CASE 13
You have been Anthony’s general practitioner since childhood. Other than the usual run of minor childhood disorders, there has been nothing of note in his medical history. Both parents and a younger sibling are well. He is currently 22 years of age and is home for the summer, on vacation from college. Anthony had called your office, requesting a complete physical examination, and, as a precursor to that visit, you have ordered a series of routine tests, including serum blood cell counts and electrolyte determinations, chest radiograph, and urinalysis. The day before the appointment the laboratory results become available and show, somewhat surprisingly to you, a marked increase in some liver enzymes (transaminases) and an elevated bilirubin level. Physical examination of this young man when he did come in revealed, not surprisingly, a mild jaundice, with some tenderness at the liver edge. There were no other significant abnormalities, although you also note some healing bruises and pinpricks in the forearm. He seems to be sniffing a lot, as though he has a perpetual postnasal drip, and he seems to be somewhat more edgy in your presence than usual. How are you going to open up a conversation? What do you want to address? Do you have significant concerns?
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implication/Analysis of Family History
There is nothing remarkable about the family history and because you have been Anthony’s physician since childhood you are more concerned about recent lifestyle changes now that he is attending college.
DIAGNOSIS
On the basis of the nucleic acid amplification tests, Anthony is informed that he is infected with HIV, the causative agent of acquired immunodeficiency disease (AIDS). Anthony’s CD4+ T cell count will need to be monitored. As the number of CD4+ T cells decreases, the number of opportunistic infections increases (Fig. 13-1).
THERAPY
Highly active antiretroviral therapy (HAART) is the treatment of choice for HIV-infected patients. This drug regimen includes two antinucleoside analogue inhibitors and a protease inhibitor or a non-nucleoside reverse transcriptase inhibitor. Even though the use of HAART is not a controversial issue, the “when” to initiate therapy is highly debated. This controversy follows the realization that the “hit hard, hit early” slogan of the mid 1990s does not lead to the eradication of the virus in patients despite long term, and early, drug therapy. HIV is detectable in latent infected cells even after prolonged therapy, and so the approach to drug therapy has had to be modified.
Advantages and Disadvantages of HAART
There are advantages and disadvantages to HAART. In patients receiving HAART, plasma HIV RNA levels fall to below the level of detection within 2 to 6 months. There is an increase in CD4+ T cell count and therefore delayed progression to AIDS. As well, in some cases HAART is accompanied by enlargement of the thymus. Whether this enlargement is due to regeneration of the thymus and active thymopoiesis or from the migration of peripheral blood cells into the thymus is currently being addressed using in vivo TREC (T cell receptor excision circles) assay of thymic function (see Case 2). On the down side, hepatotoxicity is a serious consideration, as is the development of viral variants that are resistant to the drugs. Additionally, HAART therapy does not eliminate HIV from resting memory CD4+ T cells carrying an integrated copy of the viral genome. Therefore, on discontinuation of HAART, viral load measures (plasma HIV-1 RNA) become significant when the latently infected cells are activated even by stimulatory molecules normally present in lymphoid tissues.
Role of Cytokines in Therapy
Those who advocate the use of IL-2 as therapy to increase the number of CD4+ T cells in conjunction with HAART suggest that the IL-2 would activate latent cells with the net effect being their eradication, while the patient is protected by HAART. Implicit assumptions in this approach are that the virus strains are not resistant to HAART and that all the latent cells are CD4+ T cells. Recall that some cells that do not express CD4 can be infected after binding to galactosyl ceramide.
Vaccine Failures: “Original Antigenic Sin”
Because mutations can occur early in the course of the disease, the activated cytotoxic T cells are no longer effective, yet immune response to escape mutants is much weaker than that to the primary HIV isolate (“original antigenic sin”). Antibody responses to the initial epitopes have also been reported to dominate. In addition to a blunted response to the escape mutants, the decrease in CD4+ T cells hampers cytotoxic T cell development (and antibody responses) because both require cognate interaction with, and cytokines derived from, CD4+ T cells.
