CHAPTER 128
Diabetic Foot and Peripheral Arterial Disease
Definition
The incidence of lower limb amputations due to vascular disease has increased in the United States by approximately 20% during the last decade, disproportionately in minorities [1]. Persons with diabetes mellitus and peripheral vascular disease should be identified and prophylactic foot education and preventive care instituted to reduce the risk of limb loss [2].
Diabetes mellitus, a multisystem disease, causes two conditions that place the foot at high risk for amputation: polyneuropathy and peripheral arterial disease (PAD). Diabetes affects about 25.8 million Americans [3]. Diabetes is also on the rise in the United States, particularly in African American and Hispanic populations [4]. Data from the Framingham Heart Study [5] revealed that 20% of symptomatic patients with PAD had diabetes, but the true prevalence of PAD in patients with diabetes has been difficult to determine as most patients are asymptomatic, many do not report their symptoms, screening modalities have not uniformly been agreed on, and pain perception may be blunted by the presence of peripheral neuropathy [6].
Risk factors for diabetic ulcers include male sex, hyperglycemia, and diabetes duration. Foot ulcers often result from severe macrovascular disease, and diabetic neuropathy exacerbates the risk [7]. More than 60% of nontraumatic lower limb amputations occur in people with diabetes, underscoring the need to prevent foot ulcers and subsequent limb loss [8]. Multidisciplinary clinics that identify and manage patients with at-risk feet have demonstrated impressive reductions of 44% to 85% in the incidence of foot ulcers and lower limb amputations [9]. Minor foot trauma in a person with poor underlying circulation and reduced sensation can lead to skin ulceration. Skin ulcers, if they fail to heal, may lead to gangrene and progress to a point such that an amputation becomes necessary. This sequence of events can often be prevented before it starts.
Numerous studies have further shown that attention to lifestyle modification can dramatically reduce progression to type 2 diabetes [10]. The importance of identifying and treating a core set of risk factors (prediabetes, hypertension, smoking, dyslipidemia, and obesity) cannot be overstated [11].
Atherosclerosis is a vascular disease that can involve the peripheral arterial system. PAD is underdiagnosed, undertreated, and increasing in prevalence [12]. The American Heart Association estimates that 8 to 12 million Americans have PAD and that nearly 75% of them are asymptomatic. Annually, approximately 1 million Americans develop symptomatic PAD [13]. Despite its association with other cardiovascular risks including stroke and heart disease, only 25% of Americans with PAD are undergoing active treatment [14]. Major risk factors associated with the development of PAD or that accelerate its progression are high plasma cholesterol and lipoprotein levels, cigarette smoking, hypertension, diabetes, hyperhomocysteinemia, older age, positive family history, and chronic kidney disease [15–17]. African American ethnicity is a strong and independent risk factor for PAD [8]. Hypertension is an important risk factor for PAD, conferring a twofold to threefold increased risk for development of PAD [18]. The risk of PAD is increased two to four times by diabetes [19]. Given that men have more risk factors for PAD, they are more commonly affected than women are.
Symptoms
The patient with a diabetic foot may demonstrate no symptoms because peripheral neuropathy can result in a lack of sensation. Peripheral neuropathy can mask painful ulcers and ischemic skin. Foot collapse due to Charcot joints can progress asymptomatically. Alternatively, diabetic patients can have pain sensations in the feet from sensory polyneuropathy, including burning, tingling, and painful numbness. Because of impaired sensation, patients may report imbalance and falls.
Persons with PAD have claudication pain with walking because of insufficient arterial blood supply to meet the demand of exercising muscles. Pain with vascular claudication is typically in the calf, worsened with ambulation and relieved by resting [20]. Symptoms of pain, ache, or cramp with walking can also occur in the buttock, hip, thigh, or calf [20]. Patients with neurogenic claudication due to spinal stenosis can have similar leg or calf pain with walking but must bend at the waist or sit to relieve the symptoms. Persons may present with gangrene, ischemic ulcers on the distal foot, or, when PAD is severe, pain at rest.
