may result when antifungals are given together with prolonged corticosteroid therapy. Activity of oral anticoagulants is decreased when they are used at the same time as griseofulvin; it may be necessary to adjust the anticoagulant dosage. Griseofulvin activity is decreased when used at the same time as barbiturates, requiring dosage adjustments of the griseofulvin. Use of alcohol while taking antifungals potentiates, or increases, the effect of the alcohol. Because antacids, anticholinergics, and H2 blockers (e.g., Pepcid, Zantac) change gastrointestinal (GI) pH, the patient should not take ketoconazole for at least 2 hours after taking any H2 blockers.
Toxicity can result when flucytosine is used along with other drugs that depress bone marrow or when used during radiation therapy. Use of flucytosine with hepatotoxic or nephrotoxic drugs should be avoided. The use of flucytosine also decreases leukocyte and platelet counts and hemoglobin levels.
Metronidazole and alcohol always causes a severe reaction called a disulfiram-like reaction. With this reaction, severe nausea, vomiting, tachycardia (rapid heartbeat), flushing, and confusion develops. It is very important to warn patients not to take anything containing alcohol if they are taking metronidazole.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the patient’s health history, including any allergy, bone marrow depression, use of alcohol or other drugs that may produce drug interactions (particularly corticosteroids), and the possibility of pregnancy. Some antifungal drugs may be teratogenic (causing deformities in the fetus).
The patient may have a history of fever and chills at the onset of infection. Itching is a common finding. A history of recent antibiotic therapy is common. The nurse may observe the classic signs of white discharge and erythema (redness or irritation) associated with thrush (Candida infection). The patient may also have a history of multiple scaly or blistered red patches on the skin, itching and soreness of infected areas, and brittle nails with yellow discoloration and separation from the nail bed.
n Diagnosis
In addition to the medical diagnosis, what additional problems does the patient have? Are there difficulties in maintaining adequate nutrition or cleanliness or in paying for medications? Consider the need for education of the patient or family.
n Planning
Individuals allergic to penicillin may exhibit cross-sensitivity to antifungal agents, although this is rare. The patient may experience photosensitivity (abnormal response to exposure to sunlight) when taking these drugs.
Hepatotoxicity (usually reversible) and a few cases of hepatitis in children have been reported with ketoconazole. Liver function studies must be monitored so that any liver damage may be noted. The product should be discontinued if even a minor elevation in the liver function studies develops.
n Implementation
The absorption rate of griseofulvin is increased after the patient eats a fatty meal. Ketoconazole requires stomach acidity for dissolution and absorption. In patients with achlorhydria (lack of hydrochloric acid), tablets should be dissolved in several teaspoons of aqueous 0.2 NHCl solution. The patient should drink the solution with a straw to avoid staining the teeth and should follow the medication with a full glass of water. Explain to the patient how and why this is done.
Because griseofulvin is absorbed over a long period, single daily doses are often adequate. The patient must keep using the medication until the fungal infection is gone, as shown by both clinical and laboratory tests. This process may require several weeks or many months of therapy, depending on the organism responsible and the site of the infection. Use of both oral and topical antifungal agents may be required to treat some fungal infections, primarily tinea pedis (athlete’s foot).
n Evaluation
Observe the patient for therapeutic effects: chills or fever aqssociated with some infections should disappear; watch for signs of GI distress. The patient should continue to take the medication until the laboratory tests show that normal function has returned.
Nausea, vomiting, and diarrhea are symptoms of overdosage of most of the antifungal medications.
n Patient and Family Teaching