ETIOLOGY OF AIDS: HUMAN IMMUNODEFICIENCY VIRUS
Cell Infection
Cell Surface Receptors
Productive infection requires that HIV binds to both a primary receptor, CD4, and a co-receptor CCR5 or CXCR4 on the target cell. CCR5 and CXCR4 are chemokine receptors that are targeted by different HIV strains (Fig. 13-2). CCR5 is used primarily by macrophage (M) tropic strains, whereas CXCR4 is used primarily by T cell (T) tropic strains. HIV interacts first with the primary receptor, CD4, via its envelope glycoprotein, gp120. Binding to CD4 creates a complex that allows gp120 to bind to CCR5 or CXCR4. After this binding, gp41, which is a fusion protein, enters the cell membrane to initiate fusion of the viral envelope and subsequent delivery of the viral proteins and genome into the cell. Under some circumstances, HIV can infect cells that do not express CD4 (e.g., endothelial cells, microglial cells) by binding galactosyl ceramide.
HIV Evasive Strategies
Downregulation of Class I Expression
Downregulation of class I MHC expression is a relatively common viral evasive strategy, but the mechanisms by which this is achieved vary from virus to virus. In HIV, downregulation of class I MHC is attributed to the action of the HIV regulatory protein, Nef, because its presence, or absence, in the HIV genome affects expression of class I MHC on the cell surface, a requirement for activation of cytotoxic T cells. At least two different mechanisms have been reported to explain this effect; the first is that Nef increases the endocytosis of surface class I MHC; the other is that Nef redirects class I MHC from the Golgi to the cytosol, or sequesters the complex in the Golgi. Irrespective of the mechanism, a decrease in the class I MHC-HIV peptides expressed on the infected cell surface will hinder recognition and targeting by cytotoxic T cells. Interestingly, the amount of class I MHC expressed on a cell surface has been shown to depend on the particular Nef allele encoded by a particular viral variant.
Andrews T, Sullivan KE. Infections in patients with inherited defects in phagocyte function. Clin Microbiol Rev. 2003;16:597.
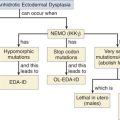
Aradhya S. A recurrent deletion in the ubiquitously expressed NEMO (IKK gamma) gene accounts for the vast majority of incontinentia pigmenti mutations. Hum Mol Genet. 2001;1:2171.
Arakawa H, Hauschild J, Buerstedde JM. Requirement of the activation-induced deaminase (AID) gene for immunoglobulin gene conversion. Science. 2002;295:1301.
Babgdong L, et al. In vivo analysis of Nef function. Curr HIV Res. 2003;1:41.
Badley AD, et al. Mechanisms of HIV-associated lymphocyte apoptosis. Blood. 2000;96:2951.
Baldini A. DiGeorge syndrome: An update. Curr Opin Cardiol. 2004;19:201.
Bartsch O, et al. DiGeorge/velocardiofacial syndrome: FISH studies of chromosomes 22q11 and 10p14, and clinical reports on the proximal 22q11 deletions. Am J Med Genet. 2003;117A:1.
Bellamy R, et al. Variations in the NRAMP1 gene and susceptibility to tuberculosis in Western Africa. N Engl J Med. 1998;338:640.
Bhushan A, Covey LR. CD40:CD40L interactions in X-linked and non X-linked hyper IgM syndrome. Immunol Res. 2001;24:311.
Caamano J, Hunter CA. NFκB family of transcription factors: Central regulators of innate and adaptive immune functions. Clin Microbiol Rev. 2002;15:414.
Carrol ED, et al. Anhidrotic ectodermal dysplasia and immunodeficiency–the role of NEMO. Arch Dis Child. 2003;88:340.
Casper-Bauguil S, et al. Mildly oxidized low density lipoproteins decrease early production of interleukin 2 and nuclear factor κB binding to DNA in activated T-lymphocytes. Biochem J. 1999;337:269.
Chinen J, Puck JM. Successes and risks of gene therapy in primary immunodeficiency diseases. J Allergy Clin Immunol. 2004;113:595.
Clark-Curtiss JE, Haydel SE. Molecular genetics of Mycobacterium tuberculosis pathogenesis. Ann Rev Microbiol. 2003;57:517.