Physical Examination
In addition to a standard physical examination, special neurovascular areas must be highlighted [21].
Inspect the skin for ulcerations, cracks, callus, or trophic changes (thin, shiny skin; distal hair loss).
Evaluate for any foot deformities that predispose it to abnormal stress distribution. These include hammer toes, collapsed foot arches due to Charcot joints, high-arch feet due to intrinsic muscle atrophy from polyneuropathy, and changes in stress distribution from previous toe or ray amputations.
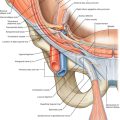
Assess distal pulses, particularly dorsalis pedis and posterior tibial. If they are absent or weak, it suggests the need for further testing for vascular integrity.
Assess sensation because persons with loss of protective sensation are at risk for skin ulceration. The instrument most frequently used for detection of neuropathy is the nylon Semmes-Weinstein monofilament. Inability to perceive the 10-g force applied by a 5.07 monofilament is associated with clinically significant large-fiber neuropathy [22].
Evaluate gait and balance. Peripheral neuropathy predisposes to falls and skin trauma. Probe any ulcers with sterile cotton-tipped applicators or surgical instruments. If bone is reached, this identifies persons with osteomyelitis, and other special bone imaging is unnecessary [23]. Assess shoes for uneven wear patterns, areas of breakdown, and width of the toe box.
Assess skin for redness and pressure points.
Functional Limitations
Persons with diabetes can develop peripheral polyneuropathy with loss of position sense and weakness. These can lead to gait instability and falls. Persons with PAD are often limited in community ambulation and vocational activities because of pain from claudication.
Diagnostic Studies
There are many noninvasive and invasive tests for PAD that are beyond the scope of this discussion. Angiography can identify surgically remediable lesions.
In the outpatient setting, the ankle-brachial index, a ratio of Doppler-recorded systolic pressures in the lower and upper extremities, is a convenient, accurate, noninvasive test that provides objective assessment of lower limb vascular status for screening and diagnosis of PAD [24]. Based on the results of the Ankle Brachial Index Collaboration, values above 1.40 indicate noncompressible arteries. Normal values are 1.00 to 1.40; borderline, 0.91 to 0.99; and abnormal, 0.90 or less [25]. The American College of Cardiology Foundation and American Heart Association Task Force on Practice Guidelines recommend resting ankle-brachial index to establish the diagnosis of lower extremity PAD in patients with exertional leg symptoms, nonhealing wounds, and age 65 years and older or 50 years and older with a history of smoking or diabetes [25]. Measurement of systolic pressure in the foot also provides a measure of arterial integrity.
Transcutaneous oximetry is the best method for assessment of cutaneous ischemia [9]. Transcutaneous oximetry pressures of more than 40 mm Hg are normal; pressures of 20 to 40 mm Hg indicate moderate disease, and potential for healing of a skin ulcer is less likely. With pressures below 20 mm Hg, severe skin ischemia is present, and skin healing is poor.
Systolic blood pressures in the foot are also helpful in quantifying the severity of ischemia. Persons with ischemic ulcers and ankle systolic pressures of less than 40 to 60 mm Hg are considered to have severe ischemia. Persons with persistently recurring ischemic rest pain and ankle systolic pressures of 50 mm Hg or less are severely involved [9].
If a person complains of numbness in the legs or feet or has low back pain, electrodiagnostic testing should be conducted to identify whether peripheral polyneuropathy is present or whether lumbosacral radiculopathy is responsible for these symptoms. Nerve conduction study findings may include reduced sensory and motor amplitude, latencies, and slowed conduction velocity. Electromyographic findings in radiculopathy include increased insertional activity, abnormal spontaneous activity, and changes in motor unit morphology; when these electromyographic findings are seen in a myotomal pattern, this suggests radiculopathy.
Treatment
Initial
Efforts to achieve smoking cessation are recommended for individuals with lower extremity PAD. Cigarette smoking is the most important risk factor for development of PAD [26]. Observational studies have demonstrated that the risk of death, myocardial infarction, and amputation is substantially greater in those individuals with PAD who continue to smoke [25]. The risk of smoking for vascular disease is even greater for women than for men [27].
