CASE 129
History: A 26-year-old man presents with dyspepsia. A liver abnormality is noted on ultrasound.
1. What should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What type of hepatoma occurs in young adults?
3. What conditions predispose an individual to develop fibrolamellar hepatoma?
4. Which of the following statements regarding imaging of fibrolamellar hepatoma is true?
B. On CT, the central scar is best seen during the arterial phase scan.
C. On MRI, the central scar is usually hypointense on all sequences.
D. Scanning with 99mTc–labeled sulfur colloid, the tumor often exhibits uptake.
ANSWERS
CASE 129
Fibrolamellar Hepatoma
1. B, C, D, and E
2. C
3. D
4. C
References
McLarney JK, Rucker PT, Bender GN, et al: Fibrolamellar carcinoma of the liver: radiologic-pathologic correlation. Radiographics. 1999;19(2):453–471.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 196.
Comment
Neoplasms of the liver in young patients can be caused by several different cell types. The most commonly encountered are FNH and hepatic adenoma. Hemangiomas and metastases also must be considered. The appearance of this tumor in conjunction with a central scar or low-density areas is suggestive of FNH, but this appearance also can occur in other conditions.
Fibrolamellar carcinoma is an unusual variant of conventional hepatocellular carcinoma seen almost exclusively in younger patients. Also, the usual predisposing factors associated with hepatocellular carcinoma, such as cirrhosis or long-standing hepatitis, are not associated with fibrolamellar carcinoma. The development of fibrolamellar hepatoma is not believed to be associated with any etiologic risk factors, but this possibility must be a strong consideration when liver masses are encountered in a young adult.
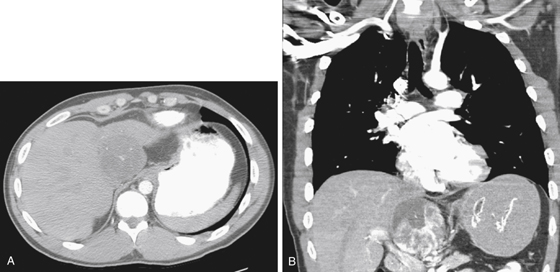
The radiologic diagnosis can be difficult to make because the lesion may resemble other liver tumors. It typically has a central “scar” or area of fibrous or necrotic tissue that can resemble FNH in its appearance. Fibrolamellar hepatoma does calcify, as in this case, and has been described in 50% of patients (see figures). On CT scans, the tumor is often hypodense, particularly its central scar. However, delayed images show increasing homogeneity or enhancement of the lesion with the surrounding liver, simulating a hemangioma. A poorly performed CT scan may underestimate the size of the lesion. Nuclear scanning may help differentiate the mass from FNH because fibrolamellar hepatoma does not have Kupffer cells.
The prognosis for patients with fibrolamellar hepatoma is much better than the prognosis for patients with hepatocellular carcinoma, and the lesion is potentially curable with surgery. Vascular invasion and other abnormalities of hepatocellular carcinoma are much less common in fibrolamellar hepatoma. This lesion also responds well to chemotherapy.