Collins KL, et al. HIV-1 Nef protein protects infected primary cells against killing by cytotoxic T lymphocytes. Nature. 1998;391:397.
Collins KL. How HIV evades CTL recognition. Curr HIV Res. 2003;1:31.
Cooper MA, Pommering TL, Koranyi K. Primary immunodeficiencies. Am Fam Physician. 2003;68:2001.
Cosma CL, Sherman DR, Ramakrishman L. The secret lives of the pathogenic mycobacteria. Ann Rev Microbiol. 2003;57:641.
Cox GM, et al. Superoxide dismutase influences the virulence of Cryptococcus neoformans by affecting growth within macrophages. Infect Immun. 2003;71:173.
Davenport MP, et al. Cell turnover and cell tropism in HIV infection. Trends Microbiol. 2002;10:275.
Doffinger R, et al. X linked anhidrotic ectodermal dysplasia with immunodeficiency is caused by impaired NF-kappa B signaling. Nat Genet. 2001;27:277.
Durandy A, Honjo T. Human genetic defects in class switching recombination (hyper IgM syndrome). Curr Opin Immunol. 2003;12:543.
Edwards E, Razvi S, Cunningham-Rundles C. IgA deficiency: Clinical correlates and responses to pneumococcal vaccine. Clin Immunol. 2004;111:93.
Engel BC, Kohn DB, Podsakoff GM. Update on gene therapy of inherited immune deficiencies. Curr Opin Mol Ther. 2003;5:503.
Fallarino F, et al. Modulation of tryptophan catabolism by regulatory T cells. Nat Immunol. 2003;4:1206.
Farhoudi A, et al. Two related cases of primary complement deficiency. Immunol Invest. 2003;32:313.
Forbes JR, Gros P. Iron, manganese, and cobalt transport by Nramp1 (Slc11a1) and Nramp2 (Slc11a2) expressed at the plasma membrane. Blood. 2003;102:1884.
Futatani T, et al. Deficient expression of Bruton’s tyrosine kinase in monocytes from X-linked agammaglobulinemia as evaluated by a flow cytometric analysis and its clinical application to carrier detection. Blood. 1998;91:595.
Garcia-Perex MA, et al. Mutations of CD40L in two patients with hyper-IgM syndrome. Immunobiology. 2003;207:285.
Gaspar HB, Conley ME. Immunodeficiency review: Early B cell defects. Clin & Exper Immunol. 2000;119:303.
Grimbacher B, et al. Homozygous loss of ICOS is associated with adult-onset common variable immunodeficiency. Nat Immunol. 2003;4:261.
Hacein-Bey-Abina S, et al. Sustained correction of X-linked severe combined immunodeficiency by ex vivo gene therapy. N Engl J Med. 2002;346:1185.
Hidalgo A, et al. Insights into leukocyte adhesion deficiency type 2 from a novel mutation in the GDP-fucose transporter gene. Blood. 2003;101:1705.
Illoh OC. Current applications of flow cytometry in the diagnosis of primary immunodeficiency diseases. Arch Pathol Lab Med. 2004;128:23.
Inohara N, Nuflez G. NODS: Intracellular proteins involved in inflammation and apoptosis. Nat Rev Immunol. 2003;3:371.
Krysztof M, Rieth W. Promoter specific functions of CIITA and MHC class II enhanceosome in transcriptional activation. EMBO J. 2002;21:1379.
Ku CL, et al. NEMO mutations in 2 unrelated boys with severe infections and conical teeth. Pediatrics. 2005;115:e615.
Kwak B, Mulhaupt F, Mach F. Statins as a newly recognized type of immunomodulator. Nat Med. 2000;6:1399.
Li Q, Verma IM. NFκB regulation in the immune system. Nat Rev Immunol. 2002;2:725.
Lu W, et al. Therapeutic dendritic-cell vaccine for simian AIDS. Nat Med. 2003;9:27.
Markert ML, et al. Complete DiGeorge syndrome: Development of rash, lymphadenopathy, and oligoclonal T cells in 5 cases. J Allergy Clin Immunol. 2004;113:734.