For diabetes control, minimize hyperglycemia. The presence of PAD is 20% to 30% higher in diabetics than in the general population. According to recently published guidelines, patients with diabetes and PAD should have aggressive control of blood glucose levels with a hemoglobin A1c level below 7.0% or as close to 6% as possible to reduce the risk of microvascular complications [25].
For hypertension control, management of blood pressure is required. The desired blood pressure range is less than 140/90 mm Hg or less than 130/80 mm Hg if diabetes or renal insufficiency is present [12]. Choice of antihypertensive medication is generally guided by the presence of underlying diseases, such as diabetes, chronic kidney disease, or proteinuria [12].
Elevated total and low-density lipoprotein cholesterol levels, reduced high-density lipoprotein level, and hypertriglyceridemia are associated with lower extremity PAD [20]. Several clinical trials have demonstrated the benefits of lipid-lowering therapy in patients with PAD and coexistent coronary and cerebral arterial disease [15].
High serum homocysteine levels are associated with a twofold to threefold increased risk for PAD [28]. Dietary supplementation with B vitamins and folate may lower homocysteine levels, but no controlled trials to date demonstrate this clinical benefit in PAD [15].
Aerobic exercise can improve lipid profiles and optimize weight, blood pressure, and glycemic control, thus playing a role in medical management of PAD.
The 2012 American College of Chest Physicians Evidence-Based Clinical Practice Guidelines for antithrombotic therapy and prevention of thrombosis recommend aspirin, 75 to 100 mg/day, for individuals with asymptomatic PAD for the primary prevention of cardiovascular events. For secondary prevention of cardiovascular disease in patients with symptomatic PAD, long-term aspirin, 75 to 100 mg/day, or clopidogrel, 75 mg/day, is recommended [29]. Warfarin is not recommended. For patients with refractory claudication despite exercise therapy and smoking cessation, cilostazol, 100 mg twice daily, is recommended in addition to aspirin, 75 to 100 mg/day, or clopidogrel, 75 mg/day [29] (Table 128.1).
Rehabilitation
Exercise
Patients with symptomatic PAD have impaired walking tolerance. A program of supervised exercise is recommended for patients with intermittent claudication. A meta-analysis of training programs concluded that supervised exercise therapy showed statistically significant and clinically relevant differences in improvement of maximal treadmill walking distance compared with nonsupervised exercise therapy regimens of approximately 150 meters [30]. A study comparing the efficacy of cycle training versus treadmill exercise in the treatment of intermittent claudication concluded that cycle exercise is not effective in improving walking performance in all claudication patients [31]. A cross-transfer effect between training modes was noted for patients reporting common limiting symptoms at baseline for both cycling and walking. Therefore, the current recommendation for exercise in intermittent claudication is walking [31]. Exercise should be performed for a minimum of 30 to 45 minutes, at least three times per week. Supervised exercise can induce increases in maximal walking ability that exceed those attained with drug therapies alone and translate into improved functional ability [26,32]. Exercise is contraindicated in the presence of an ischemic ulcer or rest pain.
Foot Care
Meticulous attention to the feet by both patient and physician and detailed education of the patient are the mainstays of preventive foot care. Deformities should prompt the clinician to consider custom shoe inserts to distribute pressures evenly over the foot. Extra-depth shoes may be necessary to accommodate hammer toes. Extra-width shoes can accommodate bunions and other foot deformities. Sneakers may be another alternative for persons with or without mild foot deformities. However, if there are any aberrations in foot bone architecture, custom footwear with molded sole inserts is desirable. Gentle rocker-bottom modifications affect weight transfer from heel to toe during the gait cycle.
Skin Ulcers
Early treatment of skin infections with antibiotics is warranted along with minimization or elimination of weight bearing during healing. Achievement of a therapeutic antibiotic concentration at the site of infection is key. Intravenous antibiotics may therefore be necessary for patients with severe infection or systemic illness and for treatment of pathogens that are not susceptible to oral agents [33].