Markert ML, et al. Thymus transplantation in complete DiGeorge syndrome: Immunologic and safety evaluations in 12 patients. Blood. 2003;102:1121.
Mastroianni CM, et al. Teaching tired T cell to fight HIV: Time to test IL-15 for immunotherapy? Trends Immunol. 2004;25:121.
McAdam AJ, et al. ICOS is critical for CD40-mediated antibody switching. Nature. 2001;409:102.
Nelson M. Metal ion transporters and homeostasis. EMBO J. 1999;18:4361.
Orange JS, Geha RS. Finding NEMO: Genetic disorders of NFκB activation. J Clin Invest. 2002;112:983.
Pienaar S, et al. X-linked Hyper IgM (HIGM1) in an African kindred: The first report from South Africa. BMC Pediatr. 2003;3:12.
Puck J. Primary immunodeficiency diseases. JAMA. 1997;278:1835.
Reisner Y. ICOS: a new important player in BMT. Blood. 2005;105:3006.
Reith W, Mach B. The bare lymphocyte syndrome and the regulation of MHC expression. Ann Rev Immunol. 2001;19:331.
Ryuta N, et al. X-linked ectodermal dysplasia and immunodeficiency caused by reversion mosaicism of NEMO reveals a critical role for NEMO in human T cell development and/or survival. Blood. 2004;103:4565.
Sabroe I, et al. Toll-like receptors in health and disease: Complex questions remain. J Immunol. 2003;171:1630.
Sempowski GD, Haynes BF. Immune reconstitution in patients with HIV infection. Ann Rev Med. 2002;53:269.
Simonte SJ, Cunningham-Rundles C. Update on primary immunodeficiency: Defects of lymphocytes. Clin Immunol. 2003;109:109.
Smahi A, et al. The NFκB signaling pathway in human diseases: from incontinentia pigmenti to ectodermal dysplasias and immune-deficiency syndromes. Hum Mol Genet. 2002;11:2371.
Spearman P. HIV vaccine development: Lessons from the past and promise for the future. Curr HIV Res. 2003;1:101.
Speth C, et al. The role of complement in invasive fungal infections. Mycoses. 2004;47:93.
Su SV, Gurney KB, Lee B. Sugar and spice: Viral envelope-DC-SIGN interactions in HIV pathogenesis. Curr HIV Res. 2003;1:87.
Takada H, et al. Female agammaglobulinemia due to the Bruton tyrosine kinase deficiency caused by extremely skewed X-chromosome inactivation. Blood. 2004;103:185.
Takeda K, Kaiho T, Akira S. Toll-like receptors. Annu Rev Immunol. 2003;21:335.
Vasselon T, Detmers PA. Toll receptors: A central element in innate immune responses. Infect Immun. 2002;70:1033.
Villa A, et al. V(D)J recombination defects in lymphocytes due to RAG mutations: Severe immunodeficiency with a spectrum of clinical presentations. Blood. 2001;97:81-88.
Volberding PA. Initiating HIV therapy: Timing is critical, controversial. Postgrad Med. 2004;115:15.
Walport MJ. Complement at the interface between innate and adaptive immunity: I. N Engl J Med. 2001;344:1058.
Walport MJ. Complement at the interface between innate and adaptive immunity: II. N Engl J Med. 2001;344:1140.
Wehrle-Haller B, Imhof BA. Integrin-dependent pathologies. J Pathol. 2003;4:481.
Wen L, Atkinson JP, Gicias PC. Clinical and laboratory evaluation of complement deficiency. J Allergy Clin Immunol. 2004;113:585.
Winkelstein JA, et al. The X-linked hyper-IgM syndrome: Clinical and immunologic features of 79 patients. Medicine (Baltimore). 2003;82:373.
Wolf D, et al. HIV Nef associated PAK and PI3-kinases stimulate Akt-independent Bad-phosphorylation to induce anti-apoptotic signals. Nat Med. 2001;7:1217.
Yang OO. CTL ontogeny and viral escape: Implications for HIV-1 vaccine design. Trends Immunol. 2004;25:138.