For more involved wounds, débridement with dressing changes or whirlpool is sometimes necessary. Deep infections into bone or infections that extend along fascial planes require débridement. If osteomyelitis is suspected, at least a 6-week course of parenteral or oral antibiotic therapy guided by culture samples obtained during débridement is an effective clinical approach. Other wound care measures, such as total contact casting, can assist with improved healing of plantar surface ulcers [34]. However, when both PAD and infection are present or the patient has a heel ulcer, outcome is poor and alternative strategies should be sought [34].
Hyperbaric oxygen therapy may improve wound healing and reduce the rate of amputation [35]. However, given its expense and limited resource, it is mostly limited to deep infections unresponsive to standard therapy.
Edema hinders wound healing. Measures to control edema, such as leg elevation, compression stockings, and pneumatic compression devices, are often used [36].
Procedures
An acute painful, pale, pulseless limb should be evaluated emergently as this indicates acute arterial compromise. Likewise, gangrene or an ulcer extending to bone should prompt surgical consultation. Sharp débridement for a necrotic wound is often necessary to remove devitalized tissue and to promote healing of ulcers.
Percutaneous endovascular interventions to treat peripheral arterial occlusion include transluminal angioplasty with balloon dilation, stents, atherectomy, laser, cutting balloons, thermal angioplasty, and fibrinolysis or fibrinectomy. This intervention may be necessary to provide enough oxygenated arterial blood to a limb to heal open sores, to improve symptoms of claudication, or to save an extremity at risk for amputation [22].
Endovascular procedures are indicated for individuals with severe vocational or lifestyle-limiting disability due to intermittent claudication for whom exercise and pharmacologic therapy have failed. Clinical features must suggest a reasonable likelihood of symptomatic improvement with endovascular intervention with a favorable risk-benefit ratio [25].
Outcomes of percutaneous transluminal angioplasty and stents depend on anatomic and clinical factors. Durability of patency after percutaneous transluminal angioplasty is greatest for lesions in the common iliac artery and decreases distally. Durability decreases with increasing length of the stenosis, multiple and diffuse lesions, poor-quality runoff, diabetes, renal failure, and smoking. Hormone replacement in women has been shown to decrease patency of iliac stents [25].
Surgery
Surgical treatment of intermittent claudication is indicated in individuals who do not derive adequate functional benefit from nonsurgical therapies, who have limb arterial anatomy favorable to a durable clinical result, and in whom the risk of cardiovascular complications is low.
The exact surgical procedure (aortobifemoral bypass, aortoiliac bypass, iliofemoral bypass, axillofemoral-femoral bypass) is determined by the site and severity of the occlusive lesion, prior revascularization attempts, general medical condition, and desired outcome [25].
Similar considerations are given in the management of limb-threatening ischemia. Surgical lower limb amputation may be necessary if revascularization attempts are unsuccessful in the management of limb-threatening ischemia or gangrene.
Potential Disease Complications
As a result of PAD, patients may develop ischemic pain from arterial insufficiency defined as claudication (pain with ambulation) or rest pain. Other potential complications include nonhealing or slow to heal foot ulcers, cellulitis, and deeper wound infections in the foot. If those complications cannot be treated medically, amputation of a portion of the lower limb may be necessary to save the remaining viable limb and to prevent disseminated infection. Charcot joints and bone fractures in the foot due to diabetic polyneuropathy can be seen, potentially leading to skin ulcer and breakdown.
Potential Treatment Complications
Potential treatment complications depend on the intervention implemented. For example, in surgical revascularization, infection of arterial bypass grafts, ischemic cardiac disease, and worsening of renal azotemia are potential complications. Patients undergoing wound débridement should be closely observed for possible infection of foot ulcers after débridement. For PAD patients initiating an exercise program, potential complications include cardiac ischemic events, given the strong correlation of arterial disease and cardiovascular disease. Therefore, in such patients, supervised exercise instruction after cardiac stress testing is initially recommended to stratify patients at potential risk.